Abstract
Mesothelioma is a malignant tumor that involves mesothelial cells that normally line the body cavities, including the pleura, peritoneum, pericardium, and testis. Testicular mesothelioma (TM) is a rare type of mesothelioma that affects tunica vaginalis, tunica albuginea, spermatic cord, and the epididymis. The frequency of TM is unknown; however, fewer than 100 cases have been reported across the world. A 47-year old male presented with a painless scrotal swelling of 3-month duration with no history of testicular trauma or any inflammatory manifestations. Clinical and sonographic examination revealed right-sided scrotal hydrocele. The patient was scheduled for subtotal excision of the tunica vaginalis. During surgery, the surgeon observed multiple variable-sized suspicious nodules on the visceral surface of the tunica vaginalis. Upon excision of the tunica vaginalis, the specimen was sent for histopathologic examination which concluded the diagnosis of malignant mesothelioma of the tunica vaginalis. Complete metastatic work-up was performed, and no metastatic deposits were identified. The patient then underwent high inguinal orchiectomy which revealed residual mesothelioma in the remaining parts of tunica vaginalis and epididymal area, yet the testis and spermatic cord were free of malignancy. TM, although a rare entity, should be included in the differential diagnosis of scrotal and testicular complaints. Careful assessment of the tunica vaginalis during scrotal and testicular surgery is crucial since TM can be incidentally discovered during surgery. Histopathologic examination of any suspicious lesion in the tunica vaginalis is imperative to exclude malignant mesothelioma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mesothelioma is a malignant tumor of the mesothelial cells that normally line the body cavities, including the pleura, peritoneum, pericardium, and testis. Approximately 87% of primary malignant mesotheliomas affect the pleural membrane [1].
Testicular mesothelioma (TM) is a rare type of mesothelioma that affects tunica vaginalis, tunica albuginea, spermatic cord, and the epididymis. The frequency of TM is unknown; however, fewer than 100 cases have been reported across the world since the first case has been reported [2].
The predisposing factors for TM remain unclear. Exposure to asbestos, testicular trauma, and long-standing hydrocele were suggested to contribute to the pathogenesis of TM [3]. The majority of patients with TM present with non-specific symptoms such as painless testicular lump or hydrocele. Although preoperative ultrasonography and CT scanning can be helpful in identifying TM, the diagnosis is usually made after histopathologic examination of the excised tunica vaginalis.
Case Presentation
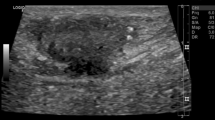
A 47-year old male presented with a painless scrotal swelling of 3-month duration. The patient denied any history of testicular trauma or inflammatory manifestations preceding the onset of the swelling. On examination, a right-sided scrotal hydrocele measuring around 12 × 8 cm in size was found. The other side of the scrotum was normal, and both testes were normal in size and shape with intact testicular sensation. Scrotal ultrasonography revealed right-sided infected hydrocele with normal appearance of the right testis and epididymis.
The patient was scheduled for subtotal excision of tunica vaginalis. Under spinal anesthesia, a scrotal incision was made at the lower half of the right side of the scrotum, then dissection was carried out until the tunica vaginalis was identified. A small incision was made in the tunica vaginalis, and the collected clear fluid was evacuated. The incision in the tunica vaginalis was enlarged to deliver the testis outside. Then on excision of the tunica vaginalis, multiple variable-sized nodules were noted on the visceral surface of tunica vaginalis (Fig. 1). After excision of the tunica vaginalis, a rubber drain was inserted and the wound was closed in layers.
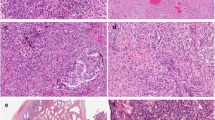
The excised tunica vaginalis was sent for histopathologic examination which revealed multiple foci of tumor tissue within normal tunical structure. The tumor composed of tubule-papillary structures with solid sheets of large polygonal cells with ample cytoplasm and large vesicular nuclei with prominent nucleoli (Fig. 2). Frequent mitosis was also observed. On immunohistochemical staining, the specimen was positive to calretinin, WT-1, and vimentin and negative to cytokeratin and Melan A. A final diagnosis of malignant mesothelioma of the tunica vaginalis was made.
