Abstract
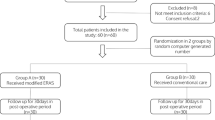
Enhanced recovery after surgery (ERAS) pathways are widely used in elective surgical procedures. The objective of this study was to evaluate the feasibility and efficacy of ERAS pathways in patients undergoing emergency surgery for perforated peptic ulcer (PPU). The single-centre prospective study was conducted in patients with PPU undergoing emergency open simple closure with Graham’s patch technique were randomized into 42 patients in ERAS group and 43 patients in standard care group in the ratio 1:1. Patients with refractory shock, ASA ≥ 3 and multiple perforation and size > 1 cm were excluded. The outcomes were studied with length of hospitalization (LOH), functional recovery parameters and postoperative morbidity. LOH in ERAS group was significantly shorter (mean difference of 5.31 ± 1.102 days; p < 0.001). Patients in ERAS group had a significantly early functional recovery (days) for the time to first fluid diet (1.904 ± 0.72; p < 0.001), and first semi-solid diet (3.1 ± 0.48; p < 0.001), first stool (3.81 ± 0.76; p < 0.001) and removal of drain (2.19 ± 0.39: p < 0.001). There was a significant reduction in postoperative morbidity rate in ERAS group compared with standard care group. The application of enhanced recovery pathways in patients with perforated peptic ulcer undergoing emergency surgery is safe and feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perforated peptic ulcer (PPU) is one of the most common acute complications and surgical emergencies in patients with peptic ulcer disease. PPU occurs in about 3.8 to 14% per 100,000 patients with mortality rate of 10 to 25% [1]. The enhanced recovery after surgery (ERAS) pioneered by Henrik Kehlet in the late 1990s has been increasingly adopted over time for favourable surgical outcomes [2]. ERAS program utilize a multimodal and multidisciplinary approach to perioperative management with the aim of minimizing perioperative and intraoperative stress responses to surgery leading to a faster discharge [3, 4]. Implementing all the care elements of ERAS in emergency situation is a challenge [4, 5]. The aim of this study was to evaluate the efficacy and feasibility of enhanced recovery pathway in patients who underwent emergency surgery for perforated peptic ulcer.
Materials and Methods
This study was a single-centre, prospective, parallel arm, randomized controlled clinical study carried out in the department of surgery in a teaching hospital of north-eastern India in a study period of 1 year. The study was approved by the Institute Ethics Committee. Written informed consent was taken from all the participants and patients were given full freedom to withdraw at any point during the study. Each patient was provided with detailed information about the study and was requested to sign an informed consent form.
All patients who presented to the emergency surgical team with diagnosis of perforated peptic ulcer were recruited and assessed for eligibility. The following patients were excluded from the study: age < 18 years’ refusal to give consent, pregnant patients, patients with history of chronic steroid use, coexistent psychiatric or neurological illness, ASA (American Society of Anaesthesiologists) class 3 or 4 and patients with refractory septic shock at presentation. Intraoperative findings with spontaneously sealed off perforations, multiple perforated ulcers, coexistent bleeding and perforated duodenal ulcer ≥ 10 mm were excluded.
Patients with a perforated ulcer less than 10 mm in size who underwent Graham’s patch repair (GPR) were included in the study. The patients were randomized into 2 groups according to their hospital register number, which was automatically given by the computer-based data processing system at admission. Randomization was made at the end of the surgical procedure. Patients with odd and even protocol numbers were included in groups 1 and 2, respectively. Group 1 was the control group and received standard postoperative care, and group 2 was the ERAS group. The surgical team was blinded to this protocol number.
Patients in both standard care and ERAS groups received identical preoperative care. They were placed nasogastric (Ryle’s) tube at admission and administration of crystalloids for fluid replacement. They also received preoperative intravenous (IV) antibiotic therapy with ceftriaxone and sulbactum (1.5 g IV stat) and metronidazole (500 mg IV stat) and IV acid reducing therapy with pantoprazole (40 mg IV 12 hourly) and IV analgesic paracetamol (1 g IV 8 hourly). The differences between the two groups in the care pathways are shown in Table 1.
Simple closure of the perforated peptic ulcer by Grahams patch technique under general anaesthesia [6] was the common surgical procedure done in all patients. The surgical procedure was carried out by senior residents. The size of perforation, nature and severity of the contamination were noted. A 28-F abdominal safe drain was placed in the sub-hepatic space before closure of the abdomen. The differences in the anaesthetic protocols between the two groups are shown in Table 1.
