Abstract
The aim of this study is to compare the recurrence rates with different modalities used as first-line treatment for first-episode primary spontaneous pneumothorax, and investigated the risk factors for recurrence. We retrospectively reviewed consecutive patients under 60 years of age who were treated for a first episode of primary spontaneous pneumothorax between May 1996 and May 2016 at our hospital. The patients were divided into 6 groups according to the treatment received. A total of 667 patients with 890 episodes of primary spontaneous pneumothorax were included in the analysis. The median follow-up period was 64.5 months. The recurrence rate in the 6 groups was as follows: observation, 52.5% (21/40); chest tube drainage, 32.6% (84/258); aspiration, 100% (42/42); axillary thoracotomy, 8.8% (9/102); 2-port video-assisted thoracoscopic surgery (VATS), 6.0% (7/117); and 3-port VATS, 10.6% (11/108). The recurrence rate was higher in non-surgery groups than in surgery groups (147/340 vs 27/327, P < 0.01). Pneumothorax size (odds ratio [OR] = 0.252, P = 0.017) and duration of chest tube drainage (OR = 0.687, P = 0.001) were independent risk factors for ipsilateral recurrence. In the management of first-episode primary spontaneous pneumothorax, the recurrence rate was higher in patients who were treated with conservative procedures as compared with surgery. Pneumothorax size and duration of chest tube drainage were risk factors for recurrence after initial treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary spontaneous pneumothorax (PSP) is a common clinical problem that affects young healthy people without any obvious precipitating factors, with reported annual incidences of 7.4–18 and 1.2–6 per 100,000 population in males and females, respectively [1]. There is no consensus on the management of the first PSP episode; observation, simple aspiration, and chest tube drainage (CTD) are the most frequently used approaches, with a recurrence rate at 1 year of 30% (range, 16–52%) [2]. Based on the development of new techniques and instruments and findings on the pathogenesis and mechanisms of PSP recurrence, surgery (either thoracotomy or video-assisted thoracoscopic surgery [VATS]) has been applied to the treatment of first-episode PSP [3, 4], but recurrence rates associated with these approaches have not been investigated in detail. To this end, the present study compared recurrence rates for different modalities used for treatment of first-episode PSP including observation, simple aspiration, CTD, axillary thoracotomy (AT), and VATS with 2 or 3 ports and examined risk factors for recurrence after initial management.
Methods
Patients
Medical records of 667 patients with first-episode PSP who were treated by different modalities at our hospital between May 1996 and May 2016 were retrospectively reviewed. The study was approved by the Institutional Review Board of the Second Affiliated Hospital of Kunming Medical University. As there was no outpatient care available, all PSP patients were hospitalized and their information recorded in a database. PSP was diagnosed as J93.101 according to the International Classification of Diseases-10. Exclusion criteria were age > 60 years old, second spontaneous pneumothorax (including pneumothorax caused by tuberculosis, lung cancer, chronic obstructive pulmonary disease, pneumoconiosis, trauma, lymphangioleiomyoma, or endometriosis), and receipt of treatment prior to admission to our hospital. Contralateral recurrence within the follow-up period was considered as a new case. The endpoint of follow-up was the first ipsilateral recurrence.
