Abstract
Clear cell odontogenic carcinoma (CCOC) is a rare odontogenic tumor associated with aggressive clinical behavior, metastasis and low survival. To date, only 67 cases have been described in the English language literature, and an understanding of the behavior of CCOC has been based on limited case reports. The aim of the research was to further reveal the features of CCOC. We report 5 new cases of CCOC, with a mean age of 52.4 years. The clinical and histopathologic data of the disease obtained from earlier literature (95 cases) and the 5 new cases were analyzed. Data were extracted, including demographics, histopathologic findings, clinical presentation, primary treatment and outcomes. Immunohistochemical results revealed that the cancer is positive for AE1/AE3, EMA and CK19, negative for smooth muscle actin SMA, Vim and S-100. EWSR1 translocation was also observed in the new cases, which may help in the diagnosis of CCOC. Metastases of CCOC were rare, but the local recurrence rate of CCOC rose to 42%. The best treatment for patients with CCOC is wide local excision combined with regional lymph node dissection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clear cell odontogenic carcinoma (CCOC) is a rare odontogenic tumor that was classified as a benign neoplasm. However, WHO has reclassified it as malignant tumor because of its aggressive clinical behavior, including an invasive growth pattern, local lymph node and distant metastasis and common recurrence [1, 2]. In 1985, Hansen et al. first described 3 cases of clear cell odontogenic tumor (CCOT) with local invasive ability and remarkably clear cell components [3]. After more than 30 years, it has again been reported, but little is known about CCOC because of the small sample size. Controversies remain regarding the epidemiology, histologic features, tumor cell differentiation, predictive factors of recurrence and outcomes of CCOC. Therefore, additional cases, especially recurrent cases, could help in the better understanding of the tumor biology of CCOC. Hence, this report includes 5 additional cases, including 3 cases with multiple recurrence. We analyzed the histopathological and immunohistochemical features in all 5 cases to examine the predictors of recurrence. Meanwhile, a comprehensive review was performed of the previously reported patients with CCOC, focusing mainly on clinical and histopathologic analysis of the reported patients along with the additional 5 patients from our data.
Materials and Methods
Case Series
The database of the department of oral pathology, Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, was searched systematically for the information of all patients with clear cell odontogenic carcinoma (CCOC) between 2002 and 2011. Patient charts who met these criteria were reviewed for pathological diagnosis. Available pathological slides were obtained and reviewed to confirm the diagnosis of CCOC.
Immunohistochemistry
Immunohistochemistry was performed on unstained sections using selected antibodies (Table 2). Briefly, 5 μm-thick sections were cut and mounted on adherent glass slides, dewaxed in xylene and rehydrated in graded ethanol. Endogenous peroxidase activity was blocked by immersion in 0.3% aqueous peroxide for 15 min, followed by 2 washes in 1 phosphate-buffered saline (PBS) for 5 min each. The slides were treated with 0.6 M sodium citrate buffer and heated in a microwave to 100 °C. Endogenous proteins were blocked by incubation in a 2% solution of bovine serum albumin in PBS for 20 min. Then, the sections were incubated for 1 h at room temperature, with the primary antibody diluted in PBS. This was followed by 2 washes in PBS and incubation with a hapten/peroxidase secondary antibody complex (Envision Plus; Dako Corp., Carpinteria, Calif) for 30 min. The bound complexes were observed by the application of either aminoethylcarbazole or diaminobenzadine (Sigma Chemical Company, St. Louis, Mo) containing 0.3 hydrogen peroxide as a substrate. After incubation, the sections were washed and lightly counterstained with hematoxylin, and a cover slip was placed. Negative controls consisted of omitting the primary antibody in the selected sections.
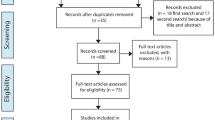
Literature Review
We conducted a comprehensive computer search of the English language literature in the National Institutes of Health PubMed database using combinations of the terms “clear cell odontogenic carcinoma,” “clear cell carcinoma” and “clear cell” to search for studies published between 1981 and December 2016. After a careful review of each published case, tumors were selected for inclusion if diagnosed as CCOC and/or showed the morphological, clinical, histochemical and immunohistochemical features typical of CCOC. Then, the data of demographics, clinical presentation, management and outcomes were extracted.
