Abstract
Leiomyosarcoma of the inferior vena cava (IVC) is a rare soft tissue sarcoma. Surgical resection with negative margins provides the best chance of long-term cure. Good quality cross-sectional imaging is imperative for preoperative planning of the need of IVC resection and reconstruction. A 31-year-old lady presented with non-specific abdominal pain. Cross-sectional imaging demonstrated a mass lesion arising in the infra-hepatic IVC causing bilateral renal vein thrombosis with good left renal collateral venous circulation. She underwent en-mass resection of the tumour along with right nephrectomy and retro-hepatic IVC ligation. The left kidney could be preserved after left renal vein ligation because of preservation of the draining collaterals demonstrated on preoperative imaging with the help of intraoperative Doppler. Demonstrable adequate draining collaterals on preoperative imaging could dismiss the need for reconstruction of inferior vena cava below the hepatic cloaca.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Leiomyosarcoma of the inferior vena cava (IVC) is a rare tumour of primary vascular origin and affects 1/100000 population [1]. Management and prognosis depend on the anatomical segment of IVC involved. Radical oncological resection offers the best survival rates.
Case
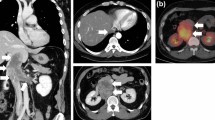
We present the case of a 31-year-old lady presenting with pain in the abdomen since 7 months. Her clinical examination was unremarkable. Contrast-enhance computed tomography (CECT) revealed a mass arising from the infra-hepatic part of IVC and extending into both renal veins, inferiorly up to the level of confluence of common iliac veins (Fig. 1). There was evidence of the right hydroureteronephrosis and left kidney drained through multiple large retroperitoneal collaterals (Fig. 2). Major mesenteric arteries and left renal artery were free. Biopsy from the mass showed high-grade spindle cell sarcoma favouring an intimal sarcoma from IVC.
Following midline laparotomy, the right medial visceral rotation provided good exposure to IVC. Proximal and distal control of IVC was attained and the tumour was dissected free of the aorta and its anterior branches. The left renal vein was found to have a thrombus close to its ostium and was divided carefully preserving the venous collaterals. Intraoperative Doppler confirmed adequate venous drainage of the left kidney through collaterals. Tumour was removed en bloc with the right kidney and retro-hepatic IVC was ligated. The post-operative course was unremarkable with regard to urine output and renal function tests. The histopathology report revealed high-grade leiomyosarcoma of the IVC and negative resection margins were confirmed. The patient received adjuvant radiotherapy 50.4Gy/28# @ 1.8Gy/fraction with IMRT. At 10-months follow-up, the patient is doing well with no evidence of recurrence, deterioration of renal function or lower limb oedema.
Discussion
Leiomyosarcoma of IVC was first described by Perl in 1871 [2]. It is the most common vascular sarcoma described. With regard to an anatomical location in IVC, Kulaylat has classified tumours into 3 groups: segment I, infrarenal; segment II, supra-renal up to but not including the main suprahepatic veins and segment III, suprahepatic with possible intra-cardiac extension. Tumours of segment II are more common and have a better prognosis than type III tumours [3].
Cross-sectional imaging plays a key role in ascertaining the tumour extension and the collateral circulation. Both CECT and magnetic resonance imaging (MRI) have proven to be valuable tools in the evaluation of such patients [4]. IVC resection may be followed by ligation, patch repair or prosthetic reconstruction [5]. Infrarenal type I tumours are generally managed by IVC ligation. Type II and type III tumours often need reconstruction of the IVC to safeguard the drainage of renal and hepatic veins [5]. Reconstruction of the IVC can be in the form of a patch or graft which may be autologous or prosthetic [6]. Reimplantation of the renal vein, autologous transplantation of the kidney to the iliac fossa or nephrectomy are the options in case of involvement of the renal venous ostia [6]. The right nephrectomy is often necessary in case of venous involvement; however, the left kidney can be preserved if there are adequate lumbar, gonadal and azygous collaterals present [7]. However, it must be noted that this left renal vein ligation is mostly well tolerated in the presence of two functioning kidneys, not after the right nephrectomy as in our case. Reconstruction of the IVC is technically challenging, increases the possibility of post-operative complications and, hence, is avoided wherever feasible.
In this case, both renal veins were involved along with the right hydroureteronephrosis. The right nephrectomy was performed but due to the presence of good collateral circulation on preoperative imaging, a successful attempt was made to preserve the left kidney without any reconstruction or transplantation. Intraoperative Doppler is a valuable tool in such a situation.
Post-operatively, there are reports of the significant risk of renal dysfunction sometimes necessitating dialysis after renal vein ligation even in the presence of collaterals [8]. However, that can be mitigated by careful preservation of collaterals, the use of intraoperative Doppler and adequate hydration.
Conclusion
Good cross-sectional imaging, preoperative planning and radical resection with negative margins offer the best possible treatment for inferior vena cava sarcoma. IVC ligation is an option even with bilateral renal venous involvement if adequate collaterals can be identified on preoperative imaging.
References
Mingoli A, Cavallaro A, Sapienza P, Di Marzo L, Feldhaus RJ, Cavallari N (1996) International registry of inferior vena cava leiomyosarcoma: analysis of a world series on 218 patients. Anticancer Res 16:3201–3205
Perl L Ein fall von sarkom der vena cava inferior. Virchows Arch F Path Anat 1871, 53:378
Kulaylat MN, Karakousis CP, Doerr RJ, Karamanoukian HL, O’Brien J, Peer R (1997) Leiomyosarcoma of the inferior vena cava: a clinicopathologic review and report of three cases. J SurgOncol 65:205–217
Cuevas C, Raske M, Bush WH, Takayama T, Maki JH, Kolokythas O, Meshberg E (2006) Imaging primary and secondary tumor thrombus of the inferior vena cava: multi-detector computed tomography and magnetic resonance imaging. Curr Probl Diagn Radiol 35(3):90–101
Ghose J, Bhamre R, Mehta N, Desouza A, Patkar S, Dhareshwar J, Goel M, Shrikhande SV (2018) Resection of the inferior vena cava for retroperitoneal sarcoma: six cases and a review of literature. Indian journal of surgical oncology 9(4):538–546
Wachtel H, Jackson BM, Bartlett EK, Karakousis GC, Roses RE, Bavaria JE, Fraker DL (2015) Resection of primary leiomyosarcoma of the inferior vena cava (IVC) with reconstruction: a case series and review of the literature. J Surg Oncol 111(3):328–333
Daylami R, Amiri A, Goldsmith B et al (2010) Inferior vena cava leiomyosarcoma: is reconstruction necessary after resection? J Am CollSurg 210:185–190
Cancarini GC, Pola A, Pezzotti G, Tardanico R, Cozzoli A, Cunico SC (2002) Recovery of renal function after right nephrectomy, cavectomy and left renal vein ligation. Journal of nephrology 15(2):186–190
Author information
Authors and Affiliations
Contributions
Aditi Chaturvedi: project writing, literature search and reviewing of the manuscript
Shriniket Raghavan: project writing
Mahesh Goel: conceptualization and case management
Shraddha Patkar: conceptualization, case management and reviewing of the manuscript
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chaturvedi, A., Raghavan, S., Goel, M. et al. Leiomyosarcoma of the Inferior Vena Cava with Bilateral Renal Vein Involvement. Indian J Surg 82, 1258–1260 (2020). https://doi.org/10.1007/s12262-020-02188-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02188-w