Abstract
The aims of this retrospective study were to consider the diagnostic role of dual-time 18F-fluorodeoxyglucose positron emission tomography and computed tomography (18F-FDG PET/CT) in detection of breast carcinoma and axillary lymph node (ALN) status and to evaluate the primary tumor 18F-FDG uptake pattern. Preoperative staging was performed by 18F-FDG PET/CT in 78 female patients with breast carcinoma. Conventional imaging results were evaluated by breast magnetic resonance imaging (MRI) of 79 lesions in 78 patients, bilateral mammography (MMG) of 40 lesions in 40 patients, and breast ultrasonography (USG) of 47 lesions in 46 patients. The primary tumor detection rate using 18F-FDG PET/CT was higher than those using MRI, USG, and MMG. The sensitivity and specificity of 18F-FDG PET/CT scans for detecting multifocality were higher than those of MRI. The specificity of ALN metastasis detection with MRI was higher than that with 18F-FDG PET/CT, but 18F-FDG PET/CT had higher sensitivity. Higher 18F-FDG uptake levels were detected in patients with ALN metastasis, histologic grade 3, estrogen–progesterone-negative receptor status, lymphatic invasion, and moderate to poor prognostic groups. There was no statistical difference for the retention index in categorical pathological parameters except for progesterone-negative status. In conclusion, 18F-FDG PET/CT scans may be a valuable imaging technique for evaluating primary tumor and axillary status in staging breast carcinoma and 18F-FDG uptake may be a prognostic factor that indicates aggressive tumor biology and poor prognosis. Dual-time imaging in breast carcinoma staging may not be used for predicting pathological criteria and the aggressiveness of primary lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast carcinoma is the most common cancer in women. Bilateral mammography (MMG), breast ultrasonography (USG), and breast magnetic resonance imaging (MRI) can be used to diagnose breast carcinoma according to the National Comprehensive Cancer Network guidelines [1]. In initial evaluations of primary breast carcinoma, MMG is still the most widely used modality and is commonly combined with USG to evaluate axillary nodal involvement. Breast MRI is a valuable supplement to MMG and USG to determine the local operative treatment strategy for a primary breast cancer lesion [2]. MRI has an additional benefit in that it does not involve exposing the patient to radioactivity. MRI is more sensitive and accurate than MMG and USG for detecting invasive lobular cancer [3].
Lately, 18F-fluorodeoxyglucose positron emission tomography and computed tomography (18F-FDG PET/CT) has been suggested for staging breast carcinoma by the National Comprehensive Cancer Network guidelines. This suggestion is especially relevant for cases of locally advanced or metastatic disease, conditions for which standard staging studies are equivocal, or suspicious findings [1]. Uptake of 18F-FDG, a commonly used radiopharmaceutical in PET/CT scans, increases distinctly in malignant cells after periods longer than 1 h [4]. Therefore, using delayed PET scans or dual-time 18F-FDG PET/CT imaging in oncological imaging has been suggested by some researchers. Determining the aggressiveness of the tumor before treatment is very important for patient management and surveillance. Some pathological parameters such as receptor status, histological tumor grade, lymphovascular/perineural invasion, and the Ki-67 index are helpful for determining disease prognosis. Determining locoregional spread with initial staging is important for the selection of neoadjuvant or adjuvant therapy and surgical procedures. The surgical staging of the axilla using either sentinel lymph node biopsy (SLNB) or axillary lymph node dissection (ALND) is the most accurate method [5]. However, determining ALN metastasis before surgery may avoid unnecessary SLNB, reducing patient discomfort.
In this study, we qualified the diagnostic ability of dual-time 18F-FDG PET/CT imaging in recently diagnosed breast carcinoma for detecting primary breast tumors and ALN status; we also compared the results with those of conventional imaging methods. This retrospective research was carried out to consider the relationship between the 18F-FDG uptake pattern and prognostic factors. We also examined the efficiency of dual-time imaging in detecting primary tumors.
