Abstract
Pneumoperitoneum using carbon dioxide (CO2) has well-known effects on respiratory system, cardiovascular system, haematological system, pregnancy etc. However, there are no previous published studies regarding the independent effect of CO2 pneumoperitoneum on gastrointestinal dysmotility or post-operative ileus. The purpose of our study was to establish whether prolonged intra-operative CO2 pneumoperitoneum has a correspondingly prolonged post-operative ileus. This experimental study was done using 60 adult guinea pigs, randomly divided into 6 batches of test and control. The test group was subjected to anaesthesia and pneumoperitoneum while the control group was subjected to only anaesthesia for the same duration. Starting with 15 min, each successive batch received an increment of 15 min of pneumoperitoneum and/or anaesthesia time until a maximum of 90 min. The animals were observed post procedure period for time duration of recovery from anaesthesia, ambulation, start of spontaneous feeding and defecation. This study leads us to conclude that the length of CO2 pneumoperitoneum does contribute to post-operative gastrointestinal dysmotility for prolonged procedures, in addition to the central depressant effects of anaesthetics and carbon dioxide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carbon dioxide (CO2) is the most commonly used gas for pneumoperitoneum [1]. It has low toxicity and is inexpensive. However, it can cause hypercapnia, acidaemia, pulmonary hypertension, cardiovascular and renal impairment [2,3,4,5,6]. Studies have demonstrated changes in normal physiology of the peritoneal cavity and reduced intestinal oxygenation which can worsen healing [7].
Several authors showed that early feeding after laparoscopic colectomy is safe and has advantages in reducing septic complications and overall morbidity when compared with parenteral nutrition [8].
Even though post-operative ileus is usually of lesser duration after laparoscopic surgeries, it can sometimes create troublesome abdominal distension and prolong recovery [9]. The duration of surgery and the specific complexities of individual operations for similar pathology are considered to influence post-operative ileus. The pathogenesis of this obligatory period of gastrointestinal quiescence is complex and incompletely understood.
Our review of literature revealed studies on the effect of pneumoperitoneum on respiratory system, cardiovascular system, haematological system, effect on pregnancy etc. [4, 10] However, we could not find any previous studies done on the effect of pneumoperitoneum on gastrointestinal dysmotility or post-operative ileus. This may be an important factor in post-operative recovery after laparoscopic surgeries which are otherwise uncomplicated. Surgeries may take longer than expected due to multiple factors including inexperienced surgeons. Such information would be helpful in standardising post-operative protocols across similar laparoscopic procedures done by surgical teams who take varying durations for standard uncomplicated procedures.
Karabicak et al. studied the effect of hypercarbia on healing of colonic anastomosis during pneumoperitoneum [11]. This study used forty guinea pigs weighing 500–550 g. Pneumoperitoneum with CO2 at a pressure of 12 mmHg was attained in the guinea pigs and maintained for 30 min. Arterial blood samples showed that hypercarbia, acidosis and hypoxia were all present in the pneumoperitoneum groups, and these levels correlated with the volume of CO2 absorbed which was dependent on the length of pneumoperitoneum [11].
Waseda et al. compared the effect of CO2 and helium pneumoperitoneum and looked at the recovery of post-operative gastrointestinal motility in male Sprague-Dawley rats [12]. The rats were divided into four groups: control, CO2 insufflation, helium insufflation and open laparotomy. The insufflation pressures were 10 mm Hg and duration of the insufflation was 1 h in all the rats. Gastrointestinal motility was evaluated by quantifying the distribution of markers placed into the stomach. The authors concluded that gastric emptying and transit time were significantly prolonged in the CO2 group compared with the helium insufflation group.
Our study aimed to evaluate the effects of duration of carbon dioxide pneumoperitoneum on gastrointestinal motility. The objectives of our study were (a) to determine whether the duration of gaseous distention of peritoneal cavity with CO2 during pneumoperitoneum contributes as an independent factor towards duration of post-operative gastrointestinal dysmotility and (b) to postulate post-operative feeding protocols on the basis of inference thus derived.
Methodology
This study was conducted in the experimental surgery laboratory of our hospital. All animals were inbred according to the Indian Council of Medical Research (ICMR) and Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA) guidelines for laboratory animals [13, 14]. Institutional animal ethics committee approval was obtained for the study.
A batch of 10 healthy guinea pigs with weight of 500–800 g was chosen and kept fasting overnight in same environmental condition. The batch was randomly divided into two groups of five each, test and control. The test group was subjected to anaesthesia and pneumoperitoneum while the control group was subjected to only anaesthesia for the same duration, to negate the possible confounding effects of anaesthesia on the experiment.