The control (standard care) group patients received standard postoperative care described in detail in Table 1. Patients in ERAS group received an adapted criterion for the use of drains and tubes as the safety of an ERAS protocol in emergency has not been well established (Table 1). ERAS care is based on principles such as non-opioid multimodal analgesia, early nutrition and early mobilization of the patients. In both the groups, oral feeding was discontinued in patients who complained of pain abdomen, distension, vomiting or diarrhoea. Feeding was reinitiated after the symptoms had completely subsided, and active bowel sounds had reappeared. All patients were discharged when they had tolerated solid diet for at least 24 h and had passed stool and in the absence of other factors such as fever, wound infection, anastomotic leakage, etc.
All patients were discharged with oral acetaminophen (500 mg on demand) and were advised to oral rabeprazole (20 mg Q12H) for 3 months. All patients were reviewed 10 days after discharge for wound discharge, fever, intolerability of food, pain abdominal, distension and vomiting. Patients were further followed up at 6 weeks for the presence of intractability of pain, vomiting, return to work, tolerability of food or any complications for need of readmissions.
.
Data Collection and Statistical Analysis
Proforma was prepared, and data was collected by the clinicians who did not engage in the study. Patients’ demographic variables, duration of the symptoms at presentation, ASA class, pulse rate, systolic blood pressure, haemoglobin, albumin and intraoperative variables such as size of perforation, nature of peritoneal contamination, were recorded. Statistical analysis was performed using Graph Pad InStat 3 for windows. Variables are expressed as numbers and percentages. Continuous data are expressed as mean with standard deviation, with calculation of the probability value to measure the significance of differences. The Student t test was used for the comparisons of continuous variables. P value less than 0.05 was considered statistically significant.
Results
The main outcome was the length of hospital (LOH) stay between the two groups, and other two outcomes were functional recovery parameters and postoperative morbidity. The functional recovery parameters included time for removal of nasogastric tube, drains and catheter; duration of ileus, time for first fluid diet and first semi-solid diet: and time for passage of first stool. Post operative morbidity parameter for need for extra anangsia, need for reinsertion of nasogastric tube, incidence of postoperative nausea and vomiting (PONV), SSI (Skin and soft tissue infection), pulmonary complications, need for readmission and reoperations were noted in study group.
In the study period of 1 year, 114 patients of PPU were assessed for eligibility, and 85 patients were randomized after exclusion preoperatively and intraoperatively. There were 42 patients in standard perioperative care group and 43 to adapted ERAS group. There was no loss to follow up during the study period. The two groups were comparable in terms of all demographic and clinic-pathological characteristics (Table 2).
Outcome Measures
Length of Hospitalization (LOH)
LOH in standard care group patients was 9.05 ± 1.27 days and in ERAS group patients was 5.31 ± 1.102 days. The length of hospital stay was reduced significantly by 3.74 days in adapted ERAS group when compared with standard care group (p < 0.0001, CI 3.23 to 4.25). (Table 3)
Functional Recovery Parameters
The patients in the adapted ERAS group had a significantly early resolution of ileus and had the nasogastric tube removed earlier when compared with standard care group (Table 3). Patients in ERAS group had a significantly early return of bowel functions in terms of appearance of first bowel sounds, first flatus and first stools, and an earlier resumption of oral feeds (Table 3). Eight patients developed postoperative ileus, three in the adapted ERAS group (7.14%), and five in standard care group (11.63%), and were managed conservatively with nasogastric tube reinsertion, bowel rest and hydration.
The patients in the adapted ERAS groups had the drains and the urinary catheter removed significantly early when compared with the standard care group (Table 3). Ninety-three percent of patients in the standard care group had the abdominal drain in situ for more than 4 days, while all patients in the adapted ERAS group had got their drains out by 3rd day. The difference in the mean the time of removal of drain (3.114 days, CI 2.79 to 3.44, P < 0.0001) was significant. The mean time for mobilization was also significantly shorter in the ERAS group (Table 3).
Postoperative Morbidity Parameters
There was significant reduction in the various postoperative morbidity parameters in the ERAS group when compared with the standard care group (Table 4). The need for extra analgesia was significantly reduced in the ERAS group (16.67%) when compared with standard care group (46.51%). There was a significant reduction in postoperative morbidity rates such as surgical site infections in ERAS group (14.29%) compared with standard care group (30.23%), postoperative nausea and vomiting in ERAS group (19.05%) compared with standard care group (65.12%) and pulmonary complications in the ERAS group (4.76%) compared with standard care group (16.28%). Two patients in the standard care group and none in the ERAS group were readmitted for distension and vomiting which was treated conservatively. There was no 30-day morbidity or mortality or reoperation reported in both the arms.