Methods
Patients
This retrospective study included 78 female patients (mean age, 51.29 ± 12.20 years; age range, 24–78 years) with breast cancer who had received 18F-FDG PET/CT scans for preoperative staging between July 2010 and November 2013. One patient had bilateral invasive ductal carcinoma. Thus, 79 lesions were evaluated in 78 patients. In our institute, the 18F-FDG PET/CT scan is performed for tumors larger than 1.0 cm in diameter because of the frequency of false-negative PET results in tumors of diameter less than 1.0 cm [6]. Breast carcinoma was diagnosed by recent trocar needle biopsy in all patients before 18F-FDG PET/CT imaging. The exclusion criterion was reception of neoadjuvant therapy before undergoing imaging studies and surgery. The conventional imaging results were evaluated by breast MRI of 79 lesions in 78 patients, bilateral MMG of 40 lesions in 40 patients, and breast USG of 47 lesions in 46 patients. This study was approved by the local ethics committee (number: GOKAEK/2014-188).
18F-FDG PET/CT Imaging Protocol
The patients were required to fast for at least 6 h before scanning; blood glucose levels were checked before injection. The 18F-FDG dose was calculated as 2.5 MBq/kg body weight (±10 %) and administered intravenously in the contralateral antecubital region or hand. The patients were rested in a quiet room during the waiting period after injection. Whole-body 18F-FDG PET/CT imaging with a Gemini GXL PET/CT scanner (Philips Healthcare, Best, The Netherlands) was performed from the vertex to the mid thighs approximately 1 h after injection. First, a CT image was obtained from the integrated PET/CT scanner with the use of a standardized protocol using 120 kV, automatically calculated milliampere seconds for the patient’s weight, a tube rotation time of 0.75 s per rotation, and a section thickness of 3.3 mm. Immediately after the CT, PET images were acquired for 3 min per bed position and reconstructed using CT data for attenuation correction with iterative reconstruction. For dual-time PET/CT scans, late imaging was obtained approximately 60 to 90 min after the first scan for evaluation of temporal changes in 18F-FDG uptake. The late scan was acquired at 4 min per bed position in supine or prone position.
The 18F-FDG PET/CT images were interpreted by visual inspection in transaxial, coronal, and sagittal planes. The foci of increased uptake in the primary lesion and ALN metastasis, if detected, were noted. Furthermore, CT data were examined for the ALN status. The regions of interest were drawn over each hypermetabolic lesion, and the maximum standardized uptake value (SUVmax) was calculated automatically in all the patients from first (SUVmax1) and late (SUVmax2) images of both the primary lesion and the ALN metastasis. If there were multiple nodes with perceptible 18F-FDG uptake, the highest SUVmax was selected. The retention index (RI), or percentage change of SUVmax, was calculated as follows:
The RI was available for 67 patients, because late images were not available in all the patients and because of technical problems in some images.
Conventional Imaging Methods
Dynamic contrast-enhanced breast MRI was achieved on a 1.5-T MR scanner with multichannel capability (Philips Intera; Philips Healthcare) in 77 patients, and 78 primary lesions were evaluated. A standard four-channel phased-array breast coil was used. After obtaining a localizer sequence, an axial T2-weighted turbo spin-echo (TSE) sequence (6 min; repetition time/echo time (TR/TE), 10,000/87; flip angle, 180°; slice thickness, 4.5 mm, no gap; number of excitations (nex), 2; matrix, 256 × 224) was obtained. Subsequently, a dynamic axial T1 3D fast low-angle shot (FLASH) sequence (9 min; TR/TE, 700/8; flip angle, 15°; thickness, 2.0 mm, 0.4 mm gap; nex, 1; matrix, 3656 × 384) was achieved (Omniscan; Amersham Health, Cork, Ireland), followed by an IV injection of gadodiamide. After four subsequent dynamic series, image subtractions of the contrast-enhanced images from the pre-contrast images were carried out.
Bilateral MMG in craniocaudal and mediolateral oblique position by Senographe 700T (GE Medical System, Waukesha, WI, USA) was performed with 28–32 mA s and 25–30 kV. The breast USG was applied with a 7.5-MHz linear probe (EnVisor HD; Philips Healthcare).
