Abstract
Laparoscopic cholecystectomy (LC) has been widely performed for gallbladder disease. However, it has potential fatal complications such as vasculo-biliary injury, which are related to inexperience. Therefore, surgical training of surgical residents in safe and accurate LC technique is important. The aim of this study was to investigate the personal learning curve of one resident and to confirm the safety of LC performed by a surgical resident. We retrospectively reviewed 151 patients who underwent LC performed by a single surgical resident at Hanyang University Hospital. Three or four trocars were inserted, and the “critical view of safety (CVS)” was established in all patients. All procedures were supervised by an experienced hepatobiliary and pancreatic surgeon. Of a total 428 LCs during the study period, 151 were performed by a single surgical resident. There were no significant differences between Group A, the surgical resident, and Group B, the experienced surgeon, in open conversion rate (0.7% vs. 3.2%, p = 0.106) and postoperative complications (6.6% vs. 3.3%, p = 0.107). No major complications including vasculo-biliary injury were recorded in either group. Group A had a significantly longer operative time than Group B (62.48 vs. 51.52, p < 0.001). LC performed by the surgical resident was safe although operative time was longer. However, inexperienced surgeons must always remember to confirm the CVS and follow basic laparoscopic surgery techniques during LC. These principles should be taught by attending staff over the learning curve. Lastly, we recommend the “4Ss” (Subject, Standardization, Stepwise approach, Supervision)” for safe and effective training in LC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic cholecystectomy (LC) is widely performed to treat gallbladder diseases such as acute cholecystitis [1,2,3]. As populations continue to age, the demand of surgery for gallbladder disease will increase, and LC is a necessary part of the surgeon’s repertoire [4]. However, LC can cause critical complications such as vasculo-biliary injury, which makes it difficult to learn and practice [5,6,7,8].
Because of the need for LC and the risks it entails, sophisticated LC training is required, especially during residency. In fact, Friedman et al. reported that the rate of biliary complications was lower in operations performed by surgeons who learned LC during their residency than in those performed by surgeons who did not [9].
However, for various reasons, there are not many opportunities for surgical residents to learn LC. One reason is that the procedures of minimal invasive surgery are difficult to manipulate, and there are fewer opportunities for education than in open surgery [10, 11]. The second reason is that there are critical complications of LC such as vasculo-biliary injury, which makes it difficult to obtain surgical opportunities [5,6,7,8]. In addition, LC training is hard to carry out because of restrictions in residents’ working times and ethical and legal issues that have arisen recently [12].
Although, despite these difficulties, efforts are frequently made to teach LC during residency, most surgical residents require extra training after their residency. In fact, a United States study reported that about 65% of surgical residents pursue additional training for laparoscopy [13], and about 82% reported a lack of education in minimally invasive surgery in Canada [14].
In this study, we analyzed 151 cases of LC performed by a single surgical resident in the Republic of Korea. In this way, we attempted to assess the safety of the LC performed by surgical residents. In addition, we tried to identify effective learning programs based on the experience of this one surgical resident.
Materials and Methods
We retrospectively reviewed a total of 428 LCs performed between October 2014 and September 2016 in Hanyang University Hospital, Seoul, Republic of Korea. These operations were classified into two groups according to the operator. Group A contained 151 cases of LC performed by the surgical resident, and Group B comprised 277 cases performed by an experienced surgeon. All the operations of Group A were performed with the experienced Group B surgeon as camera operator and the “critical view of safety (CVS)” was confirmed [15, 16]. This restrospective study was approved by the Institutional Review Board (IRB) of Hanyang University Hospital, Seoul, Korea, and all research conducted adhered to the tenets of the Declaration of Helsinki (IRB No. 2018–09-021).
Training Program for Surgical Residents
A surgical resident’s education during the first and second years includes participation as camera operator in more than 200 cases of LC, two or three experiences of animal laparoscopic surgery using pigs, and the study of anatomy texts, surgical procedures, and their complications.
After that, when the surgical resident is in the third and fourth years, he or she undertakes LC stepwise, first for non-inflammatory gallbladder then for inflammatory gallbladder or 3-port operations. In addition, from the third year, the resident performs operations such as laparoscopic appendectomy together with the “starting” surgery.
