Abstract
The aim of this study is to compare survival rates between right and left colon cancers following curative intent oncologic resection. The data of right- (between cecum and proximal two-thirds of the transverse colon) and left-sided (between distal one-third of the transverse colon and distal sigmoid colon) colon cancer patients, operated with curative intent including central vascular ligation between January 2005 and 2015, were recorded in a prospectively compiled database. Epidemiologic and clinical characteristics (laparoscopic resection, multivisceral resection, lymph node yield, metastatic lymph node yield, pathologic stage, duration of operation), early post-operative results, and overall 5-year survival rates were abstracted. A total of 426 patients were included. There were no differences in epidemiologic and clinical characteristics between two groups (p > 0.05), except a higher median lymph node yield in right-sided colon cancers (31 vs 24, p ˂ 0.001). Cox regression analysis identified no differences in overall 5-year survival rates between right (76.9%) and left colon (76.4%) cancers (p = 0.752). In right-sided colon cancer group, 5-year overall survival was significantly higher with laparoscopic resection (60.5% vs 78.9%, p = 0.008). There were no significant differences in left-sided colon cancer group per surgical approach (p = 0.357). Curative intent oncologic resection with central vascular ligation provided similar overall 5-year survival rates in right- vs left-sided colon cancers. Laparoscopic resection provided a significantly increased 5-year overall survival in right colon cancer group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, a trend for increased right-sided colonic cancer incidence was reported with an associated decrease in survival. A number of studies have demonstrated several different gene expressions comparing ascending and descending colon cancers [1,2,3]. This led to a classification of colonic cancer by subsite, i.e., the right- vs left-sided colon cancer, in order to distinguish different oncologic features and outcomes. This concept was analyzed in a number of studies demonstrating a worse prognosis in right colon cancer, whereas advanced age and female gender are also more frequently encountered in right colon cancer patients [4,5,6]. But, there are opposite articles in the literature. The results of a large-scale US database study demonstrated no survival difference between right- and left-sided colon cancers [7]. Another Japanese study reported no difference in disease free survival between right- and left-sided stage I–III colon cancer patients [8].
Because total mesorectal excision decreases local recurrence rate and increases overall survival rate, it has become a widely adopted concept in rectal cancer surgery and the similar technique has been recently recommended for colon cancer surgery. This includes ligating vascular structures at their origin and dissection through embryologic planes, which results in an increased lymph node harvest, decreased local recurrence, and increased survival from colon cancer as compared to standard hemicolectomy [9,10,11,12,13].
In our institution, the standard approach to colon cancer—open or laparoscopic resection—involves sharp dissection through embryologic planes and central vascular ligation in both right- and left-sided cancers. We hypothesized that this surgical approach can provide similar survival rates for both right- vs left-sided colonic cancers; and it can be performed laparoscopically with at least equal survival rates.
Methods
All colon cancer patients treated at our institution from January 2005 to January 2015 were recorded in a prospectively compiled database. After obtaining institutional review board approval epidemiologic (age, gender, body mass index), and clinical characteristics (laparoscopic resection, multivisceral resection, lymph node yield, metastatic lymph node yield, pathologic stage, duration of operation), early post-operative results and overall 5-year survival rates were abstracted. The study population was divided into right- and left-sided colon cancer groups retrospectively compared. For the purposes of this study, right-sided colon cancer was defined as located between caecum and proximal two-thirds of the transverse colon and left-sided colon cancer as located between distal one-third of the transverse colon and distal sigmoid colon. All operations were performed with curative intent including central vascular ligation (vascular ligation at the origin of the vessels) and through embryologic planes (Fig. 1).
In our institution, the standard of care for splenic flexure cancers is subtotal colectomy. Patients with stage IV cancers, patients who did not receive neoadjuvant therapy, patients with clinical findings of intestinal obstruction or perforation, patients diagnosed for synchronous or metachronous cancers, and those with positive surgical margins were excluded from this study. Neoadjuvant therapy in colon cancer is not the standard of care in our institution. All cases were discussed in a multidisciplinary oncology meeting, and adjuvant therapy was planned if the final pathology report reflected T3N+ or above in medically fit patients as examined by the medical oncology team. Overall survival was extracted from the national healthcare system records.