Pathology
Histopathological results were used as the standard. Postoperative histopathology samples were analyzed according to the College of American Pathologists protocol. The modified Bloom–Richardson grading system, also called the Nottingham system, was used, combining nuclear grade, tubule formation, and mitotic rate. Each element is given a score of 1 to 3 (1 being the best and 3 the worst), and the scores of all three components are added together to give the grade. In addition, for invasive ductal carcinoma, but not other histologic types, the Nottingham prognostic index (NPI) was calculated with the following formula:
The patients were divided into three groups according to the cutoff points of the index into good (≤3.4), moderate (3.41–5.4), and poor (>5.4) prognostic groups.
For immunohistochemical analysis, estrogen (ER) and progesterone (PR) receptor expression statuses were scored as high (≥10 %), low (1–9 %), and negative (0 %) [7]. Her-2/neu was categorized with scores of 0, 1+, 2+, and 3+. The proliferation index Ki-67 was measured as a percentage. When the Ki-67 index was equal to or greater than 20 %, it was taken as positive.
Statistical Analysis
Statistical analysis was carried out using the NCSS Statistical Software version 2007 (Kaysville, UT, USA). The Kruskal–Wallis test was used to compare groups. The post hoc Dunn’s multiple comparison test was used to compare subgroups. The Mann–Whitney U test was used to compare prognostic groups that were classified as positive–negative or yes–no groups for SUVmax1, SUVmax2, and RI. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and likelihood ratio were calculated for MMG, USG, MRI, and 18F-FDG PET/CT results achieved from visual assessment. The results were evaluated within a 95 % confidence interval. The statistical significance level was established at p < 0.05.
Results
Breast carcinoma was histologically confirmed in all the patients. One patient had bilateral invasive ductal carcinoma with metastases in the left axilla; histologic grades were 3 in the left side and 2 in the right side. The characteristic features of patients are recorded in Table 1. Primary tumor detection was obtained in 76 of 79 lesions (96.2 %) by 18F-FDG PET/CT, in 74 of 78 lesions (94.8 %) by MRI, in 41 of 47 lesions (87.2 %) by USG, and in 24 of 40 lesions (60 %) by MMG. While MRI detected satellite lesions in 24 (30.8 %) patients, 18F-FDG PET/CT detected satellite lesions in only 17 (21.5 %) patients. Satellite lesions compatible with multifocality in the breast were confirmed in only seven (6.5 %) patients by pathological examination. The sensitivity, specificity, PPV, NPV, and accuracy of imaging modalities for detection of multifocality and ALN metastases are shown in Table 2. The presence of ALN metastases evidenced by 18F-FDG increased uptake was evaluated visually on the overlaid PET/CT and separated PET and CT. If there was a suspected metastasis seen in all image types, such as hypermetabolism, an increase of cortical thickening, or loss of the fatty hilus of the lymph node, the patient was noted as having ALN metastases.
The 18F-FDG uptake pattern of the primary lesion was compared with pathological findings (Table 3). ER and PR hormone receptor statuses were studied in 77 patients. The ER receptor status was found to be high in 62 (78.5 %) patients, low in one (1.3 %) patient, and negative in 15 (19 %) patients. The PR receptor status was detected as high in 53 (67.1 %) patients, low in two (2.5 %) patients, and negative in 23 (29.1 %) patients. When ER and PR receptor statuses were mixed between high and low, this was accepted as positive.
Discussion
Staging is important for breast cancer because the extent of the disease at presentation is a significant prognostic factor [8]. Carcinoma metastasis outside of the breast is typically divided into regional (lymph nodes, particularly the ALN) and systemic spread. ALN status assessment is important for making decisions on further treatment after surgery and to determine the aggressiveness of the disease. A single imaging modality that can provide sufficient information about these two parameters will prevent unnecessary work.