Operative Technique
Using the Hasson technique, a 12-mm camera port is inserted into the subumbilical area, and a pneumoperitoneum is formed. Three more trocars are inserted under camera vision. When necessary, adhesiolysis is carried out, and important signposts such as the falciform ligament and Rouviere’s sulcus are identified (Fig. 1A). Serosal dissection is performed based on these parameters followed by dissection of the subserosal layer (Fig. 1B). The cystic artery and cystic duct are identified in the hepatocystic area, CVS is confirmed (Fig. 1C), and ligation is performed using an endoclip for each artery and duct. Finally, the gallbladder is removed from the gallbladder bed, and bleeding is controlled. The gallbladder is removed with an endopouch through a subumbilical incision, and, if necessary, a drain is inserted in the foramen of Winslow. Thereafter, the trocar sites are closed and the operation terminated.
Anatomical point of LC: (A) Dissection line with Rouviere’s sulcus. (B) Subserosal in layer. (C) Critical view of safety. (A) The white line that initiates the dissection with the gallbladder pulled forward establishes the hypothetical dissection line connecting Rouviere’s sulcus and the falciform ligament. (B) When the subserosal layer is approached, the critical view of safety (CVS) can be achieved with minimal bleeding and safe dissection. (C) Prior to ligation of the cystic artery (arrow head) and cystic duct (arrow), the CVS has to be obtained on both the anterior (C1) and posterior (C2) fields of view
The 3-port operation was performed in the same manner as described above except that one fewer port was used.
Statistical Analysis
All statistical analyses were performed with SPSS 21.0 software (SPSS Chicago, IL, USA). The Chi-square test and Fisher’s exact test were used to compare categorical variables, and Student’s t test was used to compare continuous variables. A p value < 0.05 was defined as statistically significant in all analyses.
Results
Comparison of Clinical Data Between Two Groups
Table 1 summarizes comparisons of the patient characteristics and surgical outcomes in Groups A and B. There were no statistically significant differences between the two groups in age, sex, body mass index (BMI), rate of acute cholecystitis, rate of 3-port operation, conversion rate, rate of complications (during or after surgery), and deaths. However, American Society of Anesthesiologists (ASA) scores, operation times, and hospital days differed significantly between the groups (p = 0.018, p = 0.001, and p = 0.021, respectively).
Case Distribution per Period in Group A
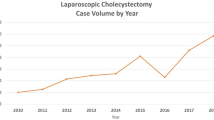
The research period of 24 months was divided into 4 quarters of 6 months (Fig. 2). Of the 151 Group A operations, 36 were performed in the first year, and the others were performed in the following year. Among 26 operations for acute cholecystitis, only 5 were performed in the first year. LC via a 3-port operation was not performed in the first year, and 17 operations were performed in the following year.
Distributions of cases per period (Group A, surgical resident), In Group A (surgical resident), the total laparoscopic cholecystectomy (LC) number increases over time. The relatively difficult operations, acute cholecystitis and 3-port operations, were also performed more in the 2nd year than the 1st year
Complications and Problems in Group A
There were 12 perioperative complications in Group A (surgical resident). Of these, 10 were postoperative complications, all of which were wound complications solved with simple dressings, and 2 were intraoperative complications. One of these was converted to open surgery and bleeding control was performed, and there was a prolonged hospital stay after surgery. The other was a small bowel injury resulting from insertion of the subumbilical trocar. The patient fasted during an additional period and had longer hospital stay; otherwise, no other complications occurred.
Although not complications, 5 operations were assisted by an experienced surgeon (Table 2). In these 5 cases, the experienced surgeon participated in some aspects of the surgical procedures to deal with problems, and all the patients recovered without complications.
Special Cases in Group A
Some of the 151 cases were not typical. Two involved anatomical variations of the gallbladder (Table 2) and underwent LC without any problem, after confirming CVS. In addition, if common bile duct stones or other common bile duct problems were suspected, or if confirmation of the common bile duct was required during surgery, laparoscopic intraoperative cholangiography was performed. Lastly, in patients suspected of having gallbladder cancer, special care was taken to ensure that the gallbladder did not perforate. In fact, T2 stage gallbladder cancer was diagnosed in 2 patients, and extended cholecystectomy was performed after LC.
Discussion
In this study, we analyzed 151 LC operations performed by one surgical resident over 2 years and compared the outcomes with LC performed by an experienced surgeon over the same period. ASA scores were significantly higher in Group B because the experienced surgeon operated mainly on patients with high ASA scores regardless of the severity of gallbladder disease in view of patient safety. In addition, patients in Group B (experienced surgeon) had longer hospital stays than those in Group A, because the patients with high ASA scores needed longer recovery periods after surgery. However, there was no significant difference between the two groups in postoperative outcomes except for operation times. Based on these results, we confirmed the safety of LC performed by a surgical resident under the supervision of an experienced surgeon.