All the animals were anaesthetized for the duration of test by intraperitoneal injection of ketamine at the rate of 30 mg/kg and midazolam 2 mg/kg [15]. In the test group, pneumoperitoneum was created by insufflating CO2 into the peritoneal cavity through a Veress needle. The CO2 pressure was maintained at 12 mm Hg continuously [11].
The duration of pneumoperitoneum and/or anaesthesia for the first batch of animals was 15 min. An increment of 15 min of pneumoperitoneum and/or anaesthesia time was done for successive batches of animals until a maximum of 90 min, i.e. 6 batches of animals.
The oral cavity of the animals was inspected for any residual food in their mouth pouches. This was to prevent aspiration of the food particles. After sedation, the eyes of the animals were protected using sterile lubricating eye drops.
Animals were placed in their earmarked cages and allowed to recover from anaesthesia spontaneously. A closed circuit TV camera (CCTV) was attached to each cage and connected to a central recording device for convenience and clarity of observation.
They were observed in post procedure period for time duration to:
-
(a)
Recovery from anaesthesia—arousal
-
(b)
Recovery from anaesthesia—ambulation
-
(c)
Start of spontaneous feeding
-
(d)
Defecation.
For the purpose of the study, the recovery durations were defined as:
Arousal time: Time from completion of procedure to awakening, depicted by opening of eyes and raising of head.
Ambulation: Time taken from cessation of procedure to the first successful steps with purposeful movement after arousal.
Defecation time: Time from completion of procedure to defection.
Feeding time: Time from completion of procedure to spontaneous feeding.
Statistical Analysis
All values are expressed as mean ± standard deviation. SPSS software version 22.0 (IBM Armonk, NY, USA) was used for statistical analysis. Mann-Whitney U and Wilcoxon signed rank tests were done for the non-parametric variables. P value < 0.05 was considered statistically significant.
Results
As per the data collected (Table 1), the arousal times are prolonged in the pneumoperitoneum group across all batches. After initial arousal, these test animals showed a proportionately delayed ambulation time across batches. This reflects a central depressant action of carbon dioxide, in addition to the sedating effects of the anaesthesia drugs. The central sedating effects of carbon dioxide are more prominent in the longer duration pneumoperitoneum groups.
The average feeding and defecation durations after anaesthesia were also longer in the pneumoperitoneum group. Even within the control groups, delay in ambulation had reflected in a proportionate delay in onset of spontaneous feeding. However, most animals were spontaneously feeding soon after they could ambulate. These observations show that the feeding times correlated with the ambulation times and that animals were ready for feeding almost as soon as they were ready for ambulation.
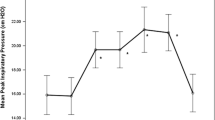
Now, the question was whether the statistical significance of higher durations of pneumoperitoneum, with respect to defecation and feeding durations in pneumoperitoneum group, was due to central effect of CO2 alone or also due to an added local GI effect of CO2. This was brought out by comparing the proportionality of the increase in the test groups for each of the factors. Difference of test minus control values was calculated for each duration group for each of the behaviours and plotted as a line diagram (Fig. 1). The test and control difference values of all the behaviours show almost parallel lines up to 60-min procedure. After 60 min, the feeding and defecation lines become steeper than the arousal line.
Discussion
In the 15-min and 30-min procedure group, there was no statistical significance between the test and control groups for all 4 behaviours evaluated. In the 45-min procedure group, only the arousal durations showed statistically significant difference between the test and control groups. The ambulation, defecation and feeding durations did not show any statistical significance in the 45-min procedure group. In the 60-min, 75-min and 90-min procedure groups, all four behaviours showed statistically significant difference between the test and control groups.
Figure 1 shows that CO2 affects the central nervous system (CNS) and gastrointestinal tract (GIT) in a similar manner up to 60 min durations of pneumoperitoneum, where the depressant effect on the GIT may or may not be independent of the CNS depressant effects of CO2. For procedures longer than 60 min, CO2 pneumoperitoneum affects the GIT independently, in addition to the CNS depressant effect. However, this independent effect of CO2 on GIT may not be statistically significant
Conclusion
In this study, animals in the pneumoperitoneum group had delayed arousal, ambulation, defecation and feeding times. The delay for these behaviours was more prominent for the longer pneumoperitoneum groups. Statistical analysis had shown the delays to be significant with respect to arousal alone for 45-min procedure group and significant for all evaluated behaviours, from the 60-min procedure group onwards. So, CO2 produces a statistically significant central nervous system depression if CO2 pneumoperitoneum is given for 45 min or more. Also, CO2 pneumoperitoneum produces a statistically significant depression of both CNS and GIT if administered for 60 min or more. For durations of 60 min and above, it was also shown that the effect of CO2 pneumoperitoneum on GI motility is partially independent of central depressant effects of pneumoperitoneum. However, this independent effect on GI motility may not be statistically significant. This leads us to conclude that CO2 pneumoperitoneum does contribute to post-operative GI dysmotility for prolonged procedures, in addition to the central depressant effects of anaesthetics and carbon dioxide.