Detecting Primary Lesions
There are many studies about detecting primary breast carcinoma [9, 10]. The rate of primary tumor detection by 18F-FDG PET/CT was higher than that of MRI, USG, and MMG. Furthermore, 18F-FDG PET/CT was superior to MRI in the detection of multifocality with 57 % sensitivity, 81 % specificity, and equal accuracy. False-negative results in our study were found for 1.5-cm invasive lobular carcinoma, 1.2-cm invasive ductal carcinoma, and the combination of Paget and DCIS. Choi et al. [9] showed that 18F-FDG PET/CT was more effective than MRI and USG in detecting primary lesion tumors sized above 2.0 cm and that the USG was more successful in detecting lesions less than 2.0 cm in diameter. In contrast, we found good detection of primary lesions with 18F-FDG PET/CT in patients with tumors larger than 1.0 cm. The sensitivity of 18F-FDG PET/CT for detecting multiple lesions in the study performed by Choi et al. [9] was the lowest of the tested methods, whereas specificity was highest. Garami et al. [10] found similar results to our own in 115 breast cancer patients; in that study, the sensitivity of the traditional diagnostic modalities in the detection of multifocality was 43.8 %, while that of PET/CT was 100 % (p < 0.001).
Detecting ALN Metastases
One of the most essential prognostic factors in breast carcinoma is ALN status [11]. We found that 18F-FDG PET/CT, with its higher accuracy, also had the highest sensitivity, though MRI had the highest specificity. Seventeen patients had false-negative results for ALN status according to 18F-FDG PET/CT. Only one patient had micrometastasis. Twelve of 17 patients with false-negative ALN status had N1 lymph node status. We thought that the N1 status might have more false-negative results in determination of metastatic lymph nodes with PET/CT. In a retrospective study for ALN metastasis detection, Choi et al. [9] reported that the presence of micrometastases could not be determined by 18F-FDG PET/CT. Furthermore, the researchers concluded that 18F-FDG PET/CT returned comparable sensitivity to USG and MRI, but had relatively high specificity in detecting ALN metastases. Garami et al. [10] found that 18F-FDG PET/CT is successful at determining axillary lymphatic status, with more accuracy than USG. In a recent study, researchers compared the axillary USG, contrast-enhanced MRI, and 18F-FDG PET/CT to determine the most adequate test, or combination of tests, for detecting ALN metastasis in T1 breast cancer. They found that currently there are no definitive modalities that can replace SLNB for detecting ALN metastasis in T1 size tumors. They suggested that ALND might be a better option if ALN metastasis is suspected based on imaging [12]. Similarly, a study used 18F-FDG PET/CT as a triage tool to choose between SLNB and ALND. This triage has the potential to reduce the number of ALN dissections applied [13]. In a study performed by Reddy and Srivastava [14], PET/CT was compared with SLNB to evaluate axillary lymph node involvement in 37 patients with T1T2N0 breast carcinoma. The researchers found that the sensitivity of PET/CT was lower than that of SLNB but that it has high specificity and positive predictive value. They also noted that PET/CT is expensive and available at few centers. We believe that 18F-FDG PET/CT, if performed preoperatively for staging, could be a suitable tool for triage of SLNB and ALND because of its higher sensitivity, PPV, NPV, and accuracy compared with other available imaging methods.
SUVmax of the Primary Lesion
High 18F-FDG uptake levels have been associated with aggressive tumor biology for various malignancies in several studies. In a study performed by Inoue [15], a high-18F-FDG uptake was seen in patients in a poor prognosis group (5-year disease-free survival rates, 75.0 vs. 95.1 %). Furthermore, 18F-FDG uptake in the primary tumor has been found to be higher in patients with positive lymph node metastasis, similar to our findings [15–18]. In one study, the combination of high SUVmax and positive ALN metastasis was shown to be a highly significant risk factor, independent of the clinical T and N factors. That is, patients with high SUVmax and ALN metastasis in PET showed a significantly poorer prognosis than the other patients (5-year disease-free survival rates, 44.4 vs. 96.8 %). This suggests that 18F-FDG PET is useful in the preoperative evaluation of prognosis in breast cancer patients and that it can be used for chemotherapy decision-making [15]. Lymphatic and vascular invasion may be related to the ALN and distant metastasis risk [19]. A study reported that there was a relationship between lymphatic invasion and 18F-FDG uptake similar to our findings [16], whereas other studies found that there was no relationship [20]. A recent study reported no relationship between perineural/vascular invasion and 18F-FDG uptake, similar to our results [16].