The cohorts of right- and left-sided colon tumors were compared for differences in epidemiologic (age > 65, gender, BMI > 30) and clinical characteristics (laparoscopic resection, multivisceral resection, lymph node yield, metastatic lymph nodes, total operating time [TOT], pathologic stage) using bivariate analysis. Chi-square or Fisher’s exact tests were used to compare categorical variables. Continuous variables were examined for normality of distribution using the Shapiro–Wilk test. Student’s t test was used for analysis of normally distributed variables and the non-parametric Mann–Whitney U test for analysis of values with a non-normal distribution.
The post-operative outcomes including mean initial flatus time, mean initial defecation time, mean initial oral feeding time, length of hospital stay (LOS), mean transfusion requirements, 30-day complications (including surgical site infections, prolonged ileus, anastomotic leak), 30-day mortality, and re-laparotomy rates were compared between the right- and left-sided colon cancers.
Overall 5-year survival was compared between right- and left-sided colon cancers using Mantel–Cox log-rank sum test. Cox proportional hazards regression model was performed to compare survival between the study groups after adjusting for clinically significant confounders.
The impact of surgical technique on survival was evaluated in right-sided and left-sided colon cancer groups. In our institution, the standard of care for colon cancer requiring multivisceral resection is by means of open surgery. To avoid a selection bias in favor of laparoscopic resection, patients with multivisceral resection were excluded and remaining patients were compared for epidemiologic, clinical, and pathologic characteristics. Overall 5-year survival was then compared using Mantel–Cox log rank sum test between open and laparoscopic resection pairwise within each strata. Cox proportional hazards regression model was used to compare survival between the study groups after adjusting for clinically significant confounders.
Results
A total of 426 patients were included into the study. There were no significant differences in age, gender, BMI, TOT, laparoscopic resection, and multivisceral resection between two groups (p > 0.05) (Table 1).
Pathologic T-stage, N-stage, metastatic lymph nodes, and pathologic stage were not significantly different between right- and left-sided colon cancer groups (p > 0.05), but median lymph node yield was greater in right-sided colon cancer group (p < 0.001) (Table 1). Histo-pathologic markers were not significantly different between right- and left-sided colon cancer groups (p > 0.05) (Table 1).
Post-operative outcomes were similar between the two groups, except initial flatus time and LOS (p = 0.049 and p = 0.002, respectively) (Table 1).
The median follow-up is 52 months. There were no differences in overall survival rates among right- vs left-sided colon cancer (p = 0.299) throughout the entire longitudinal follow-up. Cox regression analysis was performed to evaluate overall 5-year survival after adjusting for clinically relevant confounders (laparoscopic resection, multivisceral resection, T-stage, N-stage, pathologic stage), and no significant difference was observed (76.9% vs 76.4%, p = 0.752) (Table 2).
The impact of surgical technique on survival was evaluated in right- and left-sided colon cancer groups. To avoid a selection bias in favor of laparoscopic resection, patients with multivisceral resection (n = 14) were excluded and remaining patients were compared for epidemiologic, clinical, and pathologic characteristics. No significant differences were encountered between right- and left-sided colon cancer groups when compared per surgical approach (p > 0.05) (Table 3).
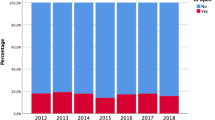
After adjusting for confounders (laparoscopic resection, T-stage, N-stage, pathologic stage), Cox regression proportional hazard model was used to evaluate whether the surgical technique affected survival in right- and left-sided colon cancer groups. In right-sided colon cancer group, 5-year overall survival was significantly higher with laparoscopic resection (60.5% vs 78.9%, p = 0.008). There were no significant differences in left-sided colon cancer group per surgical approach (p = 0.357) (Table 4; Fig. 1). Logistic regression analysis was performed separately to identify independent predictors of survival in each group. In right-sided colon cancer group, N-stage (AOR = 2.30 [1.59, 3.32], p < 0.001) and laparoscopic resection (AOR = 0.46 [0.26, 0.82], p = 0.008) were identified as independent predictors of survival.
Discussion
When each stratum was separately compared per surgical approach, laparoscopic resection was associated with a significantly increased overall 5-year survival in right-sided colon cancer (60.5% vs 78.9%, p = 0.008).
There is an increased incidence of microsatellite instability in right- and increased chromosomal instability in left-colon cancers, which confirm the heterogeneity and genetic differences between the two colonic segments [14]. There is a marked difference in colorectal cancer incidence in individuals who share a similar genetic inheritance but are living in different geographical areas. This has been proposed to underline the importance of lifestyle and dietary habits in colorectal cancer development in addition to genetic susceptibility [15]. Proximally located colon cancers have been reported with increased incidence of advanced stage, grade, and undifferentiated pathology. Higher cancer specific mortality rates were observed in proximal colon cancers [16]. In the present study, microsatellite or chromosomal instability analyses were not routinely performed. The various histopathologic markers analyzed—including lymphatic invasion, venous invasion, and tumor infiltrating lymphocytes—were not different among right- vs left-sided colon cancers (p > 0.05).