In this study, once ambulant, most animals were seen to feed soon. The findings of this present study justify the current practices. Patients after short duration non-gastrointestinal laparoscopic surgeries maybe started on oral feeds as soon as they are deemed to have recovered from the central effects of general anaesthesia. For procedures longer than 60 min, the ability to independently ambulate confidently and without support may be considered a marker for significant recovery from the general anaesthesia and resolution of post-operative ileus.
References
Yu T, Cheng Y, Wang X, Tu B, Cheng N, Gong J, Bai L, Cochrane Colorectal Cancer Group (2017) Gases for establishing pneumoperitoneum during laparoscopic abdominal surgery. Cochrane Database Syst Rev 6(6):CD009569–CD009569. https://doi.org/10.1002/14651858.CD009569.pub3
de Durães L, C, de Farias IEC, de Morais PHA et al (2013) The effect of carbon dioxide pneumoperitoneum on the healing colonic anastomosis in rats. Acta Cir Bras 28:670–677
Ivatury RR, Diebel L, Porter JM, Simon RJ (1997) Intra-abdominal hypertension and the abdominal compartment syndrome. Surg Clin North Am 77(4):783–800. https://doi.org/10.1016/S0039-6109(05)70584-3
Safran DB, Orlando R III (1994) Physiologic effects of pneumoperitoneum. Am J Surg 167(2):281–286. https://doi.org/10.1016/0002-9610(94)90094-9
Sharma KC, Brandstetter RD, Brensilver JM, Jung LD (1996) Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 110(3):810–815. https://doi.org/10.1378/chest.110.3.810
Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, Büchler MW (2004) Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg 21(2):95–105. https://doi.org/10.1159/000077038
Bessell JR, Karatassas A, Patterson JR, Jamieson GG, Maddern GJ (1995) Hypothermia induced by laparoscopic insufflation. Surg Endosc 9(7):791–796. https://doi.org/10.1007/BF00190083
Moore FA, Feliciano DV, Andrassy RJ et al (1992) Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann Surg 216(2):172–183. https://doi.org/10.1097/00000658-199208000-00008
Mattei P, Rombeau JL (2006) Review of the pathophysiology and management of postoperative ileus. World J Surg 30(8):1382–1391. https://doi.org/10.1007/s00268-005-0613-9
Rao D, Kongara D, Snigdha D, Kalyan D (2017) Study of alterations in liver function tests following laparoscopic surgery. IOSR J Dent Med Sci 16:48–54. https://doi.org/10.9790/0853-1603084854
Karabicak I, Kusaslan R, Aydogan F, et al. The effect of hypercarbia on healing of colonic anastomosis during pneumoperitoneum. Med J Bakirköy. January 2010
Waseda M, Murakami M, Kato T, Kusano M (2005) Helium gas pneumoperitoneum can improve the recovery of gastrointestinal motility after a laparoscopic operation. Minim Invasive Ther Allied Technol 14(1):14–18. https://doi.org/10.1080/13645700510010782
CPCSEA Standard operating procedures (SOP) for IAEC, New Delhi, 2010. http://cpcsea.nic.in/WriteReadData/userfiles/file/SOP_CPCSEA_inner_page.pdf
Guidelines for use of laboratory animals in medical colleges, Indian Council of Medical Research, New Delhi, 2001. http://medicaleducationunit.yolasite.com/resources/ICMR-animal use guidelines.pdf. ICMR
Guidelines on anesthesia and analgesia in guinea pigs, Animal care and use program, University of Michigan,2018. https://az.research.umich.edu/animalcare/guidelines/guidelines-anesthesia-and-analgesia-guinea-pigs
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional animal ethics committee approval was obtained for the study.
Conflict of Interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Badarudeen, B., Varghese, B.K., Kumar, M. et al. Effect of Duration of CO2 Pneumoperitoneum on Post Laparoscopic Gastrointestinal Dysmotility: an Experimental Study. Indian J Surg 83, 201–205 (2021). https://doi.org/10.1007/s12262-020-02344-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02344-2