Abstract
Pancreatic ductal injury is rare during choledochal cyst excision. Most cases present in the immediate postoperative period with pancreatic fistula or acute pancreatitis are managed conservatively. But, inadvertent ligation of the main pancreatic duct with subsequent recurrent pancreatitis and upstream dilatation of the pancreatic duct requiring a pancreatic ductal drainage operation has not been reported in the English literature. A 23-year-old female patient presented with recurrent episodes of upper abdominal pain for about 16 months. She had a history of type-1 choledochal cyst excision 18 months back. She was evaluated with abdominal ultrasound and magnetic resonance cholangiopancreatography (MRCP). MRCP showed hugely dilated main pancreatic duct with normal hepaticojejunostomy anastomosis. There was no residual cyst. MRCP findings were suggestive of stricture of the main pancreatic duct due to previous surgery. Endoscopic pancreatic ductal decompression failed. The patient was treated successfully with pancreaticogastrostomy. Postoperative recovery was uneventful. The patient was well at 24-month follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Choledochal cyst is defined as a congenital dilatation of the intrahepatic or extrahepatic biliary tree. If left untreated, they can cause morbidity and mortality from recurrent cholangitis, pancreatitis, sepsis, liver abscess, and cholangiocarcinoma. Currently, the accepted treatment is complete cyst excision and hepaticoenterostomy. Early complications of cyst excision include anastomotic leak, bowel obstruction due to kinking or adhesions, acute pancreatitis, and pancreatic leak with injury to the pancreatic duct [1]. Most common late complication is biliary-enteric anastomotic stricture. Though there are adequate data regarding the postoperative biliary complications, very few studies [2, 3] had addressed pancreatic injury after choledochal cyst excision. Herein, we report a case of inadvertent ligation of the main pancreatic duct during dissection of the intrapancreatic portion of the choledochal cyst.
Case Report
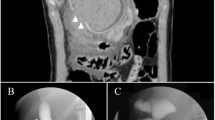
A 23-year-old female patient presented with recurrent episodes of upper abdominal pain for about 16 months. The frequency and intensity of pain had increased for the past 3 months, and she felt pain immediately after intake of food with occasional radiation to the left side of the back. She had undergone excision of type I choledochal cyst with Roux-en-Y hepaticojejunostomy 18 months back. Although the immediate postoperative recovery was uneventful, she began to feel postprandial abdominal pain 2 months after surgery. There was no history of jaundice, fever, and GI bleeding after operation. Physical examination was unremarkable. Laboratory investigations were within normal limits except raised serum amylase and lipase at the time of acute episodes of abdominal pain. She was evaluated with transabdominal ultrasound which showed a small cystic lesion in the head of the pancreas (likely to be a residual cyst in the retropancreatic region) with mildly dilated pancreatic duct. Magnetic resonance cholangiopancreatography (MRCP) (Fig. 1) showed hugely dilated pancreatic duct (3.5 cm in its maximal dimension) in the head and proximal body of the pancreas. There was no residual cyst. Previous hepaticojejunostomy site was normal and intrahepatic biliary radicles were not dilated. MRCP findings were suggestive of pancreatic duct stricture due to previous surgery. Endoscopic pancreatic ductal decompression failed. She had undergone pancreaticogastrostomy. Intraoperative findings were hugely dilated pancreatic duct throughout its length (more marked in the head region) and atrophied pancreatic parenchyma in the head and proximal body region. Pancreatic duct contained few concretions but no definite stone formation. Postoperative recovery was uneventful. The patient was well at 24-month follow-up.
Discussion
Management of choledochal cyst has evolved over decades. As this condition is more common in oriental countries, several advances in treatment have come from that quarter. Currently, the accepted treatment is complete excision. More emphasis in recent literature has been laid on the detail and the level of proximal anastomosis and the type of enteric drainage, the width of the anastomosis, the postoperative biliary complications, and the advisability of hepatic resection in type IVA cysts. But, there is paucity of data regarding the management of intrapancreatic portion of the cyst and the postoperative pancreatic complications. Complete excision of the intrapancreatic portion of the cyst is recommended for two reasons: (1) the residual cyst may contribute to stone formation [2, 4] and (2) carcinoma may arise from this residual cyst [5]. But, this is a tedious job with chances of injury to the pancreas. Reported early complications of the distal dissection are pancreatitis or pancreatic fistula from damage to the pancreatic duct. To avoid pancreatic injury, many authors recommended intramural dissection of the cyst [6], partial excision leaving behind the intrapancreatic portion of the cyst [7], and intraoperative cyst endoscopy [8] to identify the location of the pancreatic duct so that as much of the distal bile duct can be excised without pancreatic duct injury. Ando et al. [2] have recommended dissection external to epicholedochal plexus to prevent pancreatic injury. An important observation they have made is that the narrow distal segment connecting the cyst and the main pancreatic duct is located not at the bottom of the cyst but more proximally to the right ventral aspect of the cyst. They have reported no early complications by using this technique. But we think no method is completely immune as often scattered pancreatic tissue is splayed out over the inferior aspect of the cyst and is left in situ at the completion of the operation.
In conclusion, we can say that dissection just outside the epicholedochal plexus, meticulous hemostasis, gentle handling of pancreatic parenchyma, and proper delineation of the bile duct-pancreatic duct junction (as described by Ando et al.) are the key steps to reduce the incidence of pancreatic injury.
References
Singham J, Yoshida EM, Scudamore CH (2010) Choledochal cysts. Part 3 of 3: management. Can J Surg 53(1):51–56
Ando H, Kaneko K, Ito T, Watanabe Y, Seo T, Harada T et al (1996) Complete excision of the intrapancreatic portion of choledochal cysts. J Am Coll Surg 183(4):317–321
Li MJ, Feng JX, Jin QF (2002) Early complications after excision with hepaticoenterostomy for infants and children with choledochal cysts. Hepatobiliary Pancreat Dis Int 1(2):281–284
Hsu RK, Yu A, Lee JG, Leung JW (2001) Pancreatitis caused by common bile duct stones in a 3-year-old boy with prior surgery for a choledochal cyst. Am J Gastroenterol 96(6):1919–1921
Yoshikawa K, Yoshida K, Shirai Y, Sato N, Kashima Y, Coutinho DS et al (1986) A case of carcinoma arising in the intrapancreatic terminal choledochus 12 years after primary excision of a giant choledochal cyst. Am J Gastroenterol 81(5):378–384
Okada A, Nakamura T, Okumura K, Oguchi Y, Kamata S (1987) Surgical treatment of congenital dilatation of bile duct (choledochal cyst) with technical considerations. Surgery 101(2):238–243
Filler RM, Stringel G (1980) Treatment of choledochal cyst by excision. J Pediatr Surg 15(4):437–442
Miyano T, Yamataka A, Kato Y, Kohno S, Fujiwara T (1995) Choledochal cysts: special emphasis on the usefulness of intraoperative endoscopy. J Pediatr Surg 30(3):482–484
Conflict of Interest
We have no conflicts of interest regarding this manuscript and we do not have any financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ray, S., Khamrui, S. Inadvertent Ligation of the Main Pancreatic Duct: an Extremely Rare Complication of Choledochal Cyst Excision. Indian J Surg 77 (Suppl 1), 92–93 (2015). https://doi.org/10.1007/s12262-014-1168-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-014-1168-5