Abstract
The applicability of single-incision laparoscopic colectomy (SILC) for descending colon cancer is poorly understood. In the present study, consecutive experiences with SILC for descending colon cancer are reviewed, and its long-term clinical and oncological outcomes are evaluated. A single institutional experience of SILC for descending colon cancer is presented. Thirty patients (13 women) with a median age of 68.7 years and a median body mass index of 23.0 kg/m2 were treated with SILC for clinically diagnosed colon cancer between January 2011 and December 2015. We performed left hemicolectomy in patients whose tumor located at the splenic flexure, and selected descending colectomy in the other patients. There were no conversions and additional port insertion. The mean skin incision length was 2.89 cm. The mean operative time and blood loss were 184.7 min and 72.5 mL, respectively. The mean number of harvested lymph nodes was 18.8. The 5-year relapse-free survival for stage I, stage II, and stage III disease was 100%, 70.0%, and 67.3%, respectively. The 5-year overall survival for stage I, stage II, and stage III disease was 100%, 72.0%, and 67.3%, respectively. Our initial experiences showed that SILC can be applied to the treatment of descending colon cancer with good long-term clinical and oncological outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the oncologic safety of laparoscopic colectomy in cancer patients has been proven in randomized trials [1], laparoscopic surgery has steadily become a safe and practical treatment option for these patients, even those with malignant disease of the colon.
Single-incision laparoscopic colectomy (SILC) is a challenging procedure. Although it seems to be safe and feasible, there is insufficient clinical evidence to confirm this. Watanabe J et al. [2] reported that there was no difference in the number of lymph nodes dissected between the SILC and conventional multiport laparoscopic procedures in their randomized clinical trial. We started with SILC in December 2010 for colon cancer after having experience with hybrid single-incision laparoscopic procedure using the techniques of open surgery through the small incision [3].
Descending colon cancer has a complicated lymphoid system draining to the superior mesenteric artery and the inferior mesenteric artery. In reported studies about the oncological outcome of laparoscopic colectomy, descending colon cancer was frequently excluded because of its complicated lymphatic flow and the difficulty of its procedure [4]. There are no articles about the feasibility of SILC for descending colon cancer. In the present study, our consecutive experiences with SILC for descending colon cancer are reviewed, and its long-term clinical and oncological outcomes are evaluated.
Materials and Methods
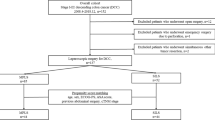
A consecutive experience of SILC for descending colon cancer is presented. Thirty patients (13 women) with a median age of 68.7 years (range, 50–85 years) and a median body mass index of 23.0 kg/m2 (range, 14.5–32.7 kg/m2) were treated with SILC between January 2011 and December 2015. Sixteen patients (53.3%) had undergone prior abdominal surgery (3 appendectomies, 3 gastrectomies, 2 colorectal resections, 2 gynecological surgeries, 2 cholecystectomies, 2 cesarean sections, and 2 other surgeries) (Table 1). In all the cases, patient’s consent for SILC was obtained. We performed left hemicolectomy in patients whose tumor located at the splenic flexure, and descending colectomy in the other patients.
Surgical Procedures
Patient Positioning and Access in the EZ-Access Method
Under general anesthesia, the patients were placed in the modified lithotomy position. First, a Lap protector (LP; Hakkou Shoji, Japan) was inserted through a 2.5-cm transumbilical incision, which protected the wound. Next, an EZ-access (Hakkou Shoji, Japan) was mounted onto the LP, and three ports were made in the EZ-access. Almost all procedures were performed with standard laparoscopic instruments, and the operative procedures were similar to those employed in the standard laparoscopic colectomy procedure using a flexible scope.
Left Hemicolectomy
First, resection of soft tissues around the inferior mesenteric artery including lymph nodes was performed. The left colic artery was identified, and proximal ligations of this vessel were performed. The mesentery of the descending colon was gently mobilized by the median-to-lateral approach, and resection of the lateral side was performed beyond Gerota’s fascia to the left abdominal wall. The lymph node dissection around the mid colic artery and its left branch area was performed, and the left branch was ligated. The omental bursa was entered, and the mesentery of the transverse colon was dissected from the inferior border of the pancreas. The transverse or descending colon was delivered through a Lap protector, and the anastomosis was performed extracorporeally using the functional end-to-end method. The anastomotic site is returned to the peritoneal cavity.
