Abstract
In fetus, the reproductive tract consists of two parts, one male (Wolffian duct) and one female (Mullerian duct), and during embryogenesis, because of hormonal influence, the Mullerian duct system develops to form female genital tract, while the Wolffian duct system regresses and may eventually disappear. Gartner’s cysts arise from the remnant of mesonephric duct (Wolffian duct) and appear only in approximately 1–2% of the population. They are mostly asymptomatic and small but sometimes can be bigger. Here we report a unique case of a large Gartner’s cyst in the posterior vaginal wall with symptoms of dyspareunia and voiding disturbances. After examination, she was diagnosed with vaginal cyst and complete excision was done and confirmed as a mesonephric benign cyst (Gartner’s cyst).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gartner’s duct cyst is a benign vaginal cyst that originates from the vestigial remnant of the mesonephric duct (Wolffian duct) in females [1, 2]. Occasionally, a part of this Wolffian system remains and in these cases, the duct is located mainly between the vagina and cervix [3]. Most Gartner’s cysts are small (< 3 cm), asymptomatic, usually paravaginal, and in the anterolateral position; however, they can be large and cause urethral or even ureteric obstruction [4]. Its chances of being present in the posterior vaginal wall are relatively rare [5]. Gartner’s cysts arise only in approximately 1–2% of the population. Here we report a case of a large Gartner’s cyst in the posterior vaginal wall with symptoms of dyspareunia and voiding disturbances.
Case Report
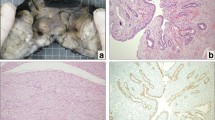
A 41-year-old female (Obst H/O - para 2 with previous 2 normal vaginal deliveries, with last childbirth 11 years back) presented to our gynaecological outpatient department with complaints of chronic pelvic pain and dyspareunia. Patient also gave a history of difficulty in passing urine. No other history of any menstrual irregularity or any kind of vaginal discharge. During a routine gynaecological examination, found to have a large cystic swelling arising from the posterior vaginal wall and growing up to labia majora introitus (whitish in colour, non-transilluminant and flaccid on touch, Fig. 1). Upon speculum examination, the cervix was found to be hypertrophied with erosion over anterior lip. Sonography of the whole abdomen with TVS showed small hypoehoic cyst at the vagina (measuring 37 × 35 × 30 mm, vol 20 cc) with small nabothian follicle at the cervix (8 × 8mm), and uterus size and shape was found to be normal with ovaries apparently normal. Pap smear showed features of atrophic vaginitis with candidiasis. Her laboratory routine blood investigations and urinalysis were normal.
The differential diagnosis could include rectocele (which was ruled out by clinical examination, as cough impulse was negative), inclusion cyst of vagina (which is usually found at the lower end of the posterior vaginal wall) and Gartner’s duct cyst (which is usually located in the anterolateral vaginal wall and rarely posterior wall). In this case, the provisional diagnosis of Gartner’s duct cyst was made in view of patient clinical presenting picture (i.e. dyspareunia with history of difficulty in passing urine) and its appearance on local examination (i.e. cystic lesion which was non-transilluminant and flaccid on touch).
The patient was then planned for elective surgical excision. Under general anaesthesia, an encircling incision was given and then by sharp and blunt dissection excision of the vaginal cyst was done followed by repair of posterior vaginal wall transversally with absorbable sutures (Fig. 2).
Post-operative course was uneventful, and the patient was discharged in a stable condition on the 2nd post-operative day. The patient was followed up after 1 week, and she did not have any complaints.
Excised cystic tissue (measuring 5 × 3 × 3 cm) was sent for histopathology (Fig. 3) which showed solid cystic lesion filled with jelly-like material and section showed vaginal cyst lined by layer of low cuboidal epithelium showing reactive change along with stratified squamous epithelium with no signs of dysplasia and stroma shows fibrocollagenous tissue which is consistent with mesopnephric benign cyst (Gartner’s duct cyst).
Discussion
Mullerian and mesonephric duct derivatives tend to be located along the anterolateral aspect of the vagina but can be found almost at any location within the vaginal walls. Classically, Gartner’s cyst (mesonephric cyst) are solitary, are S-shaped unilateral about 2 cm in diameter, and are located in the antero-lateral vaginal wall of the proximal one-third of the vagina [6]. But in this case, a quite large cyst about 5 × 3 × 3 cm in the posterior vaginal wall was seen.
Gartner’s duct cyst is usually asymptomatic and small in size, and there were no definite risk factors identified for it. However, they may occur due to some factors such as trauma to the vagina during childbirth or invasive procedures involving female genital tract, and sometimes, these risk factors increase one’s chances of getting a condition compared to an individual without the risk factor. In this case, the patient was asymptomatic and feeling heaviness and discomfort in the vaginal region after TVS.
Only in exceptionally rare and few isolated cases, there has been a malignant transformation reported [7]. Hence, surgical excision is the mainstay of treatment if they are symptomatic and large. Diagnosis is confirmed with histopathology which shows cyst lined by low cuboidal epithelium showing reactive change along with stratified squamous epithelium.
Learning Points
-
A large Gartner’s cyst in the posterior wall is a rare medical condition.
-
Surgical excision of a large cyst is the mainstay of treatment to avoid malignant transformation of cyst later on.
-
Surgical excision should be done carefully to avoid injury to adjoining structures and rectum.
-
While repairing the posterior vaginal wall, the important point to be kept in mind is maintaining the length of the vaginal canal for coitus post-surgically.
References
Hoogendam JP, Smink M (April 2017) Gartner’s duct cyst. N Engl J Med 376(14):e27. https://doi.org/10.1056/NEJMicm1609983
Tiwari C, Shah H, Desale J, Waghmare M (2017) Neonatal gartner duct cyst: two case reports and literature review. Dev Period Med 21(1):35–37
Siegelman ES, Outwater EK, Banner MP, Ramchandani P, Anderson TL, Schnall MD (1997) High resolution MR imaging of the vagina. Radiographics 17:1183–1203
Akinbiyi AA, Suchet I (2008) Symptomatic giant gartner’s duct cyst of the vagina. J Gynecol Surg 24(2)
Kondi-Pafiti A, Grapsa D, Papakonstantinou K, Kairi-Vassilatou E, Xasiakos D (2008) Vaginal cysts: a common pathologic entity revisited. Clin Exp Obstet Gynecol 35:41–44
Pradhan S, Toban H (2009) Vaginal cysts : a clinopathological study of 41 casses. J Gynecol Surg 24(75)
Bats A-S, Metzger U, Le Frere-Belda M-A, Brisa M, Lecuru F (2009) Malignant transformation of Gartner’s cyst. Int J Gynecol Cancer 19(9):1655–1657
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khetarpal, S., Khetarpal, A. Gartner’s Duct Cyst (Mesonephric Cyst) in Posterior Vaginal Wall. Indian J Surg 84, 203–205 (2022). https://doi.org/10.1007/s12262-021-02791-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-021-02791-5