Abstract
The main objective of this study was to investigate the incidence of free tumour cells in peritoneal lavage cytology performed using a standard method before and after the resection of the tumour, and to assess the usefulness of this technique in scheduled interventions on colorectal cancer patients. Peritoneal lavage cytology was performed on a homogeneous sample of 188 patients undergoing colorectal cancer curative resection before and after the resection of the tumour. The procedure was performed systematically in all cases. Malignant cells were detected in the peritoneal lavage cytology performed before the resection of the tumour in three patients. Lymph node affection was the variable most associated with the prognosis of these colorectal cancer patients. Peritoneal lavage cytology can provide additional information for a small group of patients who need to be closely monitored and studied to decide on the most effective type of chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nowadays, in spite of the advances in treatment of colorectal cancer, many patients presenting an early stage develop recurrence, so that not enough is known about the variables that intervene in the evolution and prognosis of this disease. The identification of patients at risk of developing peritoneal metastases may thus improve prognostic information and guide targeted therapy.
The prognostic value of peritoneal lavage cytology is well established in ovarian neoplasia [1, 2] and gastric, pancreatic, and œsophageal tumours [2,3,4,5], but not in colorectal cancer.
The main objective of the present study was to investigate the incidence of free tumour cells in the peritoneal lavage cytology performed with a standard technique before and after tumour resection, and to assess the usefulness of this technique in patients who had had scheduled interventions for colorectal cancer. Among the secondary objectives was the study of prognostic variables of cancer-specific mortality and recurrence.
Methods
Patients
During the period from February 2013 to August 2016, a peritoneal cytology lavage (PCL) was performed before and after tumour resection on all the patients undergoing curative resection for colorectal cancer in our hospital. We have excluded patients with pre-operatively and intra-operatively diagnosed metastases, those undergoing emergency surgery, and those with a history of previous intra-abdominal tumour. In all cases, the tumour with free macroscopic and microscopic margins was completely resected (R0).
Recurrence that was locoregional, peritoneal, or in any other organs was defined by radiological or histological evidence of cancer recurrence in the region of the primary tumour bed, the abdominal cavity, or in other organs.
Procedures
Immediately after laparotomy (open surgery) or creation of the pneumoperitoneum and insertion of ports (laparoscopic surgery), but before exploration of the abdomen and mobilization of the tumour, 100 ml of saline solution was instilled in the area adjacent to the tumour, followed by immediate aspiration of 40 ml of this lavage fluid. In the case of extraperitoneal tumours, the saline solution was instilled into and aspirated from the Douglas’ pouch. The same procedure was carried out following tumour resection at the site where the tumour had been or in the Douglas’ pouch. The aspirates were passed into 50 ml centrifuge tubes containing 10 ml of “ThinPrep CytoLyt Solution” preservation liquid for processing 24 h later, beginning with centrifuging at 2500 rpm for 5 min. Two samples were prepared for each patient (before and after resection), processing them in ThinPrep 2000 and staining with hæmatoxylin and eosin (H&E). The sample was considered positive if at least one tumour cell was detected. Cells suspected of malignancy were classified as negative. The peritoneal lavage smears were checked by two pathologists, who would have to agree on the results.
Statistical Analyses
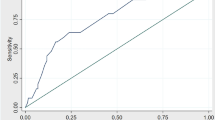
The results were analysed with the SPSS (version 18) program. Relationships between clinicopathologic parameters were assessed using the Chi-squared or the Fisher exact tests for qualitative variables and the Student’s t or Mann-Whitney U tests for quantitative variables. Kaplan-Meier disease-free survival (DFS) and net cancer-specific survival (NCSS) curves were calculated and compared using the log-rank test. For the cancer-specific survival calculation, data on patients who had died from other causes or who were still alive at the end of the study were censored. A Cox proportional hazards model was used to assess the cancer-specific mortality and recurrence risks (expressed in terms of the hazard ratio, HR). A p value of less than 0.05 was considered statistically significant.