Two (1.3%) complications occurred, and 5 (3.3%) difficulties arose during the Group A operations. However, all the operations were completed with supervision by the experienced surgeon without any significant problems. There were also a few special cases such as one involving a left-sided gallbladder, but they were carried out without any difficulty by the educated step method with securing of CVS.
In addition, since the biliary system including gallbladder has many anatomical variations, and abnormal findings in the common bile duct are common, trainees need education in laparoscopic intraoperative cholangiography so as to be able to confirm the anatomy of the biliary system during surgery.
In the medical education system in the Republic of Korea, a total 6 years of medical school education, including 2 years of premedical school, must be completed to become a doctor. After this, a 1 year internship and 4 years as surgical resident are required. Thus, it takes more than 11 years to become a surgeon. Moreover, most surgeons in the Republic of Korea also need extra training such as fellowships in the divisions of hepatobiliary and pancreatic surgery.
Many efforts are being made to provide education in laparoscopic surgery including LC during the residency period in the Republic of Korea. However, in reality, providing effective education for surgical residents is difficult due to legal problems including working hours, ethical problems, and the fact that many patients want to be operated on by an experienced surgeon. For these reasons, we have tried to develop an LC training program that is effective for surgical residents and safe for patients.
Studies on safe and effective LC training for surgical residents have been conducted in many countries [9, 17,18,19,20,21]. Dario et al. analyzed the safety of LC performed by surgical residents based on a retrospective analysis of 569 LC cases in Italy. [22] In addition, Koulas et al. analyzed 1370 LC cases in Greece and reported on the safety of supervised LC performed by surgical residents [23]. However, many of the studies involved a number of different residents, and most were done from the viewpoint of the experienced surgeon, not from the position of surgical resident. [24,25,26,27]. In this study, we tried to establish the safety of LC performed by surgical residents via the results of LC operations performed by a single resident. In addition, we considered methods for effective LC training from the viewpoint of the surgical resident, not the experienced surgeon.
For effective surgical resident training, we recommend the “4Ss” (Subject, Standardization, Stepwise approach, Supervision) (Fig. 3). The first “S” is the “Subject” and refers to LC-related knowledge such as the relevant anatomy and important indicators such as “critical view of safety (CVS),” post-operative complications, and so on. This knowledge is required to support accurate surgical technique and minimize complications. The second “S” stands for “Standardization”. Standardization of the surgical procedure and technical maneuvers, as well surgical instruments, can minimize the confusion that may occur during surgery. The third “S” stands for “Stepwise approach” and refers to the step-by-step experience of the operation as provided in our surgical resident training program. Initially, the surgical resident participates in the surgery as the camera operator, and after he/she has performed a simple operation such as a non-inflammatory GB, operations such as inflammatory GBs and 3-port procedures are performed. The last “S” is “Supervision”, which is essential for patient safety and the state of balance of residency training.
Conclusion
Under the supervision of an experienced surgeon, standardized LC performed by a surgical resident is safe. “4Ss” (Subject, Standardization, Stepwise approach, Supervision)” are recommended for effective surgical resident training in LC.
