Abstract
The liver is the most commonly injured organ following trauma. Management of liver trauma has shifted away from surgical intervention towards non-operative management (NOM), and with careful observation, regular re-examination and utilisation of interventional radiological services, there has been an improvement in outcomes. Mortality following liver trauma is quoted at 10–15%. Patients admitted between 1st January 2009 and 31st December 2014 were identified via our Trauma Audit and Research Network (TARN) officer and from CT scan reports containing the words biloma, contusion, laceration and trauma. Liver injuries were graded by a consultant radiologist using the AAST scale. Information on interventions and outcomes was gathered from a combination of TARN data and case note review. Eighty-eight patients were identified with a median age of 26 (2–71). Fifty-one patients (58%) were male. Incidence peaked in the third decade with both men and women. Median ISS was 22 (4–59). Blunt trauma was the cause in 76 (86%) of the patients. Seven patients died prior to scanning or laparotomy. Eighteen patients required laparotomy; the remaining 63 patients were managed non-operatively. Overall mortality was 13.6%—all fatalities occurring within the blunt trauma group. Mortality following laparotomy was 22% and higher in males (15.7 vs 10.8%). Non-operative management (NOM) for liver trauma is well established at our hospital. Our mortality rate is comparable to larger series. A blunt mechanism of injury and the need for surgical intervention both represent poor prognostic factors in patients with liver trauma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the largest solid organ in the body, the liver is the most frequently injured abdominal organ. Despite the relative protection it receives from the lower half of the bony chest, it is still vulnerable to injury from both blunt and penetrating forces. In the UK, the incidence of liver trauma is around 2.4 per 100,000 [1], with the majority of injuries to the liver resulting from blunt trauma (either deceleration or crush). In the USA and South Africa, penetrating trauma has a higher incidence. There has been a major paradigm shift in the management of liver trauma over the last three decades, with the movement away from mandatory laparotomy and packing of liver injuries, heading towards a selective non-operative approach. During the evolution of non-operative management, the inclusion criteria has broadened so that now it is widely accepted that provided the patient is haemodynamically stable, has a minimal transfusion requirement and has no evidence of generalised peritonitis, a non-operative strategy can be attempted, regardless of the grade of injury [2,3,4,5].
The American Association for the Surgery of Trauma (AAST) Liver Injury Scale is the most widely used grading system for hepatic trauma. Since its development, it has been a useful tool in stratifying patients with correlation to their risk of morbidity and mortality (Table 2).
The advent of conservative management for liver trauma has given rise to a different group of complications which may present in a variety of ways and at varied times following the initial injury—predominantly of a septic and haemorrhagic nature. Complications such as pseudoaneurysm formation (Fig. 1) and biliary injuries may initially be asymptomatic, but may have potentially fatal sequelae. Due to the potentially catastrophic nature of these complications, it is the protocol at the Cardiff Liver Unit that all patients who are admitted with a grade III or greater liver injury should undergo a routine CT scan of the abdomen and pelvis at day 10 following the injury with a specific goal of detecting these serious complications in asymptomatic patients. There are conflicting studies on whether early re-scanning (i.e. prior to discharge) of such patients is required [7, 8]. In Cardiff, we feel that detection of complications such as pseudoaneurysms in a timely manner allows intervention in a safer, more elective setting, preferably using interventional radiology services.
The Cardiff Liver Unit is a regional Hepatobiliary centre serving a local population of approximately 450,000 [9] from the Cardiff and Vale of Glamorgan area, as well as being a tertiary referral centre, accepting patients from the whole of South and Mid Wales.
The protocol we follow in Cardiff (Table 3) for all patients admitted with a Grade 3 liver injury or more severe allows us to standardise our care.
We reviewed the management and outcomes of patients admitted to our hospital having suffered a traumatic injury to the liver.