Right-sided colon cancer has been associated with decreased survival, which led to a proposal of dividing colonic cancer into two different entities by subsite. The first large-scale trial on this concept, by Meguid et al., analyzed the Surveillance, Epidemiology, and End Results Program (SEER) database from 1988 to 2003 encompassing 77.978 patients and demonstrated a worse prognosis in right colon cancer. Right colon cancers were associated with an increased incidence of advanced stage at presentation, advanced grade, and N2 status [4]. Interestingly, stage II right colon cancers had a better prognosis as compared to left colon cancers. Also, this study did include stage IV cancers, which renders the interpretation of survival data difficult. Similarly, Suttie et al. reported decreased survival for right-sided colon cancer after controlling for age, histological grade, and tumor stage and attributed these results to a more advanced stage at presentation and a lower curative resection rate in right-sided colon cancer [5]. In a recent study, right- vs left-sided colon cancer survival was compared in a large-scale German database. Right-sided colon cancers had a higher incidence of locally advanced disease and lymph node metastasis, though the cause of these differences was not clearly demonstrated. The different outcomes related to site were concluded as most likely related to environmental and genetic factors [6]. Weiss et al. analyzed SEER data from 1992 to 2005 including stage I–III colon cancer patients aged 66 years and older and reported that right-sided cancers had a preponderance of female gender, advanced age, and advanced stage [7]. Overall 5-year survival was similar between right- and left-sided colon cancers, though stage II right-sided cancers had lower mortality. Of note, at least half of colon resections in both groups retrieved less than 12 nodes (right-sided 55.7% vs left-sided 49.6%, p < 0.001), which raises concerns about the quality of oncologic resections. Moritani et al. studied recently the recurrence patterns of right- vs left-sided colon resections and reported no significant differences in the distribution of the first recurrence sites and disease free survival rates [8]. In contrast to the previous studies, there were no differences in epidemiological characteristics and pathologic stages between right- and left-sided colon cancers in the present study (p > 0.05). The utilization of screening colonoscopy, especially in low-income areas, varies significantly. The colonoscopy is usually delayed until symptoms become overt, which results in a late diagnosis of right-sided colon cancers as compared to left-sided lesions. This ultimately results in advanced stage and worse prognosis associated with right-sided colon cancers [16, 17]. In our country, the national healthcare system covers all individuals with free access to medical facilities. Although there was no screening program in place throughout the study period, colonoscopy is offered and performed without any charges to all patients who present to outpatient clinics with a suspicion of colon cancer. This may have resulted in a clearance of the abovementioned drawbacks against right colon tumors, which also may explain the indifferences regarding age, gender, and stage in right- and left-sided colon cancer patients.
Recent study also has demonstrated similar overall 5-year survival rates for right- and left-sided colon cancers (76.9% vs 76.4%, respectively, p = 0.752). Even though dissection of at least 12 lymph nodes is considered adequate in colon cancer staging, there is an established positive relation between increasing lymph node harvest and survival [18]. In the present study, following curative intent resection with central vascular ligation, median lymph node yield in right-sided colon cancers was greater than left-sided lesions (31 vs 24, p ˂ 0.001). The increased lymph node harvest associated with right-sided colon resections has probably also contributed to the relatively increased survival as compared to previous reports.