The 18F-FDG uptake of the primary tumor in various publications has been found to be positively related to tumor size [16–18, 21], whereas other studies revealed that there was no relationship [15, 20]. In a study performed by Heudel et al. [21], the low SUVmax level in T1 tumors was thought to be related to a partial volume effect. Our study did not include T1a–T1b tumor sizes to avoid partial volume effects in our results. However, we found a lower SUVmax level in T1c-sized tumors than those sized T2 and T4. Grouheux et al. [20] excluded tumors smaller than 2.0 cm to avoid the partial volume effect and showed no correlation between tumor size and 18F-FDG uptake, similar to our findings.
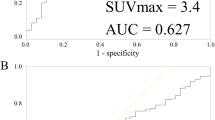
Some studies have reported a strong positive correlation between 18F-FDG uptake and histological grade [16–18, 20, 21], and our results are similar to these findings. The NPI score for invasive ductal carcinoma is based on assessment of tumor size, grade, and nodal stage and has yielded important prognostic information. One study compared NPI scores and the SUVmax [22]. In this study, in the worse prognosis group, the optimal threshold values were ≥4.2 for SUVmax. The predicted 15-year survival rates were 80, 42, and 13 % in the good, moderate, and poor prognostic groups, respectively [23]. Analogously, some researchers have established that breast carcinomas with a high SUVmax (>4.0) were associated with poorer prognosis, higher relapse, and higher mortality rates [15, 18]. In our study, we could not determine a threshold, but SUVmax1 and SUVmax2 levels were lower in the good prognostic group than in the moderate and poor prognostic groups.
Some studies have demonstrated a relationship between SUV and hormone receptors such as ER [16, 21] and PR [21]. We found lower SUVmax1 and SUVmax2 in ER- and PR-positive patients. Furthermore, c-erb-B2 overexpression is not associated with increased 18F-FDG uptake [17, 20]. The positive correlation between Ki-67 index and 18F-FDG uptake has been reported previously [16]. Controversially, we established that Ki-67 index was not correlated with SUVmax1, SUVmax2, or RI.
Boerner et al. [24] showed higher tumor-to-non-tumor and tumor-to-organ ratios in PET images made 3 h after 18F-FDG injection in breast cancer and enhancement of the lesion detectability when compared with images made 1.5 h after injection. Researchers determined that the RI showed the best results with a positive and significant relationship (p < 0.05) with ER and PR status and Ki-67 in breast carcinoma [25]. We determined that there was a significantly high RI level for dual time 18F-FDG PET/CT imaging for those with PR-negative status. But, there was no relationship between RI and other pathological parameters.
Limitations
This retrospective study has some limitations. These are the following: (1) each conventional imaging technique was not performed on all the patients, (2) the time between early and late imaging of dual time 18F-FDG PET/CT was not the same in each patient, (3) the Ki-67 index was not available for every patient, and (4) the area under the receiver operating characteristic curve for RI and SUVmax values was not calculated because of the limited number of patients and the distribution of data. Therefore, a cutoff point for these was not determined.
Conclusions
The 18F-FDG PET/CT scan may be a valuable imaging technique for detection of primary tumor and axillary staging. Positive ALN status by 18F-FDG PET/CT can be used as a triage tool to choose SLNB or ALND. Furthermore, 18F-FDG uptake may be a factor that indicates aggressive tumor biology and prognosis. Although dual-time 18F-FDG PET/CT imaging was only useful in determining PR status, we believe that dual-time imaging in breast carcinoma staging may not be used for predicting pathological criteria and the aggressiveness of primary lesions.