Modalities for the Treatment
The 667 patients were divided into the following 6 groups according to the treatment they received: observation, simple aspiration, CTD, AT, VATS with 2 ports, and VATS with 3 ports. CTD involved insertion of a 24F or 28F chest tube into the 2nd or 3rd anterior intercostal space at the mid-clavicular line under local anesthesia, with closed underwater seal drainage. Before VATS was widely adopted at our hospital, we used AT, in which a 5-cm incision was made toward the anterior-inferior axillary region, and mini-thoracotomy was performed through the 3rd or 4th intercostal space; the thorax was then explored and adhesions separated, and pulmonary ruptures or bullae were repaired or removed. For bullae < 3 cm in diameter, the bottom was ligated with silk thread, while larger bullae were directly resected with continuous suturing applied to prevent air leakage. VATS with 2 ports was performed under general anesthesia with single lung ventilation. A 10-mm port was placed in the 8th intercostal space at the mid-axillary line through which a thoracoscope was introduced; a 15-mm port was then placed in the 4th intercostal space on the anterior axillary line, and hemostasis and separation of adhesion were performed under thoracoscopy. After determining the specific location of bullae, wedge resection was performed with a linear cutting suture, and a single intercostal tube was inserted after the operation. For VATS with 3 thoracoscopic ports, a 10-mm port was placed in the 8th intercostal space at the mid-axillary line, through which a thoracoscope was introduced; a 10-mm port was placed in the 5th intercostal space at the posterior axillary line; and a 15-mm port was placed in the 4th intercostal space at the anterior axillary line. The other steps of the procedure were the same as for VATS with 2 ports, except that 2 intercostal tubes were inserted after the operation. We classified observation, simple aspiration, and CTD as non-surgery groups and referred to them as conservative treatment; the remaining three groups were surgery groups, collectively referred to as surgical treatment. Indications for surgery included persistent air leakage (> 4 days) (116 cases, 35.6%), tension pneumothorax (35 cases, 10.6%), hemopneumothorax (37 cases, 11.4%), and bullae observed by chest X-ray or chest computed tomography (CT) (139 cases, 42.4%). Pleurodesis was most often performed with 10% povidone-iodine-soaked gauze or by simple mechanical pleural abrasion in some patients. Pneumothorax size was calculated as a percentage as previously described [5].
Statistical Analysis
Statistical analysis was performed using SPSS for Windows v22.0 (SPSS Inc., Chicago, IL, USA). Data are presented as median (range) and number (percentage) unless otherwise stated. One-way analysis of variance was used to evaluate continuous variables, and the nonparametric test was used to compare categorical variables. Uni- and multivariate binary logistic regression was used to examine associations between treatment modalities and recurrence rates. The Kaplan-Meier curves were generated to visualize cumulative probabilities of recurrence, which were analyzed with the log-rank test. P values < 0.05 were considered statistically significant for all tests.
Results
Clinical and demographic information of patients is shown in Tables 1 and 2. A total of 667 cases with 890 episodes of PSP were reviewed (601 males and 66 females; median age, 27 years [range, 6–59 years]). Among the 667 patients, 240 (40.0%) were current smokers. All patients initially had chest or back pain, and 167 (25.0%) presented with significant dyspnea. The median follow-up was 64.5 months (range, 1–240 months), and median time from symptom onset to hospitalization was 65.5 h (range, 1–480 h). A total of 174/667 patients (26.1%) experienced recurrence. There were no significant differences in height, body weight, body mass index, sex ratio, location of pneumothorax, and interval to recurrence across the 6 groups. However, patients in the observation group were younger than those in any other group (P = 0.003), and patients in the aspiration group had the earliest admission to hospital after symptom onset, while those in the AT group had the latest admission (P < 0.001). Pneumothorax size was smaller in the observation and aspiration groups than in the other 4 groups, and duration of hospitalization was significantly longer in surgery groups than in non-surgery groups (P < 0.001). The number of patients with recurrence in each group was as follows: observation, 21 (52.5%); CTD, 84 (32.6%); aspiration, 42 (100%); AT, 9 (8.8%); VATS with 2 ports, 7 (6.0%); and VATS with 3 ports, 11 (10.6%). Recurrence rate varied across groups (χ2 = 181.12, P < 0.01); the rate was higher in non-surgery groups than in surgery groups (χ2 = 105.76, P < 0.01) (Fig. 1). Duration of tube drainage was shorter in the CTD group than in the AT and VATS groups (P ˂ 0.001).
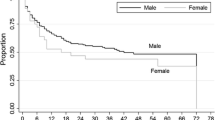
Sex, age, time from symptom onset to hospitalization, pneumothorax size, height, body weight, body mass index, location of pneumothorax, smoking history, treatment modality, duration of tube drainage, and pleurodesis history were included as variables in the logistic regression analysis of recurrence; and sex, time from symptom onset to hospitalization, pneumothorax size, treatment modality, and duration of tube drainage with a P value < 0.1 were included as variables in the multivariate logistic regression analysis (Table 3). We found that large pneumothorax size, non-surgical modality, and shorter duration of tube drainage were risk factors for recurrence after the first episode of PSP (P = 0.017, P < 0.001, and P = 0.001, respectively). Mean recurrence-free survival times were as follows: observation, 78.8 months; CTD, 141.4 months; aspiration, 31.9 months; AT, 159.4 months; VATS with 2 ports, 150.5 months; and VATS with 3 ports, 125.7 months (Fig. 2). Patients who were treated by surgical modalities had longer recurrence-free survival than those treated by non-surgical modalities (log-rank = 193.6, df = 5, P ˂ 0.001).