References
Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, Endo I, Umezawa A, Asai K, Suzuki K, Mori Y, Okamoto K, Pitt HA, Han HS, Hwang TL, Yoon YS, Yoon DS, Choi IS, Huang WSW, Giménez ME, Garden OJ, Gouma DJ, Belli G, Dervenis C, Jagannath P, Chan ACW, Lau WY, Liu KH, Su CH, Misawa T, Nakamura M, Horiguchi A, Tagaya N, Fujioka S, Higuchi R, Shikata S, Noguchi Y, Ukai T, Yokoe M, Cherqui D, Honda G, Sugioka A, de Santibañes E, Supe AN, Tokumura H, Kimura T, Yoshida M, Mayumi T, Kitano S, Inomata M, Hirata K, Sumiyama Y, Inui K, Yamamoto M (2018) Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). Journal of hepato-biliary-pancreatic sciences 25:73–86
Peng W, Sheikh Z, Nixon S, Paterson-Brown S (2005) Role of laparoscopic cholecystectomy in the early management of acute gallbladder disease. BJS 92:586–591
Kwon YJ, Ahn BK, Park HK, Lee KS, Lee KG (2013) What is the optimal time for laparoscopic cholecystectomy in gallbladder empyema? Surg Endosc 27:3776–3780
Stinton LM, Shaffer EA (2012) Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut and liver 6:172–187
Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG (2001) Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg 234:549–559
Club SS (1991) A prospective analysis of 1,518 laparoscopic cholecystectomies. N Engl J Med 324:1073–1078
Lau WY, Lai EC, Lau SH (2010) Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg 80:75–81
Connor S, Garden O (2006) Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg 93:158–168
Friedman R, Pace B (1996) Resident education in laparoscopic cholecystectomy. Surg Endosc 10:26–28
Lomanto D, Lawenko M, Lopez-Gutierrez J (2009) Training in minimally invasive surgery: an Asian perspective. Asian J Endoscopic Surg 2:65–67
Wolfe BM, Szabo Z, Moran ME, Chan P, Hunter JG (1993) Training for minimally invasive surgery. Surg Endosc 7:93–95
Rea DJ, Smith M (2018) Resident Duty Hours in Surgical Education. Surgeons as Educators: Springer. p. 163–87
Rattner D, Apelgren K, Eubanks W (2001) The need for training opportunities in advanced laparoscopic surgery. Surg Endosc 15:1066–1070
Chiasson P, Pace D, Schlachta C, Mamazza J, Poulin E (2003) Minimally invasive surgery training in Canada. Surg Endosc Other Interv Tech 17:371–377
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 211:132–138
Strasberg SM (2002) Avoidance of biliary injury during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci 9:543–547
Böckler D, Geoghegan J, Klein M, Quasim W, Turan M, Meyer L (1999) Implications of laparoscopic cholecystectomy for surgical residency training. JSLS 3:19
Kauvar DS, Braswell A, Brown BD, Harnisch M (2006) Influence of resident and attending surgeon seniority on operative performance in laparoscopic cholecystectomy1. J Surg Res 132:159–163
O'Bryan MC, Dutro J (2008) Impact of laparoscopic cholecystectomy on resident training: fifteen years later. J Surg Educ 65:346–349
Bencini L, Bernini M, Martini F, Rossi M, Farsi M, Boffi B, Miranda E, Moraldi L, Moretti R (2008) Safety of laparoscopic cholecystectomy performed by surgical residents. Chir Ital 60:819–824
Torney MS, Dell-Kuster S, Mechera R, Rosenthal R, Langer I (2012) The cost of surgical training: analysis of operative time for laparoscopic cholecystectomy. Surg Endosc 26:2579–2586
Pariani D, Fontana S, Zetti G, Cortese F (2014) Laparoscopic cholecystectomy performed by residents: a retrospective study on 569 patients. Surg Res Pract 2014:1–5
Koulas S, Tsimoyiannis J, Koutsourelakis I, Zikos N, Pappas-Gogos G, Siakas P et al (2006) Laparoscopic cholecystectomy performed by surgical trainees. JSLS 10:484
Moore MJ, Bennett CL (1995) The learning curve for laparoscopic cholecystectomy. Am J Surg 170:55–59
Cagir B, Rangraj M, Maffuci L, Herz BL (1994) The learning curve for laparoscopic cholecystectomy. J Laparoendosc Surg 4:419–427
Fahrner R, Turina M, Neuhaus V, Schöb O (2012) Laparoscopic cholecystectomy as a teaching operation: comparison of outcome between residents and attending surgeons in 1,747 patients. Langenbeck's Arch Surg 397:103–110
Atabek U, Spence RK, Pello MJ, Alexander JB, Villanueva D, Camishion RC (1993) Safety of teaching laparoscopic cholecystectomy to surgical residents. J Laparoendosc Surg 3:23–26
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethical Approval
This restrospective study was approved by the Institutional Review Board (IRB) of Hanyang University Hospital, Seoul, Korea, and all research conducted adhered to the tenets of the Declaration of Helsinki (IRB No. 2018–09-021).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jung, Y.K., Choi, D. & Lee, K.G. Learning Laparoscopic Cholecystectomy: a Surgical resident’s Insight on Safety and Training During the Initial 151 Cases. Indian J Surg 83, 224–229 (2021). https://doi.org/10.1007/s12262-020-02350-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02350-4