References
Bevers TB, Anderson BO, Bonaccio E, Buys S, Daly MB, Dempsey PJ, Farrar WB, Fleming I, Garber JE, Harris RE (2009) Breast cancer screening and diagnosis. J Natl Compr Cancer Netw 7:1060–1096
Abdulkareem ST (2014) Breast magnetic resonance imaging indications in current practice. Asian Pac J Cancer Prev 15:569–575
Biglia N, Mariani L, Sgro L, Mininanni P, Moggio G, Sismondi P (2007) Increased incidence of lobular breast cancer in women treated with hormone replacement therapy: implications for diagnosis, surgical and medical treatment. Endocr Relat Cancer 14:549–567. doi:10.1677/ERC-06-0060
Lodge MA, Lucas JD, Marsden PK, Cronin BF, O’Doherty MJ, Smith MA (1999) A PET study of 18FDG uptake in soft tissue masses. Eur J Nucl Med 26:22–30
Yi M, Giordano SH, Meric-Bernstam F, Mittendorf EA, Kuerer HM, Hwang RF, Bedrosian I, Rourke L, Hunt KK (2010) Trends in and outcomes from sentinel lymph node biopsy (SLNB) alone vs. SLNB with axillary lymph node dissection for node-positive breast cancer patients: experience from the SEER database. Ann Surg Oncol 17(Suppl 3):343–351. doi:10.1245/s10434-010-1253-3
Kumar R, Chauhan A, Zhuang H, Chandra P, Schnall M, Alavi A (2006) Clinicopathologic factors associated with false negative FDG-PET in primary breast cancer. Breast Cancer Res Treat 98:267–274. doi:10.1007/s10549-006-9159-2
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A et al (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28:2784–2795. doi:10.1200/JCO.2009.25.6529
Singletary SE, Connolly JL (2006) Breast cancer staging: working with the sixth edition of the AJCC Cancer Staging Manual. CA Cancer J Clin 56:37–47
Choi YJ, Shin YD, Kang YH, Lee MS, Lee MK, Cho BS, Kang YJ, Park JS (2012) The effects of preoperative (18)F-FDG PET/CT in breast cancer patients in comparison to the conventional imaging study. J Breast Cancer 15:441–448. doi:10.4048/jbc.2012.15.4.441
Garami Z, Hascsi Z, Varga J, Dinya T, Tanyi M, Garai I, Damjanovich L, Galuska L (2012) The value of 18-FDG PET/CT in early-stage breast cancer compared to traditional diagnostic modalities with an emphasis on changes in disease stage designation and treatment plan. Eur J Surg Oncol 38:31–37. doi:10.1016/j.ejso.2011.09.002
Dong G, Wang D, Liang X, Gao H, Wang L, Yu X, Liu J (2014) Factors related to survival rates for breast cancer patients. Int J Clin Exp Med 7:3719–3724
Hwang SO, Lee SW, Kim HJ, Kim WW, Park HY, Jung JH (2013) The comparative study of ultrasonography, contrast-enhanced MRI, and (18)F-FDG PET/CT for detecting axillary lymph node metastasis in T1 breast cancer. J Breast Cancer 16:315–321. doi:10.4048/jbc.2013.16.3.315
Heusner TA, Kuemmel S, Hahn S, Koeninger A, Otterbach F, Hamami ME, Kimmig KR, Forsting M, Bockisch A, Antoch G, Stahl A (2009) Diagnostic value of full-dose FDG PET/CT for axillary lymph node staging in breast cancer patients. Eur J Nucl Med Mol Imaging 36:1543–1550. doi:10.1007/s00259-009-1145-6
Reddy CV, Srivastava A (2009) Role of FDG PET-CT in evaluation of axillary lymph node involvement in T1T2N0 breast cancer in comparison with sentinel lymph node biopsy. J Nucl Med 50(Supplement 2):1691–1691
Inoue T, Yutani K, Taguchi T, Tamaki Y, Shiba E, Noguchi S (2004) Preoperative evaluation of prognosis in breast cancer patients by [(18)F]2-deoxy-2-fluoro-D-glucose-positron emission tomography. J Cancer Res Clin Oncol 130:273–278. doi:10.1007/s00432-003-0536-5