Through advancing technology and increasing demand by both patients and industry, laparoscopic surgery is becoming increasingly incorporated into surgical practice. At the beginning of 2000, laparoscopic colon resection was compared with open resection by a number of trials and pathologic, short-term clinical and oncological outcomes were reported similar with using both approaches [19,20,21]. Since 2010, the long-term outcomes of laparoscopic colorectal surgery have started to be published and these studies have confirmed the short-term outcomes of previous studies and have supported the fact that using laparoscopic surgery for colorectal cancer is safe and efficient [22, 23]. In 2009, Hohenberger et al. described the total mesocolic excision technique for colon cancer surgery, which is an analogue to the total mesorectal excision technique as described by Heald [9]. Hohenberger et al. reported a 7% increase in cancer-related 5-year survival of colon cancer after performing of complete mesocolic excision with central vascular ligation [10]. The median harvested lymph node using this technique was shown to be greater than the standard hemicolectomy (30 vs 18, p < 0.0001) [11]. After the introduction of complete mesocolic excision, the feasibility of the application of these principles in the laparoscopic setting remains controversial, especially in right colon cancer [10]. The trial conducted by West NP et al. has endorsed this finding. They have revealed that this dissection plane can be applied more easily in the left-sided resections than right-sided resections, and it improves 5-year survival, especially in stage III disease [24]. As described in detail by Acar et al. in their dynamic article from Ankara University, the development of this dissection plane requires particular caution and they indicate this technique may lead to achieve better outcomes in colon cancer patients [25]. In the present study, all colon resections were performed by six faculty members, who are experienced colorectal surgeons. We found no differences in lymph node harvest in right- and left-sided colon cancer strata between open vs laparoscopic resections (p > 0.05). The strata were comparable for TNM stages, and a significant survival benefit was observed in favor of laparoscopic resection in right-sided colon cancer group (60.5% vs 78.9%, p = 0.008). This increased survival in laparoscopy groups needs to be explained. The trial from Spain has represented lower acute phase systemic response with laparoscopic-assisted colectomy [26]. In the experimental animal study from Mayo Clinic, it has been concluded that systemic levels of proinflammatory cytokines and VEGF increase after laparotomy compared to laparoscopy, and they have been found to be associated with increased angiogenesis and tumor growth [27]. COLOR II trial revealed that laparoscopic surgery (LS) provides equal results as open surgery (OS) in terms of local recurrence and disease-free and overall survival for rectal cancer. Furthermore, they found better disease free survival with LS in patients who had stage III disease (LS 64.9% vs OS 52.0%) [28]. Lacy et al. reported same advantages of LS in lymph node–positive colon cancer patients. Both studies claim that causing less stress response and influencing immune functions lesser than OS are reasons for the survival benefit of LS [19, 28]. We believe that this increased survival in laparoscopic resection group is associated with its immunological effects and being less traumatic as Law et al. reported in their trial that laparoscopic colorectal surgery had positive effects not only on the short-term results but also on the general and disease-free survival rates [29]. When Cox regression proportional hazard regression model was used, N-stage (AOR = 2.30 [1.59, 3.32], p < 0.001) and laparoscopic resection (AOR = 0.46 [0.26, 0.82], p = 0.008) were identified as independent predictors of survival in the right-sided colon cancer group.
The major drawback associated with this study is by its retrospective nature. However, the right- and left-sided colon cancer patients were comparable for epidemiologic, clinical, and pathologic characteristics, which allow the analyses to be performed in a most possible homogenous population. The lack of disease free survival is the second disadvantage of the current study. Our institution is a tertiary referral center and at least half of the patients travelled from all over the country and were followed-up in institutions close their homes. This has restricted our access to the disease-free survival rates severely, but the overall survival data was extracted from the national healthcare system records, which are universally 100% reliable and accurate.
Conclusion
Following curative intent oncologic resection with central vascular ligation, lymph node yield was greater for right-sided colon tumors. Short-term post-operative outcomes were clinically comparable among both groups. When adjusted for clinically relevant confounders, 5-year overall survival rates were not different between right- and left-sided colon cancers. Laparoscopic resection provided a significantly increased 5-year overall survival in right colon cancer group.
