Abstract
Around 51 cases of sialolipoma of the salivary gland have been reported worldwide as per the literature reviewed. Majority of cases (n = 25) arise from the parotid gland (51.4%) clinically behaving like pleomorphic adenoma with very less incidence of facial nerve entrapment (14%). Sialolipoma is a rare neoplasm of the salivary glands, described as a distinct entity by Nagao et al. in 2001. Lipomatous neoplasms of the parotid gland are rare tumours accounting 0.6 to 4.4% of all parotid neoplasms with most series reporting an incidence of 1%. It is extremely rare in females, being 10 times more common in males, and the most common age of presentation is the fifth to sixth decade. Numerous histological variants of salivary gland lipoma have been described. Sialolipoma is a rare variant having proliferation of mature adipocytes with secondary entrapment of the normal salivary gland element. We report a rare case of sialolipoma in the left parotid of a 49-year-old woman presented to General Surgery Department who was treated with superficial parotidectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sialolipoma is a rare tumour of the salivary glands, described in 2001 by Nagao et al. [1]. It is a benign lipomatous neoplastic growth of the salivary glands with mature adipose tissue. Sialolipoma occurs in the minor and major salivary glands with an unpredictable and potentially aggressive behaviour [2, 3]. Treatment includes total parotidectomy for deep lobe involvement and superficial parotidectomy in the tumour of outer lobes, with preservation of the facial nerve [3,4,5]. The aim of this article is to report a case of sialolipoma in a 49-year-old female presented with left parotid swelling and discuss the clinicopathological, radiological and histopathological findings. A thorough review of the available world literature revealed only 51 cases of sialolipoma reported so far [6]. Herein, we discuss one more case of sialolipoma and review the literature.
Case Report
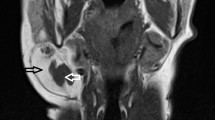
A 49-year-old female presented to the Department of General Surgery with a left parotid mass of approximately 6 months duration, without a history of xerostomia, salivary pain, odynophagia, dysphagia, weight loss, mouth pain, facial weakness or conditions associated with immunodeficiency. On examination, a 2 × 1 cm soft mass was palpated over the left parotid bed, which was nontender and mobile. Clinical diagnosis of pleomorphic adenoma was kept. Computed tomography (CT) scan showed a 9 × 11 × 18 mm-sized well-defined encapsulated, homogenous contrast-enhancing mass noted in the superficial lobe of the left parotid gland at its inferior pole with subtle stranding of overlying fat and skin (Fig. 1). The right parotid, bilateral submandibular and thyroid gland appear normal in size and contrast enhancement. No definite diagnosis was rendered on imaging studies. USG-guided FNA was performed twice, showed presence of many normal salivary glands acini admixed with occasional clusters of ductal epithelial cells in a murky to lipoidal inflammatory background but was indefinite about the diagnosis. Possibility of benign salivary gland lesion was suggested. The patient was treated surgically with a left superficial parotidectomy with facial nerve preservation.
We received multiple, irregular, nodular, tan-yellow, capsulated tissue bits altogether measuring 4 × 2.5 × 1.5 cm. Cut surface in all tissue bits was solid, lobulated and tan-yellow in appearance. Entire tissue was processed for histopathological examination.
Sections taken from all tissue bits showed encapsulated tumour comprising of mature adipose tissue intimately admixed with serous acini and ducts of the salivary gland. Fibro-collagenous tissue, septations and focal lymphoid tissue were also noted in some sections with five lymph nodes showing features of reactive lymphoid hyperplasia. Based on these findings, the diagnosis of sialolipoma was rendered (Fig. 2). Postoperative course was uneventful.
Discussion
Sialolipoma is a newly recognised variant of lipoma characterised by the proliferation of benign salivary gland tissue intimately admixed with mature adipose tissue.
The usual clinical presentation of most patients is in their fourth or fifth decade of life with a slight male preponderance. In the present case, it was reported in a female patient.
Fine needle aspiration (FNA) is not a conclusive investigation modality for diagnosis, as encountered in a similar problem in our case because both fatty and salivary gland tissues are not dysplastic. CT or MRI are superior to ultrasonography in defining the exact location and texture of the lesion. CT is more useful in picking up a lipomatous component of the tumour. On the contrary, MRI is crucial in the detection of glandular elements. In our case, the CT scan showed a hyperdense, homogenous, contrast-enhancing mass in the parotid gland against the usual findings of non-enhancing hypodense mass lesion consistent with lipomatous lesion. Thus CT scan also proved to be non-diagnostic.
It is a well-circumscribed encapsulated lesion microscopically comprising of mature adipose tissue and non-neoplastic salivary gland tissue [1]. There may be slight variations in microscopy in different cases such as atrophy of the glandular structures, ductal dilation with scattered foci of fibrosis, sebaceous and squamous metaplasia, oncocytic changes, myxoid islands and lymphocyte infiltration inside the lipomatous proliferation. [1,2,3, 5].
Differential diagnosis of sialolipoma includes salivary gland lesion with extensive lipomatous components such as lipomatosis, lip adenoma and pleomorphic adenoma with excess of adipose tissue. Presence of normal encapsulated salivary gland tissue with ducts intimately admixed with adipose tissue enables to be distinguished from lipomatous lesion. Lack of normal salivary gland component in lip adenoma differentiates from sialolipoma.
Recommended treatment is superficial parotidectomy with preservation of facial nerve wherein cases with deeper lobe involvement and total parotidectomy is indicated [3]. No recurrence is reported after excision of the tumour.
Referring to our case, superficial parotidectomy was performed with preservation of facial nerve with follow-up of 6 months without any recurrence.
Conclusion
Sialolipoma is a rare salivary gland neoplasm. FNA has a limited diagnostic utility. One should be aware of this entity when seeing a well-circumscribed lesion with adipose tissue component on imaging studies. Preoperative imaging is necessary to establish a diagnosis. However, surgical excision and histopathology are imperative for a definite diagnosis.
References
Nagao T, Sugano I, Ishida Y, Asoh A, Munakata S, Yamazaki K, Konno A, Kondo Y, Nagao K (2001) Sialolipoma: a report of seven cases of a new variant of salivary gland lipoma. Histopathology 38:30–36
Hornigold R, Morgan PR, Pearce A, Gleeson MJ (2005) Congenital Sialolipoma of the parotid gland first reported case and review of the literature. Int J Paediatric Otorhinolaryngol 69:429–434
Michaelidis IG, Stefanopoulos PK, Sambaziotis D, Zahos MA, Papadimitriou GA (2006) Sialolipoma of the parotid gland. J Craniomaxillofac Surg 34:43–46
Ponniah I, Lavanya N, Suresh Kumar P (2007) Island of salivary gland in adipose tissue: a report of three cases. J Oral Pathol Med 36:558–562
Pusiol T, Franceschetti I, Scialpi M, Piscioli I (2009) Oncocytic sialolipoma of the submandibular gland with sebaceous differentiation: a new pathological entity. Indian J Pathol Microbiol 52:379–382
Ahmed E, Rabia N, Shumaila T, Hazem Z et al (2016) Sialolipoma of the superficial lobe of the parotid gland: a case report and literature review. Saudi J Med Med Sci 4(1):38–41
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khera, S., Elhence, P., Bagga, N. et al. Sialolipoma of Parotid Gland: a Lesser Known Entity. Indian J Surg 82, 90–92 (2020). https://doi.org/10.1007/s12262-019-01917-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-01917-0