The Kaplan-Meier cumulative recurrence analysis demonstrating the effect of each initial treatment modality on the probability of recurrence. AT, axillary thoracotomy; CTD, chest tube drainage; VATS 2, video-assisted thoracoscopic surgery with 2 ports; VATS 3, video-assisted thoracoscopic surgery with 3 ports
Discussion
PSP is a common condition that affects many healthy young people. The average rate of recurrence is 30% [1, 2]. The optimal procedure for the treatment of first-episode PSP is debated; in general, conservative modalities such as observation or simple needle aspiration are used, and some authors have suggested that management depends on clinical symptoms and not pneumothorax size [3, 6, 7]. However, others recommend a more aggressive approach such as CTD for PSP > 20% of the hemithorax, irrespective of the symptoms [4, 8, 9]. There have been few studies comparing recurrence rates between conservative and surgical treatment modalities for the first episode of PSP. In this study, we analyzed different PSP treatment approaches according to symptom severity, pneumothorax size, and chest X-ray or CT findings and determined that for a smaller pneumothorax size (median, 27%; range 10–40%) and mild symptoms, observation and oxygen therapy yielded satisfactory outcomes, with a recurrence rate of 52.5% (21/40) after a median follow-up of 16.5 months (range, 10–70 months). For patients with larger pneumothorax size (median, 64%; range,10–100%) and obvious symptoms, CTD was employed, and the recurrence rate was 32.6% (84/258) after a median follow-up of 23.9 months (range, 1–240 months). In recent years, we have used simple needle aspiration as initial treatment in patients with moderate pneumothorax size (median, 48.3%; range, 35–90%) and obvious symptoms, with a recurrence rate 100% (42/42) after a median follow-up of 31.9 months (range, 1–240 months). The overall recurrence rate among patients who were not treated surgically was 43.2% (147/340), which is comparable with the previously reported rate of 54.7% [10, 11].
Although non-surgical approaches are preferred for initial treatment of first-episode PSP [12], the high recurrence rates are a concern. In another study with a shorter follow-up period, 52/164 patients required a second treatment after initial aspiration [4]. PSP patients treated with simple aspiration must meet strict criteria before they can be discharged, which is not always appropriate [6], especially for patients who live far from the hospital. We question the appropriateness of simple aspiration in the initial management of PSP; in some patients, it was more reasonable to select CTD [13]. Because of the high recurrence rate after non-surgical procedures and occurrence of air leakage resulting from ruptured bullae (3.6–73%), which is generally accepted as the cause of PSP [14], we have used surgery to treat first-episode PSP to reduce the risk of recurrence, especially in patients with a large-sized pneumothorax, severe symptoms, or bullae in the chest X-ray or CT scan and found that surgical options were appealing to patients. Our analyses showed that the recurrence rate was much lower after surgical procedures (AT or VATS) than after non-surgical procedures (27/327 vs 147/340, P < 0.01), while the duration of CTD and hospitalization were much longer. Before the refinement of minimally invasive technology, PSP patients who required surgery elected to undergo AT. With technologic advances, VATS has been increasingly performed at our hospital. At first, only VATS with 3 ports was carried out, but as surgeons’ proficiency with the technique improved, 2-port VATS was adopted. Both AT and VATS are the most frequently used modalities for PSP treatment, and in recent years, the latter has been the first choice for PSP patients who require surgery [15]. Studies comparing recurrence rate, pain following surgery, duration of hospitalization and CTD, and costs of thoracotomy and VATS found that the latter had certain advantages such as shorter length of hospital stay, less pain and analgesic usage, and better cosmetic outcome, while the former had a lower recurrence rate [16,17,18]. However, there is an ongoing debate concerning recurrence rates with the 2 procedures, with some evidence showing that with the development of more effective surgical techniques and instruments, VATS can achieve better outcomes [19]. AT allows a broad exploration of the thoracic cavity, which could permit the management of all defects; we used direct wedge resection of the apical segment or lobectomy and propylene sutures, which could prevent new bullae related to the staple line as has been reported with VATS using stapler lobectomy [20]. The choice of VATS with 2 vs 3 ports depends on the location of bullae, preferences of the patient and surgeon, and the surgeon’s proficiency. VATS as a first-line treatment for PSP offers patients a better clinical outcome and psychosocial advantages as they can quickly resume their normal living habits [4]. However, additional studies are needed to confirm the effectiveness and advantages of surgical modalities as initial treatment for PSP.