Methods
This was a retrospective study looking at all patients admitted to the University Hospital of Wales over a 6-year period. Two separate methods were used to identify appropriate patients. Firstly, a request was made to the TARN (Trauma Audit and Research Network) to identify all patients labelled as having been admitted to UHW with a liver injury between 2009 and 2014. Secondly, a search was made on the hospital radiology system to identify all patients who underwent a CT scan in which the report or request included the word “trauma”, “contusion”, “biloma” or “laceration”. Every CT report was read and assessed to identify whether the patient had a traumatic liver injury. Iatrogenic hepatobiliary injuries and incidental findings without a recognised acute injury were not included in this study. On a few scans, there was doubt whether a feature on the CT reflected a true injury or a perfusion artefact along the falciform ligament—these scans were not included in the study.
Once appropriate patients were identified, medical records and TARN data were interrogated to extract the necessary data regarding demographics, need for surgery/interventional radiology and outcome. Admission CT scans were reviewed by a consultant radiologist to provide a liver injury grade. Information regarding interventions (radiological or surgical) and outcomes was obtained from the hospital clinical portal and patient notes.
Results
Between January 1st 2009 and December 31st 2014, 88 patients were admitted to the University Hospital of Wales in Cardiff with a recorded liver injury. Fifty-four (61%) were admitted directly to UHW, with the remaining 34 (39%) patients being transferred in from other hospitals in South Wales.
The median age of patients was 26 (2–71), with 51 (58%) being male. Median International Severity Score (ISS) of all patients was 22 (4–59). Men were more than twice as likely to have suffered from penetrating trauma compared to women (17 vs 8%), and this in the main stay was due to stabbings.
Overall mortality in our cohort was 13.6%, with seven of the 88 patients (8%) of patients dying before arriving in hospital or in the resuscitation department. When split by gender, the mortality amongst males was higher, at 15.7% compared to 10.8% amongst female patients.
Interestingly the mortality was much higher in the patients admitted directly to UHW compared to patients transferred (18 vs 6%), though this is likely to represent the fact that many of these patients had multiple injuries requiring other tertiary specialties at our hospital (i.e. cardiothoracics and neurosurgery) (Tables 1, 2 and 3).
Blunt vs Penetrating
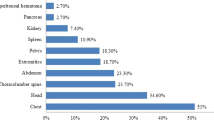
The majority of liver injuries in our cohort was sustained by a blunt mechanism of action. The most common causes of which were road traffic collisions followed by falls from height. The commonest cause of penetrating injuries was stabbing (including self-harm). The overall split of blunt trauma to penetrating trauma was 86 to 14%. This remained the case when we looked at the mechanism of injury per gender. Median ISS was notably higher in the blunt trauma group compared to the penetrating trauma group, representing the more complex and multi-organ involvement of blunt injuries. Mechanism of injury was directly related to mortality, with all of the fatalities occurring in the blunt trauma group.
NOM vs Intervention
Of the 88 patients, seven died in the emergency department prior to definitive management. Of the 81 who survived long enough to have a management plan put in place, 63 (77%) were managed with a non-operative approach with the remaining 18 patients undergoing a laparotomy or laparoscopy as part of their initial management. No patients subsequently failed non-operative management. Operative intervention was more common in the penetrating trauma group compared to the blunt trauma cohort (42 vs 19%). The majority of patients who underwent laparotomy was managed with simple packing, though two patients underwent resectional debridement, one patient underwent suture of the laceration whilst one patient underwent a formal anatomical resection (following previous damage control surgery at a local district general hospital). The mortality was much higher amongst our patients who underwent laparotomy (22%) when compared to those managed non-operatively (1.6%). This difference was statistically different.