Discussion
In this prospective trial, there was a significant reduction in hospital stay with no worsening of the postoperative complication rates in patients managed with ERAS protocols when compared with the standard care. The patients in the ERAS group had a significantly earlier functional recovery in terms of bowel functions, earlier resumption of oral feeds and earlier mobilization. Hence, it demonstrates the safety, efficacy and feasibility of an adapted ERAS protocol in emergent situations.
In the present study, attempt was made to use the possible ERAS care elements of preoperative, intraoperative and postoperative components in patients managed for PPU. There are few reports of successful use of modified ERAS protocols in emergency situations; these studies were, however, limited by inclusion of few care elements and fewer patients [7, 8]. One study evaluated the feasibility of ERAS protocols in a prospective RCT on 47 patients with laparoscopic Grahams patch repair [9]. However, emphasis was given solely on postoperative ERAS care elements such as non-opioid analgesics, omission of nasogastric decompression and resumption of liquid feeds by 24 h postoperatively. A systematic review done concluded the success of an ERAS pathway in various emergency surgeries [10].
In emergency setting, the limited literature available demonstrates a decreased LOH by utilization of ERAS protocols. In two reported studies on patients of urgent colectomy, a reduction in LOH of 2–3 days was reported [11, 12]. A reduction of LOH by 3 days was reported in patients who underwent laparoscopic Graham patch repair managed by ERAS protocols [10]. In the present study, the hospital stay was reduced by 3.7 days in the ERAS group (Table 3). The shortened hospital stay may be attributed to the implementation of more number of ERAS care elements, especially in the preoperative and intraoperative period. Inclusion of these elements in the ERAS pathway is important as the intraoperative management plays a key role in deciding the outcome in the postoperative period [13]. Failure of adherence or implementation of intraoperative elements might have led to poor outcomes even though a strict protocol was followed in the postoperative period.
ERAS protocols for major elective upper gastrointestinal surgery support safe omission of routine nasogastric decompression [14, 15]. However, similar reports in an emergency situation were lacking [12]. In one study, the nasogastric tube was immediately removed after the patients’ recovery from anaesthesia [9]. In the present study, NG tube was withdrawn if drainage was ≤ 300 ml over a period of 24 h. There were reports of prolonged ileus, delayed resumption of orals and increased pulmonary complications with the use of nasogastric decompression [14]. In the present study, a significantly shorter duration of ileus and low incidence of pulmonary complications rate (4.76%) in the adapted ERAS group which had a significant duration (mean of 1.2 days) of NG decompression were found when compared with the standard care. One study reported a mean of 1.5 days for resumption of orals in the ERAS group [9]. In the present study, liquid and semi-solid diet were resumed at an average of 1.9 and 3.1 postoperative days, respectively, in patients who had open Grahams patch repair combined with ERAS care elements. Likewise, an average of 3.4 days was reported in patients who had urgent colectomy managed with ERAS protocol [11]. The evidence for omission of drains in emergent situations is lacking. In present study, majority of the patients in the ERAS group had the drains removed on the second postoperative day. Moreover, with an adapted protocol, it was possible to attain shorter time to first flatus, first feeds and first walk, thus accelerating patients’ recovery as in the previous reports. Hence, the truncated use of NG decompression and drains in the present study did not interfere with the successful implementation of ERAS protocol. One study had reported a reduction of 20% in the number of patients of emergency laparotomy requiring catheter beyond 2 days owing to the “diffusion” of ERAS practices from elective procedures [7]. In the present study, majority of the patients of the adapted ERAS group had the urinary catheter removed within 2 days. The effect of early removal of catheter was also reflected in a significant reduction in incidence of UTI in ERAS group.
Relieving patient anxiety by preoperative counselling is of utmost importance especially in an emergency situation. Intraoperatively, short-acting opioids with lesser carry over effect were utilized. In one study, it was resorted to NSAIDs for management of postoperative pain with opioids for breakthrough pain [9]. In the present study, the need for extra analgesia was found to be significantly higher in the standard care group (46.51%) when compared with the ERAS care group (16.67%). The present study thus demonstrates the safe and successful implementation of adapted analgesic care elements in the emergency setting.