One of the most important aims of PSP management is to reduce the risk of recurrence. In this study, we explored the risk factors for PSP recurrence after different initial treatments in order to identify the most appropriate procedure. We found that pneumothorax size, duration of CTD, and treatment modality were 3 risk factors for recurrence. The recurrence rate increased with pneumothorax size (odds ratio [OR], 0.252; P = 0.017); this was calculated using the method of Kircher and Swartzel [5], which allows a more precise evaluation of PSP. Some studies have shown that the probabilities of ipsilateral recurrence and persistent air leakage were higher with larger as compared with small pneumothorax size [20], which is supported by our findings. A larger pneumothorax size was associated with a longer time for closure of the lung defect and may be a new indication for surgical treatment of PSP [20]. We also found that pneumothorax size was a risk factor for ipsilateral recurrence. Another risk factor was the duration of CTD (OR = 0.687, P = 0.001); in patients who underwent CTD irrespective of surgery, longer CTD duration was associated with a lower rate of recurrence. We used large-sized tubes (24Fr or 28Fr) for intercostal CTD; with re-expansion of the collapsed lung, there is greater inflammation of the pleura around the chest tube, which could lead to pleural symphysis caused by adhesion of the visceral and parietal pleura. A longer CTD duration could aggravate pleural inflammation and enhance pleural adhesion, thereby reducing the risk of recurrence. However, the predictive value of CTD duration for pneumothorax recurrence remains to be determined.
In contrast to other studies [11, 21, 22], we did not find any link between smoking or pleurodesis and PSP recurrence. Although PSP arises in patients without clinically apparent lung disease, almost 80%—including both smokers and non-smokers—exhibit emphysema-like changes such as bullae either by chest CT or by surgical examination [23]. As smoking can aggravate bronchiolitis and the rupture of bullae, it has been suggested as an independent predictive factor for risk of pneumothorax recurrence [7, 11, 21], but this was not the case in our study. The most likely reason for this finding is that some second-hand smokers in our patient pool were classified as nonsmokers but nonetheless experienced recurrence. In fact, PSP recurrence is multifactorial, and it is difficult to identify a single predictive factor. Pleurodesis is not a standard intraoperative procedure at our hospital. Although mechanical pleural abrasion is one of the most widely used techniques for pleurodesis, whether it reduces the risk of PSP recurrence is controversial [22]. Talc is used in many countries and is effective in reducing recurrence risk; however, we have never used this method as it can cause chest pain, fever, and occasionally serious complications such as anaphylactic shock. The pleural abrasion performed with 10% povidone/iodine-soaked gauze is a combination of physical and chemical methods, which induces an inflammatory response in pleura and facilitates its adhesion. Some studies found that thoracoscopic wedge resection of bullae successfully controlled PSP, but the additional pleural abrasion did not reduce pneumothorax recurrence rate [22].
Our study had several limitations. Firstly, its retrospective design and the fact that it was conducted at a single center may have resulted in patient selection bias. Secondly, because we have tended to use observation or simple aspiration to treat patients with small-sized pneumothorax and mild or moderate symptoms over the last 4 years, the follow-up period was much shorter in these 2 groups than in the other 4 groups, which may have limited the power of analysis. Thirdly, we examined specific surgical modalities for the treatment of first-episode PSP based on our experiences over many years, but the clinical value of surgery (thoracotomy or VATS) must be evaluated in randomized controlled trials with a larger cohort, as improvements in diagnostic imaging techniques and surgical procedures and instruments over the past 20 years are likely to influence outcomes.