Discussion
Role of Non-operative Management
The shift in the management of adult liver trauma away from mandatory laparotomy coupled with techniques such as hepatic artery ligation and resectional debridement [10] can be traced back to the early mid 1980s. The initial reports of conservative, non-operative management of initially splenic [11] and then liver injuries [12] in children led to the realisation that adult trauma victims could be potentially managed in this way. The selection criteria for such management has broadened since Meyer [13] published the seminal paper in 1985, although the key features of lack of peritoneal signs, haemodynamic stability and the absence of other significant intra-abdominal injuries have remained critical in selecting which patients should have a trial of non-operative management and which should go straight to the operating theatre. The initial criterion of a simple liver injury with < 125 ml of intra-peritoneal blood has now expanded to include all grades of liver injury dependent on haemodynamic stability of the patient [5]. Our data concurs with contemporary data that the majority of patients admitted following liver trauma can be managed non-operatively with satisfactory outcomes [14].
With the increasing utilisation of non-operative management, it is important to emphasise that there will always be a role for operative management of a subset of patients who do not respond to initial resuscitation. Although peri-hepatic packing is often the only liver-related surgical intervention required in the majority of patients undergoing surgical intervention, other techniques such as debridement resection, suture repair of laceration and anatomical resection can be utilised when required [15].
“The Cardiff Protocol” and Routine Rescanning of Asymptomatic Patients with Severe Liver Injuries
Much debate exists regarding the role of routine short-term follow-up scanning of patients admitted with a liver injury. Whilst many authors including Cox [8] and Parks [16] advocate that routine inpatient scanning is unnecessary, Demetriades’ [7] data supports routine Day 10 scanning with a finding of a complication rate of 23% (4/17) amongst asymptomatic patients. In Cardiff, we follow the Demetriades mantra, in that all patients admitted with a significant liver injury (grade 3 or greater) undergo routine CT scanning at Day 10 to exclude the presence of a potentially fatal complication. In our cohort, five asymptomatic patients had CT scans which revealed complications requiring intervention; three pseudoaneurysms requiring embolization and two bilomas treated with radiologically guided percutaneous drainage and ERCP. These patients made good recoveries with no long-term sequelae related to their injury. Given the ease of access to high-quality CT scanning coupled with the potential threat to life of a missed pseudo-aneurysm and the morbidity associated with laparotomy and open repair of such a complication, we cannot justify not routinely scanning these patients.
Comparison to Other Series
Our overall mortality of 13.6% is comparable to other published series [1, 17,18,19,20,21]. Our data also agrees with other case series that males are more commonly affected by liver trauma [22] and that blunt trauma is a poor prognostic factor, with all our fatalities occurring in the blunt trauma group. The statistically significant increase in mortality seen in the group of patients requiring operative intervention is most likely to represent the polytrauma nature of their injuries.
References
Scollay JM, Beard D, Smith R, McKeown D, Garden OJ, Parks R (2004) Eleven years of liver trauma: the Scottish experience. Br J Surg 91(Suppl1):24
Sherman HF, Savage BA, Jones LM, Barrette LM, Latenser BA, Varcelotti JR et al (1994) Non-operative management of blunt hepatic injuries: safe at any grade? J Trauma 37(4):616–621. https://doi.org/10.1097/00005373-199410000-00015
Croce MA, Fabian TC, Menke PG, Waddle-Smith L, Minard G, Kudsk KA, Patton Jr JH, Schurr MJ, Pritchard FE, ‘Nonoperative management of blunt hepatic trauma is the treatment of choice for haemodynamically stable patients. Results of a prospective trial,Ann Surg 1995; 221:744–753, 6, DOI: https://doi.org/10.1097/00000658-199506000-00013