Ekmekcioglu O, Aliyev A, Yilmaz S, Arslan E, Kaya R, Kocael P, Erkan ME, Halac M, Sonmezoglu K (2013) Correlation of 18F-fluorodeoxyglucose uptake with histopathological prognostic factors in breast carcinoma. Nucl Med Commun 34:1055–1067. doi:10.1097/MNM.0b013e3283658369
Ikenaga N, Otomo N, Toyofuku A, Ueda Y, Toyoda K, Hayashi T, Nishikawa K, Tanaka M (2007) Standardized uptake values for breast carcinomas assessed by fluorodeoxyglucose-positron emission tomography correlate with prognostic factors. Am Surg 73:1151–1157
Ueda S, Tsuda H, Asakawa H, Shigekawa T, Fukatsu K, Kondo N, Yamamoto M, Hama Y, Tamura K, Ishida J, Abe Y, Mochizuki H (2008) Clinicopathological and prognostic relevance of uptake level using 18F-fluorodeoxyglucose positron emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in primary breast cancer. Jpn J Clin Oncol 38:250–258. doi:10.1093/jjco/hyn019
Woo CS, Silberman H, Nakamura SK, Ye W, Sposto R, Colburn W, Waisman JR, Silverstein MJ (2002) Lymph node status combined with lymphovascular invasion creates a more powerful tool for predicting outcome in patients with invasive breast cancer. Am J Surg 184:337–340
Groheux D, Giacchetti S, Moretti JL, Porcher R, Espié M, Lehmann-Che J, de Roquancourt A, Hamy AS, Cuvier C, Vercellino L, Hindié E (2011) Correlation of high 18F-FDG uptake to clinical, pathological and biological prognostic factors in breast cancer. Eur J Nucl Med Mol Imaging 38:426–435. doi:10.1007/s00259-010-1640-9
Heudel P, Cimarelli S, Montella A, Bouteille C, Mognetti T (2010) Value of PET-FDG in primary breast cancer based on histopathological and immunohistochemical prognostic factors. Int J Clin Oncol 15:588–593. doi:10.1007/s10147-010-0120-3
Nakajo M, Kajiya Y, Kaneko T, Kaneko Y, Takasaki T, Tani A, Ueno M, Koriyama C, Nakajo M (2010) FDG PET/CT and diffusion-weighted imaging for breast cancer: prognostic value of maximum standardized uptake values and apparent diffusion coefficient values of the primary lesion. Eur J Nucl Med Mol Imaging 37:2011–2020. doi:10.1007/s00259-010-1529-7
Elston CW, Ellis IO, Pinder SE (1999) Pathological prognostic factors in breast cancer. Crit Rev Oncol Hematol 31:209–223
Boerner AR, Weckesser M, Herzog H, Schmitz T, Audretsch W, Nitz U, Bender HG, Mueller-Gaertner HW (1999) Optimal scan time for fluorine-18 fluorodeoxyglucose positron emission tomography in breast cancer. Eur J Nucl Med 26:226–230
García Vicente AM, Soriano Castrejón A, Relea Calatayud F, Muñoz Madero V, Molina Garrido MJ, León Martín AA, Cordero García JM, Pilkington Woll JP, Chacón López-Muñiz I, Palomar Muñoz A (2012) 18F-FDG semi-quantitative parameters and biological prognostic factors in locally advanced breast cancer. Rev Esp Med Nucl Imagen Mol 31:308–314. doi:10.1016/j.remn.2011.12.001
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the local ethics committee (number: GOKAEK/2014-188).
Statements
The authors have no potential conflicts of interest to disclose. Although formal consent is not required for this type of study, our study was approved by the local ethics committee. This study does not contain any experiments with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ozen, A., Altinay, S., Ekmekcioglu, O. et al. Dual-Time 18F-FDG PET/CT Imaging in Initial Locoregional Staging of Breast Carcinoma: Comparison with Conventional Imaging and Pathological Prognostic Factors. Indian J Surg 78, 382–389 (2016). https://doi.org/10.1007/s12262-016-1486-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-016-1486-x