Statistical Analysis
Data from patients in our database and those in the literature review were abstracted and combined. Statistical analysis was performed with the SPSS 17.0 software package. The Pearson chi-square test was performed to assess the evaluation of factors that affect the risk of overall recurrence (α = 0.05).
Results
Clinical Features of our Files
From the review of our database, 5 patients with a CCOC diagnosis were identified. Clinical findings are summarized in Table 1. The mean age at the time of diagnosis was 58 years (range, 40–78 years) (3 women and 2 men). All patients were in an advanced stage, with a mean tumor size of 5.6 cm (range 4.5–8 cm). The main clinical symptoms included unhealed wounds after extraction, pain, loosened teeth and labial expansion of the alveolar bone. Tumor locations were mandible (4 tumors) and maxilla (1 tumor). Radiographically, all the patients presented with extensive bone resorption with well-defined to irregular margins. One patient had clinical submandibular lymph node metastasis on presentation. None had evidence of distant metastasis.
The Outcome of our Files
All patients were treated with wide excision. One patient underwent neck dissection at the time of resection, because of preoperative lymphadenopathy. Furthermore, histological evidence exhibited metastasis. Three patients had multiple recurrences, two patients had a first recurrence during enucleation five years and one year later respectively, while another patient had a first recurrence during block resection one year later. One patient who had positive lymph nodes and large bulky primary disease underwent adjuvant radiation therapy. No patients underwent chemotherapy. Follow-up ranged between 3 and 8 years. No distant metastases have been identified, and no deaths have occurred from the disease so far.
Histological and Immunohistochemical Features of our Files
Microscopically, all cases demonstrated similar patterns of lobules, trabeculae, and sheets of neoplastic cells (Fig. 1a). All cases demonstrated a background composed of a connective fibrous stroma that separated the tumor cells. The shape of the tumor cell was oval or polyhedral with small, eccentric, and dark-staining nuclei. In one tumor, rare mitosis and focal necrosis were observed (Fig. 2). Perineural invasion (PNI, Fig. 1b) was also identified in the same patient, who had multiple recurrences.
The immunohistochemical results of the 5 tumors are summarized in Table 2. Tumor cells were positive for AE1/AE3 (5/5) (Fig. 3), epithelial membrane antigen (EMA) (5/5), CK19 (5/5) and CK8 (1/5). Tumor cells were negative for smooth muscle actin (SMA) (0/5), Vim (0/5) and S-100 (0/5). Four cases showed EWSR1 translocation (Fig. 4).
Literature Review of CCOC
All 95 cases of CCOC reviewed were well documented. Epidemiology, treatment and outcomes of this sample population are summarized in Table 3, including the 5 new cases reported in our study (N = 100 cases). The average age of the patients was 52 years, and 61% of the reported CCOC occurred in women. The most common primary location was the posterior mandible (74%), followed by the maxilla (26%), and most of the patients were diagnosed in at an advanced stage. The most common symptom was swelling, and other signs included pain and tooth mobility. Overall, the preoperative lymph node status of 89 patients was available, and only 17 (17/89) had clinical lymphadenopathy on presentation. Ten patients presented with distant metastases.
The most common management of CCOC involved gross total resection. Overall, 85 patients underwent original treatment, and of these, 81 underwent gross total resection. Although, the curative effect of radiotherapy and chemotherapy was not clear, 22 patients were treated with radiotherapy as an adjuvant therapy, and 5 patients received chemotherapy.
The postoperative outcomes of 77 patients were documented. Of these, 57 were alive and disease-free, 10 were alive with disease and 10 had died from the disease. Metastases were rare, but the local recurrence rate of CCOC was 42% (35/83).
Discussion
Odontogenic tumors are rare tumors of the jaws that are predominantly composed of clear cell components. The initial report of aggressive and malignant clear cell odontogenic tumors was put forwarded by Hansen et al. [3], and few cases have been documented since. The most recent review of the English literature reported a total of 95 cases of CCOC [4,5,6]. The clinicopathologic features of this entity were first analyzed by Muramatsu et al. [7] The incidence of these tumors peaked in the fifth to seventh decades (mean age, 56.5 years; range, 17–89 years), with a female preponderance (M/F ratio, 10:17) and a prevalent localization in the anterior segments of the jaws. The mandible is affected more commonly than the maxilla.