References
Glebov OK, Rodriguez LM, Nakahara K, Jenkins J, Cliatt J, Humbyrd CJ, DeNobile J, Soballe P, Simon R, Wright G, Lynch P, Patterson S, Lynch H, Gallinger S, Buchbinder A, Gordon G, Hawk E, Kirsch IR (2003 Aug) Distinguishing right from left colon by the pattern of gene expression. Cancer Epidemiol Biomark Prev 12(8):755–762
Iacopetta B (2002) Are there two sides to colorectal cancer? Int J Cancer 101(5):403–408
Gatta G, Ciccolallo L, Capocaccia R, Coleman MP, Hakulinen T, Møller H, Berrino F, EUROCARE Working Group (2003) Differences in colorectal cancer survival between European and US populations: the importance of sub-site and morphology. Eur J Cancer 39(15):2214–2222
Meguid RA, Slidell MB, Wolfgang CL, Chang DC, Ahuja N (2008) Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol 15(9):2388–2394
Suttie SA, Shaikh I, Mullen R, Amin AI, Daniel T, Yalamarthi S (2011) Outcome of right- and left-sided colonic and rectal cancer following surgical resection. Color Dis 13(8):884–889
Benedix F, Kube R, Meyer F, Schmidt U, Gastinger I, Lippert H, Colon/Rectum Carcinomas (Primary Tumor) Study Group (2010) Comparison of 17,641 patients with right- and left-sided colon cancer: differences in epidemiology, perioperative course, histology, and survival. Dis Colon Rectum 53(1):57–64
Weiss JM, Pfau PR, O’Connor ES, King J, LoConte N, Kennedy G, Smith MA (2011) Mortality by stage for right- versus left-sided colon cancer: analysis of surveillance, epidemiology, and end results-Medicare data. J Clin Oncol 29(33):4401–4409
Moritani K, Hasegawa H, Okabayashi K, Ishii Y, Endo T, Kitagawa Y (2014) Difference in the recurrence rate between right- and left-sided colon cancer: a 17-year experience at a single institution. Surg Today 44(9):1685–1691
Heald RJ (1988) The ‘Holy Plane’ of rectal surgery. J R Soc Med 81(9):503–508
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation-technical notes and outcome. Color Dis 11(4):354–364
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28(2):272–278
Bokey EL, Chapuis PH, Dent OF, Mander BJ, Bissett IP, Newland RC (2003) Surgical technique and survival in patients having a curative resection for colon cancer. Dis Colon Rectum 46(7):860–866
Chen SL, Bilchik AJ (2007) Resecting lymph nodes in colon cancer: more than a staging operation? Ann Surg Oncol 14(8):2175–2176
Weiss JM, Schumacher J, Allen GO, Neuman H, Lange EO, Loconte NK, Greenberg CC, Smith MA (2014) Adjuvant chemotherapy for stage II right-sided and left-sided colon cancer: analysis of SEER-Medicare data. Ann Surg Oncol 21(6):1781–1791
Rozen P, Rosner G, Liphshitz I, Barchana M (2007) The changing incidence and sites of colorectal cancer in the Israeli Arab population and their clinical implications. Int J Cancer 120(1):147–151
Wray CM, Ziogas A, Hinojosa MW, Le H, Stamos MJ, Zell JA (2009) Tumor subsite location within the colon is prognostic for survival after colon cancer diagnosis. Dis Colon Rectum 52(8):1359–1366
Henry KA, Sherman RL, McDonald K, Johnson CJ, Lin G, Stroup AM, Boscoe FP (2014) Associations of census-tract poverty with subsite-specific colorectal cancer incidence rates and stage of disease at diagnosis in the United States. J Cancer Epidemiol 2014:823484
Bilimoria KY, Palis B, Stewart AK, Bentrem DJ, Freel AC, Sigurdson ER, Talamonti MS, Ko CY (2008) Impact of tumor location on nodal evaluation for colon cancer. Dis Colon Rectum 51(2):154–161
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
COST study group (2004) A Comparaison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Guillou PJ, Quirke P, Thorpe H (2005) Short term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet Oncol 365:1718–1726
Veldkamp R, Kuhry E, Hop WC, Colon Cancer Laparoscopic or Open Resection Study Group (2005) Laparoscopic surgery versus open surgery for colon cancer: shortterm outcomes of a randomised trial. Lancet Oncol 6:477–484
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97(11):1638–1645
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82
Açar Hİ, Cömert A, Avşar A, Çelik S, Kuzu MA (2014) Dynamic article: surgical anatomical planes for complete mesocolic excision and applied vascular anatomy of the right colon. Dis Colon Rectum 57(10):1169–1175
Delgado S, Lacy AM, Filella X, Castells A, Garcia-Valdecasas JC, Pique JM, Momblan D, Visa J (2001) Acute phase response in laparoscopic and open colectomy in colon cancer: randomized study. Dis Colon Rectum 44:638–646
Pera M, Nelson H, Rajkumar SV, Young-Fadok TM, Burgart LJ (2003) Influence of postoperative acute-phase response on angiogenesis and tumor growth: open vs. laparoscopic-assisted surgery in mice. J Gastrointest Surg 7:783–790
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, COLOR II Study Group (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Law WL, Poon JT, Fan JK, Lo OS (2012) Survival following laparoscopic versus open resection for colorectal cancer. Int J Color Dis 27:1077–1085
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Keskin, M., Sivrikoz, E., Yeğen, G. et al. Right vs Left Colon Cancers Have Comparable Survival: a Decade’s Experience. Indian J Surg 82, 134–141 (2020). https://doi.org/10.1007/s12262-019-01900-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-01900-9