Conclusions
This case series analysis of 667 patients of first-episode primary spontaneous pneumothorax has shown that both conservative and surgical treatments can be used in the management of first-episode primary spontaneous pneumothorax. However, the risk of recurrence was higher with the former approach. Another important finding from this study emerged that both pneumothorax size and chest tube drainage duration were risk factors for primary spontaneous pneumothorax recurrence after initial treatment, with larger pneumothorax size and longer chest tube drainage duration associated with higher and lower recurrence rates, respectively. Overall surgical treatments done by axillary thoracotomy or video-assisted thoracoscopic surgery were associated with much less recurrence of pneumothorax if employed as primary treatment. These findings provide a reference for surgeons when selecting the optimal treatment modality for a first episode of primary spontaneous pneumothorax to minimize the risk of recurrence and improve the long-term prognosis of patients.
References
Bobbio A, Dechartres A, Bouam S, Damotte D, Rabbat A, Régnard JF, Roche N, Alifano M (2015) Epidemiology of spontaneous pneumothorax: gender-related differences. Thorax 70(7):653–658. https://doi.org/10.1136/thoraxjnl-2014-206577
Huang TW, Lee SC, Cheng YL, Tzao C, Hsu HH, Chang H, Chen JC (2007) Contralateral recurrence of primary spontaneous pneumothorax. Chest 132(4):1146–1150. https://doi.org/10.1378/chest.06-2772
Tschopp JM, Rami-Porta R, Noppen M, Astoul P (2006) Management of spontaneous pneumothorax: state of the art. Eur Respir J 28(3):637–650. https://doi.org/10.1183/09031936.06.00014206
Divisi D, Di Leonardo G, Crisci R (2015) Video-assisted thoracic surgery versus pleural drainage in the management of the first episode of primary spontaneous pneumothorax. Am J Surg 210(1):68–73. https://doi.org/10.1016/j.amjsurg.2014.10.025
Kircher LT Jr, Swartzel RL (1954) Spontaneous pneumothorax and its treatment. J Am Med Assoc 155(1):24–29. https://doi.org/10.1001/jama.1954.03690190030009
Janssen J, Cardillo G (2011) Primary spontaneous pneumothorax: towards outpatient treatment and abandoning chest tube drainage. Respiration 82(2):201–203. https://doi.org/10.1159/000324268
Tschopp JM, Bintcliffe O, Astoul P, Canalis E, Driesen P, Janssen J, Krasnik M, Maskell N, Van Schil P, Tonia T, Waller DA, Marquette CH, Cardillo G (2015) ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J 46(2):321–335. https://doi.org/10.1183/09031936.00219214
Torresini G, Vaccarili M, Divisi D, Crisci R (2001) Is video-assisted thoracic surgery justified at first spontaneous pneumothorax? EurJ Cardiothorac Surg 20(1):42–45. https://doi.org/10.1016/s1010-7940(01)00679-0
Chou SH, Cheng YJ, Kao EL (2003) Is video-assisted thoracic surgery indicated in the first episode primary spontaneous pneumothorax? Interact Cardiovasc Thorac Surg 2(4):552–554. https://doi.org/10.1016/S1569-9293(03)00143-9
Hatz RA, Kaps MF, Meimarakis G, Loehe F, Müller C, Fürst H (2000) Long-term results after video-assisted thoracoscopic surgery for first-time and recurrent spontaneous pneumothorax. Ann Thorac Surg 70(1):253–257. https://doi.org/10.1016/s0003-4975(00)01411-9
Sadikot RT, Greene T, Meadows K, Arnold AG (1997) Recurrence of primary spontaneous pneumothorax. Thorax 52(9):805–809. https://doi.org/10.1136/thx.52.9.805
Henry M, Arnold T, Harvey J, Pleural Diseases Group, Standards of Care Committee, British Thoracic Society (2003) BTS guidelines for the management of spontaneous pneumothorax. Thorax 58(Suppl 2):ii39–ii52. https://doi.org/10.1136/thorax.58.suppl_2.ii39
Baumann MH, Strange C, Heffner JE, Light R, Kirby TJ, Klein J, Luketich JD, Panacek EA, Sahn SA, AACP Pneumothorax Consensus Group (2001) Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus Statement. Chest 119(2):590–602. https://doi.org/10.1378/chest.119.2.590
Laituri CA, Valusek PA, Rivard DC, Garey CL, Ostlie DJ, Snyder CL, St Peter SD (2011) The utility of computed tomography in the management of patients with spontaneous pneumothorax. J Pediatr Surg 46(8):1523–1525. https://doi.org/10.1016/j.jpedsurg.2011.01.002