Most patients complained of a painless swelling, tooth abnormalities or slow-growing progressive swelling over several months to years [8]. Radiologically, these tumors manifested as radiolucent lesions with irregular margins, with root resorption in most cases [9]. The differential diagnosis from the radiographic image includes squamous cell carcinoma, minor salivary gland carcinomas and metastatic tumors to the jaws. The clinical features of the present series were consistent with those of the previous reports. However, our data showed patients at a relatively younger age (mean 42.4 years) at diagnosis and a more apparent predilection for females (4:1). The most common location of the tumor was the anterior or premolar areas of the jaws (4 of 5 cases), and only one case was located in the mandibular molar and ramus regions, which are the typical sites for ameloblastomas.
The main histological differential diagnosis of CCOC includes other head and neck tumors with a conspicuous clear cell component. These may originate from sources including ameloblastoma, calcifying epithelial odontogenic tumors, squamous cell carcinoma and salivary gland tumors such as mucoepidermoid carcinoma, myoepithelial carcinoma and hyalinizing clear cell carcinoma.
Histopathologically, CCOCs show 3 patterns: biphasic, monophasic and ameloblastomatous. The most common pattern is biphasic, which comprises nests of cells with clear cytoplasm admixed with cells containing eosinophilic cytoplasm [10]. The 5 new cases reported were of typical biphasic pattern. The histologic features of CCOC are unique, and the presence of clear cells has been pathognomonic. Clear cell odontogenic carcinomas often demonstrate peripheral palisading nuclei, monotonous nuclear size with occasional raisinoid nuclei, stromal hyalinization and perineural invasion. Atypical mitoses were absent, and necrosis, neuronal and vascular invasions appear rare [11, 12]. In our cases, rare mitoses and focal necrosis were observed in the patient with multiple recurrences. Perineural invasion (PNI, Fig. 1b) was also identified in the same patient. The argument that the more aggressive examples of CCOC are often associated with transformation to high grade histology (areas of focal necrosis) was accepted. A similar phenomenon was also observed in Hyalinizing Clear Cell Carcinoma of the salivary gland (HCCC, data not shown). The relationship between focal necrosis and recurrence needs further confirmation, as, currently, its mechanism is not clear and the sample size is too small to draw conclusions.
Immunohistochemical and molecular analyses help to identify the tumors. CK14, CK19 and EMA immunostaining patterns and cellular distribution may help in the definitive diagnosis of CCOC, and the negativity of CK7, vimentin and SMA remained important in the exclusion of other tumors presenting clear cells [13, 14]. Our cases also demonstrated the immunohistochemical expression of cytokeratins (AE1/AE3and CK19) and EMA. Several reports demonstrated that EWSR1 translocation status remained helpful in the diagnosis of CCOC [15, 16]. Four of the 5 cases showed EWSR1 translocation. Most of the cases from our literature review were treated before EWSR1 testing and may not be CCOC but other entities such as clear cell mucoepidermoid carcinomas. EWSR1-rearrangement may occur in other subtypes of soft tissue tumors, such as mucoepidermoid carcinomas and sarcomas. Therefore, combined immunohistochemistry and EWSR1 rearrangement can improve the diagnostic precision for CCOC.
Surgical excision is the mainstay of treatment for CCOC. Examination of regional lymph nodes and radiological examination to exclude distant metastasis are recommended. Wide local excision and extensive lymph node dissection remains useful if lymph node involvement is suspected. Proper jaw reconstruction is important and should be performed simultaneously with resection. Fibular free flap is the best choice for the reconstruction of jaw defects in the mandible because of its advantages of adequate bone length, ease of graft dissection and contouring and long pedicles with proper vessels. The patients who underwent conservative therapy, such as enucleation or curettage, had higher local recurrence than those who underwent initial treatment by resection [17]. Therefore, surgical resection with negative bony margins remains the recommended treatment for CCOC because curettage or enucleation virtually guarantees local and/or regional recurrence. Although the curative effect of radiotherapy and chemotherapy is not clear, adjuvant radiotherapy could be considered for patients with soft tissue infiltrations and positive lymph nodes, especially if tumor-free margins are unclear.
