Abstract
We present the clinical case of a patient who, having been referred for surgery on two-stage hepatectomy, could not have a conventional portal embolization performed as an intermediate step in order to be able to resection the whole of the hepatic illness she was suffering. During right portal embolization (PE), the portography revealed minimal flow in the left portal vein, without thrombosis or stenosis. Given the risk of serious hepatic insufficiency, the embolization procedure was ruled out. Our option was to perform a portal embolization in two stages: initial PE of the right posterior branch, and subsequently, right anterior branch PE. After that, the liver resection could be completed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical treatment of hepatic metastases (HM) is an elective treatment [1]. Nonetheless, only 30% of patients can be offered the surgery [1]. We present the clinical case of a patient who, having been referred for surgery on two-stage hepatectomy, could not have a conventional portal embolization performed as an intermediate step in order to be able to resection the whole of the hepatic illness she was suffering.
Clinical Case
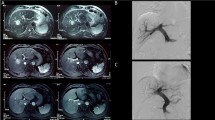
The patient was 67-years-old upon presentation, with a background of encephalitis in infancy, conditioning a slight right hemiparesis and arterial hypertension in medical treatment. In December 2014, she was diagnosed with symptomatic sigmoid neoplasia with synchronous bilobar hepatic metastases by abdominal computer tomography (CT) (Fig. 1): segments II (25 mm), III (< 10 mm), IVa (17 mm), IVb (< 10 mm), VI (< 10 mm), VI–VII (12 mm), and VIII (20 mm). Left hemicolectomy was performed without morbidity. The histopathological result was a moderately differentiated adenocarcinoma, p-TNM T3N0 with MLH-1, MLH-2, and MLH-6 present.
She began treatment with neoadjuvant chemotherapy (ChT) of the hepatic metastases, revealing a positive response according to RECIST criteria. Given the distribution of the lesions and an insufficient left hepatic lobe volume, she was considered for referral for surgery in two stages. She was operated on in March 2015, with resection of the left hepatic lobe lesions being performed. She was subsequently scheduled for right portal embolization (PE), with the portography revealing minimal flow in the left portal vein, without thrombosis or stenosis. Given the risk of serious hepatic insufficiency, the embolization procedure was ruled out. The patient continued with chemotherapy treatment without revealing any progression in the illness, and we therefore considered sequential portal vein embolization (SPVE): initial PE of the right posterior branch, and 4 weeks later, right anterior branch PE. Table 1 shows the portal flow values and hepatic volume measurements before and after the procedures. Throughout this process, the patient continued with ChT treatment. The abdominal CT after completing the process did not show changes in the number and size of hepatic metastases of the right liver lobe, and the liver volumetry showed the correct volume of the left liver lobe.
Finally, in November 2015, the surgical treatment was completed (right hepatectomy) revealing good postoperative progress except for transitory hyperbilirubinemia, rising to 9 mg/dL, but which spontaneously normalized. The patient completed the adjuvant ChT. After 14 months, she revealed an increase in CEA with left inguinal lymphadenopathies and pulmonary metastases diagnosed by abdominal CT and PET-TC, recommencing ChT and dying as a result of the progression of the illness 24 months after the second surgery.
Discussion
The surgical treatment of hepatic metastases is not feasible in a very substantial percentage of patients. Various treatments and technical options have served to increase resection potential. ChT has perhaps been the most significant, and today represents a basic complement in the treatment of such patients [1].
PE is a technique applied since the 1990s, when the future liver remnant is insufficient [2]. However, it is ineffective in some patients, or the execution of the procedure could, as in the case we present, which is nonetheless uncommon, condition serious hepatic insufficiency [3]. As a result, SPVE is a technical option for consideration in this clinical situation to minimize the risks to the patient and attempt surgical recovery which would provide better survival than with ChT alone [1].
References
Adam R, Kitano Y (2019) Multidisciplinary approach of liver metastases from colorectal cancer. Ann Gastroenterol Surg 3:50–56. https://doi.org/10.1002/ags3.12227
Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P et al (1990) Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery 107(5):521–527
Alvarez FA, Castaing D, Figueroa R, Allard MA, Golse N, Pittau G, Ciacio O, Sa Cunha A, Cherqui D, Azoulay D, Adam R, Vibert E (2018) Natural history of portal vein embolization before liver resection: a 23-year analysis of intention-to-treat results. Surgery. 163(6):1257–1263. https://doi.org/10.1016/j.surg.2017.12.027
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lama, C., Parada, C., Artacho, J.R. et al. Sequential Portal Vein Embolization: a Technical Option for Hepatic Metastasis Resection. Indian J Surg 82, 924–926 (2020). https://doi.org/10.1007/s12262-020-02137-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02137-7