Another study comparing all emergency laparotomies in pre- and post-ERAS period reported a significant reduction in the complications in the post-ERAS period suggesting its safe role in emergency [7]. Non-significant reduction in the overall complication rates in patients of urgent colectomy managed with ERAS protocol reported in one study [12]. In the present study, there was a significant reduction in the rates of surgical site infections (14.29%), pulmonary complication rate (4.76%) and incidence of PONV rate (19.05%) in the ERAS group (Table 4). LOH is associated with high incidence of hospital acquired infections [16,17,18]. In the present study the LOH (Length of Hospital) stay was low. This was relected by low incidence of SSI and pulmonary complications.
There were two readmission cases in standard care group which were managed conservatively. Patients who developed minor complications before discharge continued to stay in the hospital; however, none of the patients who were discharged early in the adapted ERAS group had readmissions within 30 days of discharge.
Conclusions
ERAS pathways, in modified form, are feasible and safe for application in select patients undergoing simple closure in perforated duodenal ulcer surgery. Implementation of ERAS programs results in major improvements in clinical outcomes. The ERAS can be a standard care in emergency surgery.
References
Søreide K, Thorsen K, Søreide JA (2014) Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg 101(1):e51–e64
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198
Scott MJ, Miller TE (2015) Pathophysiology of major surgery and the role of enhanced recovery pathways and the anaesthesiologist to improve outcomes. AnesthesiolClin 33(1):79–91
Quiney N, Aggarwal G, Scott M, Dickinson M (2016) Survival after emergency general surgery: what can we learn from enhanced recovery programmes. World J Surg 40:1283–1287
Lyon A, Payne CJ, MacKay GJ (2012) Enhanced recovery programme in colorectal surgery: does one size fit all. World J Gastroenterol: WJG 18(40):5661–5663
Graham R (1937) The treatment of perforated duodenal ulcers. SurgGynec Obstet 64:235–238
Wisely JC, Barclay KL (2016) Effects of an enhanced recovery after surgery programme on emergency surgical patients. ANZ J Surg 86(11):883–888
Møller MH, Adamsen S, Thomsen RW, Møller AM (2011) Peptic ulcer perforation (PULP) trial group. Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg 98(6):802–810
Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MA, Dogan Y, Alis H (2014) Enhanced postoperative recovery pathways in emergency surgery: a randomized controlled clinical trial. Am J Surg 207:807–814
Paduraru M, Ponchietti L, Casas IM, Svenningsen P, Zago M (2017 Apr) Enhanced recovery after emergency surgery: a systematic review. Bullet Emerg Trauma 5(2):70–78
Roulin D, Blanc C, Muradbegovic M, Hahnloser D, Demartines N, Hübner M (2014) Enhanced recovery pathway for urgent colectomy. World J Surg 38:2153–2159
Lohsiriwat V (2014) Enhanced recovery after surgery vs. conventional care in emergency colorectal surgery. World J Gastroenterol 20:13950–13955
Nygren J, Ljungqvist O, Thorell A (2017) Enhanced recovery after surgery: ERAS. InSurgical Patient Care (pp. 349-361). Springer, Cham
Khan N, Bangash A, Ullah A, Khan A (2011) Postoperative nasogastric decompression is not warranted in elective closure of gut stomas and bilioentericanastamosis: a randomized controlled trial. J Postgrad Med Inst (Peshawar-Pakistan). 22(3)
Shamil N, Quraishi S, Riaz S, Channa A, Maher M (2010) Is nasogastric decompression necessary in elective enteric anastomosis? J Ayub Med College Abbottabad 22(4):23–26
Hassan M, Tuckman H, Patrick R, Kountz D, Kohn J (2010) Hospital Length of Stay and Probability of Acquiring Infection. Int J Pharm Healthc Mark 4:324–338
Mujagic E, Marti WR, Coslovsky M, Soysal SD, Mechera R, von Strauss M, Zeindler J, Saxer F, Mueller A, Fux CA, Kindler C, Gurke L, Weber WP (2018) Associations of hospital length of stay with surgical site infections. World J Surg 42:3888–3896
Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, Lee JW, Henderson WG, Moss A, Mehdiratta N, Colwell MM, Bartels K, Kolodzie K, Giquel J, Vidal Melo MF (2017) Postoperative pulmonary complications, early mortality, and hospital stay following non cardiothoracic surgery: a multicenter study by the perioperative research network investigators. JAMA Surg 152(2):157–166
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chndan, M.N., Khakholia, M. & Bhuyan, K. Enhanced Recovery after Surgery (ERAS) Versus Standard Care in Patients Undergoing Emergency Surgery for Perforated Peptic Ulcer. Indian J Surg 82, 1044–1049 (2020). https://doi.org/10.1007/s12262-020-02195-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02195-x