Van Der Wilden GM, Velmahos GC Emhoff T, Brancato S, Adams C, Georgakis G et al (2012) Successful nonoperative management of the most severe blunt liver injuries: a multicenter study of the research consortium of New England centers for trauma. Arch Surg 147:428–429
McVay MR, Kokoska ER, Jackson RJ, Smith SD (2008) Throwing out the “grade” book: management of isolated spleen and liver injury based on haemodynamic stability. J Pediatr Surg 43(6):1072–1076. https://doi.org/10.1016/j.jpedsurg.2008.02.031
Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR (1995) Organ injury scaling: spleen and liver (1994 revision). J Trauma 38(3):323–324. https://doi.org/10.1097/00005373-199503000-00001
Demetriades D, Karaiskakis M, Alo K, Velmahos G, Murray J, Asensio J (2003) Role of postoperative computed tomography in patients with severe liver injury. Br J Surg 90(11):1398–1400. https://doi.org/10.1002/bjs.4312
Cox JC, Fanian TC, Maish GO, Bee TK, Pritchard FE, Russ SE et al (2005) Routine follow up imaging is unnesecary in the management of blunt hepatic injury. J Trauma 59:1175–1180
Office for National Statistics, www.ons.gov.uk
Flint LM, Mays ET, Aaron WS, Fulton RS, Polk HC (1977) Selectivity in the management of liver trauma. Ann Surg 185(6):613–618. https://doi.org/10.1097/00000658-197706000-00001
Aronson DZ, Scherz AW, Einhorn AH, Becker JM, Schneider KM (1977) Nonoperative management of splenic trauma in children: a report of six consecutive cases. Pediatrics 60(4):482–485
Karp MP, Cooney DR, Pros GA, Newman BM, Jewett Jr TC (1983) The nonoperative management of pediatric hepatic trauma. J Pediatr Surg 18(4):512–518. https://doi.org/10.1016/S0022-3468(83)80211-5
Meyer AA, Crass RA, Lim RC Jr, Jeffrey RB, Federle MP, Trunkey DD (1985) Selective non-operative management of blunt liver injury using computed tomography. Arch Surg 120:781–784
Clemente N, Di Saverio S, Giorgini E, Biscardi A, Villani S, Senatore G, Filicori F, Antonacci N, Baldoni F, Tugnoli G (2011) Management and outcome of 308 cases of liver trauma in bologna trauma Centre in 10 years. Ann Ital Chir 82(5):351–359
Polanco P, Leon S, Pineda J, Puyana JC, Ochoa JB, Alarcon L, Harbrecht BG, Geller D, Peitzman AB (2008) Hepatic resection in the management of complex injury to the liver. J Trauma 65(6):1264–1269. https://doi.org/10.1097/TA.0b013e3181904749
Parks RW Hepatobiliary and pancreatic trauma. In: Garden OJ, Parks RW (eds) A Companion to Specialist Surgical Practice: Hepatobiliary and Pancreatic Surgery, 5th edn, Saunders Elselvier 304–325
Feliciano DV, Mattox KL, Jordan GL Jr, Burch JM, Bitondo CG, Cruse PA (1986) Management of 1000 consecutive cases of hepatic trauma (1979–84). Ann Surg 204(4):438–454. https://doi.org/10.1097/00000658-198610000-00012
Schweizer W, Tanner S, Baer HU, Lerut J, Huber A, Gertsch P, Blumgart LH (1993) Management of traumatic liver injuries. Br J Surg 80(1):86–88. https://doi.org/10.1002/bjs.1800800128
Aldrete JS, Halpern NB, Ward S, Wright JO (1979) Factors determining morbidity and mortality in hepatic injuries., Analysis of 108 cases. Ann Surg 189(4):466–474
Gür S, Orsel A, Atahan K, Hökmez A, Tarcan E (2003) Surgical treatment of liver trauma (analysis of 244 patients). Hepato-Gastroenterology 50:2109–2011
Prichayudh S, Sirinawin C, Sriussadaporn S, Pak-art R, Kritayakirana K, Samorn P (2014) Management of liver injuries: predictors for the need of operation and damage control surgery. Injury 45(9):1373–1377. https://doi.org/10.1016/j.injury.2014.02.013
Saleh AF, Al Sageer E, Elheny A (2016) Management of liver trauma in Minia University Hospital Egypt. Indian J Surg 78(6):442–447. https://doi.org/10.1007/s12262-015-1393-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mortimer, M.C.M., Parry, C. & Kumar, N. Liver Trauma in South Wales: the Cardiff Protocol. Indian J Surg 81, 119–123 (2019). https://doi.org/10.1007/s12262-018-1740-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-018-1740-5