Results
We adopted single-incision laparoscopic colectomy for descending colon cancer in 30 patients. Twenty-three descending colectomies and seven left hemicolectomies were performed in this series. There were no conversions and additional port insertion (Table 1). The mean skin incision length was 2.89 cm (range, 2–5 cm). The mean operative time and blood loss were 184.7 min (range, 96–350 min) and 72.5 mL (range, 1–340 mL), respectively. The mean number of harvested lymph nodes was 18.8. The pathological stages included stage 0 (n = 1), stage I (n = 5), stage II (n = 10), stage III (n = 11), and stage IV (n = 3). Early post-operative complications occurred only in one patient with intraperitoneal abscess (3.3%). Late post-operative complications occurred in four patients (13.3%). There were three incisional hernias and a small bowel obstruction. The patients were discharged after a mean period of 12.0 posto-perative days. Three (11.5%) tumor recurrence or metastases occurred in 26 patients with stage I to stage III disease with the median follow-up of 64 months (Table 2). One peritoneal seeding occurred in T4 cancer patient in 7 months after operation, and he died 48 months after recurrence; one liver metastasis occurred in patient with stage II disease 7 months after operation, and she died 8 months after recurrence. One lung metastasis occurred in patient with stage II disease 13 months after operation, and she live after metastasectomy. Three non-cancer-related deaths were noted in stage III cancer patients. The 5-year relapse-free survival for stage I, stage II, and stage III disease was 100%, 70.0%, and 67.3%, respectively (Fig. 1). The 5-year overall survival for stage I, stage II, and stage III disease was 100%, 72.0%, and 67.3%, respectively (Fig. 2).
Discussion
Single-incision laparoscopic colectomy (SILC) has emerged as a new generation of laparoscopic colorectal surgery that is akin to conventional surgery with the added benefit of better cosmesis. This procedure for colon cancer was first described by Bucher P et al. [5] and Remzi FH et al. [6] in 2008. Many authors have reported that SILC provides a better cosmetic result with similar perioperative results [7]. Our review with a total of 15 studies with 589 patients who underwent SILC for colorectal cancer showed no significant differences between the SILC and conventional laparoscopic colectomy in terms of short-term clinical and oncological outcomes [8].
Yamamoto et al. [4] reported that there are some difficulties in laparoscopic resection for descending colon cancer in terms of mobilization, extent of resection, and lymphadenectomy according to the location of the tumor. In addition, resection of descending colon cancer may result in major complications in case of dissection in the wrong plane because descending colon is adjacent to critical structures including the pancreas, duodenum, spleen, and the base of the inferior mesenteric vein. Therefore, descending colectomy and left colectomy are more difficult even in conventional laparoscopic procedure which often limits its use for the descending colon cancer. SILC is thought to be a challenging procedure because of its procedural difficulty over conventional laparoscopic colectomy. It is a natural consequence that there are no articles about the feasibility of SILC focused on descending colon cancer.
In this study, we presented about 30 descending colon cancer patients with the median follow-up period of 64 months. They were consecutive patients from the introduction of SILS in our hospital. These data include bad outcomes which were derived from inadequate procedures of learning phase; therefore, we believe that our study indicates the practical outcome of SILS in a community hospital setting. To our knowledge, the present study is the first study presenting adequate long-term cancer outcomes with SILS for descending colon cancer. The 5-year RFS and OS in this study were comparable to CLS from the aspect of these rates with its long follow-up period, which allows us to conclude the long-term oncological safety of SILS for descending colon cancer.
Concerning about the hospitalization, our patients stayed in our hospital for 12.0 days after operation. This is mainly owing to the healthcare system in Japan. The health care expenditure is inexpensive in our country. In this series, we could treat non-selective descending colon cancer patients with the mean 2.89-cm skin incision and mean 72.5-mL blood loss without increasing morbidity.
Our study has several limitations, including its retrospective nature and the data for SILC versus conventional multiport laparoscopic colectomy. Our initial experiences showed that SILC can be applied to the treatment of descending colon cancer in community hospital setting with good long-term oncological outcomes. Further trials are necessary to prove that it has non-cosmetic advantages over conventional laparoscopic colectomy.
References
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Watanabe J, Ota M, Fujii S, Suwa H, Ishibe A, Endo I (2016) Randomized clinical trial of single-incision versus multiport laparoscopic colectomy. Br J Surg 103:1276–1281
Hirano Y, Hattori M, Kitamura H, Maeda K, Douden K, Hashizume Y (2011) Hybrid single-incision laparoscopic sigmoidectomy: the effective use of small incision. J Laparoendosc Adv Surg Tech A 21:625–627
Yamamoto M, Okuda J, Tanaka K, Kondo K, Tanigawa N, Uchiyama K (2012) Clinical outcomes of laparoscopic surgery for advanced transverse and descending colon cancer: a single-center experience. Surg Endosc 26:1566–1572
Bucher P, Pugin F, Morel P (2008) Single port access laparoscopic right hemicolectomy. Int J Color Dis 23:1013–1016
Remzi FH, Kirat HT, Kaouk JH, Geisler DP (2008) Single-port laparoscopy in colorectal surgery. Color Dis 10:823–826
Makino T, Milsom JW, Lee SW (2012) Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg 255:667–676
Hirano Y, Hattori M, Douden K, Ishiyama Y, Hashizume Y (2016) Single-incision laparoscopic surgery for colorectal cancer. World J Gastrointest Surg 27(8):95–100
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statements
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Hirano, Y., Shimada, M., Kato, K. et al. Single-Incision Laparoscopic Colectomy for Descending Colon Cancer: a Single Institutional Experience. Indian J Surg 81, 350–353 (2019). https://doi.org/10.1007/s12262-018-1818-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1818-0