Crisci R, Coloni GF (1996) Video-assisted thoracoscopic surgery versus thoracotomy for recurrent spontaneous pneumothorax. A comparison of results and costs. Eur J Cardiothorax Surg 10(7):556–560. https://doi.org/10.1016/s1010-7940(96)80424-6
Goto T, Kadota Y, Mori T, Yamashita S, Horio H, Nagayasu T, Iwasaki A (2015) Video-assisted thoracic surgery for pneumothorax: republication of a systematic review and a proposal by the guideline committee of the Japanese association for chest surgery 2014. Gen Thorac Cardiovasc Surg 63(1):8–13. https://doi.org/10.1007/s11748-014-0468-9
Tamura M, Shimizu Y, Hashizume Y (2013) Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 8:153. https://doi.org/10.1186/1749-8090-8-153
Barker A, Maratos EC, Edmonds L, Lim E (2007) Recurrence rates of video-assisted thoracoscopic versus open surgery in the prevention of recurrent pneumothoraces: a systematic review of randomised and non-randomised trials. Lancet 370(9584):329–335. https://doi.org/10.1016/S0140-6736(07)61163-5
Muramatsu T, Shimamura M, Furuichi M, Nishii T, Takeshita S, Ishimoto S, Morooka H, Tanaka Y, Yagasaki C, Ohmori K, Shiono M (2011) Cause and management of recurrent primary spontaneous pneumothorax after thoracoscopic stapler blebectomy. Asian J Surg 34(2):69–73. https://doi.org/10.1016/S1015-9584(11)60022-5
Sayar A, Kök A, Citak N, Metin M, Büyükkale S, Gürses A (2014) Size of pneumothorax can be a new indication for surgical treatment in primary spontaneous pneumothorax: a prospective study. Ann Thorac Cardiovasc Surg 20(3):192–197. https://doi.org/10.5761/atcs.oa.12.02212
Cheng YL, Huang TW, Lin CK, Lee SC, Tzao C, Chen JC, Chang H (2009) The impact of smoking in primary spontaneous pneumothorax. J Thorac Cardiovasc Surg 138(1):192–195. https://doi.org/10.1016/j.jtcvs.2008.12.019
Ling ZG, Wu YB, Ming MY, Cai SQ, Chen YQ (2015) The effect of pleural abrasion on the treatment of primary spontaneous pneumothorax: a systematic review of randomized controlled trials. PLoS One 10(6):e0127857. https://doi.org/10.1371/journal.pone.0127857
Haynes D, Baumann MH (2011) Pleural controversy: aetiology of pneumothorax. Respirology 16(4):604–610. https://doi.org/10.1111/j.1440-1843.2011.01968.x
Author information
Authors and Affiliations
Contributions
Weijiang Ma: Study design, project writing, and management, actually performing the study, viz., experiments, practical work, operative work, data acquisition, data analysis, statistical inferences, manuscript writing, and repeated editing and reviewing of the manuscript, Feng Ling: Conceptualization, study design, project writing and management, defining the study, extensive literature search, actually performing the study, viz., experiments, operative work, data acquisition, data analysis, statistical inferences, manuscript writing, and repeated editing and reviewing of the manuscript, Limin Yang: Conceptualization, study design, extensive literature search, data analysis, manuscript writing, and repeated editing and reviewing of the manuscript, Shaojun Yang: Conceptualization, study design, extensive literature search, experiments, data acquisition, data analysis, statistical inferences, Xu Li: Study design, project writing and management, defining the study, actually performing the study, Jianqiang Ma: Data acquisition, data analysis, statistical inferences, Jia Liu: Experiments, data acquisition
Corresponding author
Ethics declarations
All authors contributed substantially to this study. The institution from where the article comes is a guarantor of the content. The study was approved by the Institutional Review Board of the Second Affiliated Hospital of Kunming Medical University.
Conflict of Interest
The authors declared no conflicts of interest concerning the authorship and /or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ma, W., Ling, F., Yang, L. et al. Primary Spontaneous Pneumothorax—Outcomes of Different Treatment Modalities. Indian J Surg 83, 645–651 (2021). https://doi.org/10.1007/s12262-020-02408-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02408-3