The patient was informed of the diagnosis and had CT scanning of the chest, abdomen, and pelvis which revealed no pulmonary or abdominal metastatic deposits. Bone scan was also conducted and revealed no metastatic bony lesions. The patient underwent high inguinal orchiectomy, and the resected specimen was sent for histopathologic examination that revealed residual mesothelioma in the remaining parts of tunica vaginalis and epididymal area, yet the testis and spermatic cord were free of malignancy. An informed consent for publication of this case report was obtained from the patient.
Discussion
TM is a rare condition that usually affects patients aging between 55 and 75 years. Although the patient in the present report was younger than the reported range, TM can occur at even younger ages as around 10% of patients are younger than 25 years [4].
Peterson et al. [5] explained TM with no history of asbestos exposure to be associated with chronic inflammation and long-standing hydrocele. The patient in this report presented with hydrocele of 3-month duration only in contrast to the previous reports that documented long-standing hydrocele in patients with TM.
The patient in this report did not show any alarming clinical or radiologic signs, but the suspicion of specific pathology of the tunica vaginalis was raised intraoperatively after observing multiple variable-size nodules. The final diagnosis was made after histopathologic examination of the resected tunica vaginalis which highlights the importance of routine pathologic examination of tunica vaginalis in testicular and scrotal surgery.
Treatment of patients with localized TM involves radical inguinal orchiectomy as the standard surgical procedure. Inguinal lymph node dissection should be combined with high inguinal orchiectomy if there was evidence of metastasis in the inguinal lymph nodes. If no metastatic deposits were identified on metastatic work-up, adjuvant chemotherapy and radiotherapy are not required [6]. Since the patient in the present report did not exhibit any signs of lymph node or distant metastasis, he did not receive adjuvant treatment.
Conclusion
TM, although a rare entity, should be included in the differential diagnosis of scrotal and testicular complaints. Careful assessment of the tunica vaginalis during scrotal and testicular surgery is crucial since TM can be incidentally discovered during surgery. Histopathologic examination of any suspicious lesion in the tunica vaginalis is imperative to exclude malignant mesothelioma.
References
Hodgson JT, Darnton A (2000) The quantitative risks of mesothelioma and lung cancer in relation to asbestos exposure. Ann Occup Hyg 44(8):565–601
Barbera V, Rubino M (1957) Papillary mesothelioma of the tunica vaginalis. Cancer 10:183–189. https://doi.org/10.1002/1097-0142(195701/02)10:1<183::AID-CNCR2820100127>3.0.CO;2-1
Yen C-H, Lee C-T, Su C-J, Lo H-C (2012) Malignant mesothelioma of the tunica vaginalis testis: a malignancy associated with recurrent epididymitis? World J Surg Oncol 10:238. https://doi.org/10.1186/1477-7819-10-238
Plas E, Riedl CR, Pfluger H (1998) Malignant mesothelioma of the tunica vaginalis testis: review of the literature and assessment of prognostic parameters. Cancer 83:2437–2446
Peterson JT Jr, Greenberg SD, Buffler PA (1984) Non-asbestos-related malignant mesothelioma. a review. Cancer 54:951–960
Ceresoli GL, Zucali PA, Favaretto AG, Grossi F, Bidoli P, del Conte G, Ceribelli A, Bearz A, Morenghi E, Cavina R, Marangolo M, Parra HJS, Santoro A (2006) Phase II study of pemetrexed plus carboplatin in malignant pleural mesothelioma. J Clin Oncol 24:1443–1448
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection, writing, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Emile, S.H., Balata, M., Elfallal, A.H. et al. Malignant Mesothelioma of the Tunica Vaginalis: Incidental Diagnosis of a Rare Condition. Indian J Surg 81, 80–82 (2019). https://doi.org/10.1007/s12262-018-1778-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1778-4