References
Piattelli A, Sesenna E, Trisi P et al (1994) Clear cell odontogenic carcinoma: report of a case with lymph node and pulmonary metastases. Eur J Cancer B Oral Oncol 30 B:278–280
Brinck U, Gunawan B, Schulten HJ et al (2001) Clear cell odontogenic carcinoma with pulmonary metastases resembling pulmonary meningothelial-like nodules. Virchows Arch 438:412–417
Hansen LS, Eversole LR, Green TL et al (1985) Clear cell odontogenic tumour: a new histologic variant with aggressive potential. Head Neck Surg 8:115–123
Hadj Saïd M, Ordioni U, Benat G et al. (2017) Clear cell odontogenic carcinoma. A review. J Stomatol Oral Maxillofac Surg
Ordioni U, Benat G, Hadj Saïd M, et al. (2017) Clear cell odontogenic carcinoma, diagnostic difficulties. A case report. J Stomatol Oral Maxillofac Surg
Datar UV, Kamat MS, Kanitkar SS et al (2017) Clear cell odontogenic carcinoma: a rare case report with emphasis on differential diagnosis. J Cancer Res Ther 13(2):374–377
Muramatsu T, Hashimoto S (1996) Inoue Tet al. Clear cell odontogenic carcinoma in the mandible:histochemical and immunohistochemical observations with a review of the literature. J Oral Pathol Med 25(9):516–521
Swain N, Dhariwal R, Ray JG et al (2013) Clear cell odontogenic carcinoma of maxilla: a case report and mini review. J Oral Maxillofac Pathol 17:89–94
Chaine A, Pitak-Arnnop P, Dhanuthai K et al (2009) An asymptomatic radiolucent lesion of the maxilla. Clear cellodontogenic carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:452–457
Prakash AR, Sairam V, Srinivas Reddy P et al (2015) Clear cell odontogenic carcinoma-a rare case report. J Maxillofac Oral Surg 14(Suppl 1):60–63
Martínez Martínez M, Mosqueda-Taylor A, Carlos R et al (2014) Malignant odontogenic tumors: amulticentric Latin American study of 25 cases. Oral Dis 20:380–385
Loyola AM, Cardoso SV, de Faria PR et al (2015) Clear cell odontogenic carcinoma: report of 7 new cases and systematic review of the current knowledge. Oral Surg Oral Med Oral Pathol Oral Radiol 120(4):483–496
Chera BS, Villaret DB, Orlando CA et al (2008) Clear cell odontogenic carcinoma of the maxilla: a case report and literature review. Am J Otolaryngol 29(4):284–290
Carinci F, Volinia S, Rubini C et al (2003) Genetic profile of clear cell odontogenic carcinoma. J Craniofac Surg 14:356–362
Bilodeau EA, Weinreb I, Antonescu CR et al (2013) Clear cell odontogenic carcinomas show EWSR1 rearrangements: a novel finding and a biological link to salivary clear cell carcinomas. Am J Surg Pathol 37(7):1001–1005
Ginat DT, Villaflor V, Cipriani NA et al (2016) Oral cavity clear cell odontogenic carcinoma. Head Neck Pathol 10(2):217–220
Zhang J, Liu L, Pan J et al (2011) Clear cell odontogenic carcinoma: report of 6 cases and review of the literature. Med Oncol 28(Suppl 1):S626–S633
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiment: XHY LL BG. Performed the experiments: JWZ NSZ. Analyzed the data: XHY LL. Materials/Analysis tools: XHY. Wrote the paper XHY LL JWZ.
Corresponding authors
Ethics declarations
Competing Interests
All authors declare that there are no potential conflicts of interest.
Grant Support
This study was supported by Jiangsu Province’s Key Provincial Youth Talents Program (Grant No.QNRC2016841).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, L., Zhang, JW., Zhu, NS. et al. Clear Cell Odontogenic Carcinoma: a Clinicopathological and Immunocytochemical Analysis. Pathol. Oncol. Res. 26, 1559–1564 (2020). https://doi.org/10.1007/s12253-019-00741-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-019-00741-x