Results
The study sample consisted of 188 patients (114 men and 74 women), mean age 69 years (range 34–89 years), and 127 (67.6%) with some cardiovascular risk factor (Table 1). The cases included 40 infraperitoneal rectal tumours. Of the 188 patients studied, 52 received neoadjuvant therapy as they presented a locally advanced rectal tumour. The tumour locations and surgical procedures are listed in Tables 2.
Malignant cells were found in the aspirates of 3 patients (2 open surgery, 1 laparoscopic), with only the pre-resection specimen being positive (1.6%). The median patient follow-up was 22 (0–49) months. Post-operative mortality (30 days after the intervention) was 2.7% (5 patients), and 9 patients died during the follow-up due to causes unrelated to the tumour.
The clinicopathologic characteristics of the 3 IPLC-positive patients are summarized in Table 3. In all three cases, there was deep invasion of the intestinal wall and affection of the lymph nodes. During the follow-up period, none of the three developed locoregional recurrence, peritoneal carcinomatosis, or distant metastases. However, in the 185 patients with negative cytology, the recurrence rate was 20.2% (n = 38), the cancer-specific mortality rate was 7.4% (n = 14), and 3 (1.6%) developed peritoneal recurrence (one stage pT3pN1b and two stage pT2pN0).
The 4-year NCSS was 86% and the 4-year DFS was 73%.
We performed univariate and multivariate analyses of the clinicopathologic variables (including the peritoneal lavage cytology) which could potentially influence the prognosis (Table 4). In the univariate analysis, the depth of tumour invasion at the level of the colon wall, the affection of regional lymph nodes, and lymphatic and venous invasion were significantly associated with DFS. Affection of lymph nodes was the only variable significantly related with NCSS. In the multivariate analysis, only affection of lymph nodes was an independent risk factor for DFS.
Discussion
With our standard technique, we only found tumour cells in 3 of the 188 patients (1.6%). This prevents us from analysing the prognostic value of this technique for the diagnosis of free tumour cells in the peritoneal cavity.
Recent studies suggest that the existence of free tumour cells in the peritoneal lavage fluid is associated with lower overall survival and greater likelihood of peritoneal recurrence [6,7,8], with positive peritoneal lavage rates of between 2.1% and 52% in patients with colorectal cancer [9]. This broad range reflects the heterogeneity of the lavage techniques and the laboratory methods used to detect free tumour cells in the peritoneal cavity. The laboratory methods used include conventional cytology, immunological techniques and molecular techniques. The advantage of cytology alone is that it is relatively inexpensive and does not require preservation of RNA and complex techniques. Mean weighted yield was calculated as 8·4% for cytopathology, 28·3% for immunological techiniques and 14·5% for molecular techniques [7].
The low rate of positive samples in our study may be due to our having only included stage I-III patients undergoing scheduled curative surgery, and also to our strict criterion for the identification of tumour cells which excluded cells only suspected to be malignant. Noura et al. [10] studied a sample of 697 patients using inclusion criteria and a malignant cell detection technique similar to ours, finding positive peritoneal lavage in 2.2% of the cases, a figure very similar to ours.
PC may be the result of the complex molecular interaction between cancer cells and receptor elements that is known as the peritoneal metastatic cascade [11]. We believe that the probability of detecting tumour cells during peritoneal transport is low. Although peritoneal lavage cytology is the best technique to find them, it is an insensitive procedure, only useful for a very small set of patients. Another carcinomatosis mechanism that has been described is the iatrogenic seeding of tumour cells during surgery. To study this theory, we decided to perform the peritoneal lavage at two times, but we found no tumour cells in any of the 188 samples taken after the tumour’s resection. Of all the papers published on free tumour cells in the peritoneal cavity, only three assessed the difference between pre- and post-resection lavage [9, 12, 13].
The limitations of this present study are due to its observational nature, and that it was performed in a single hospital, with a limited number of patients, and with a short follow-up period. On the contrary however, the patients studied constituted a group with very homogeneous characteristics, and the study was very rigorous and specific.
That we only found tumour cells in three patients is a major limitation for it to be possible to assess the prognostic value of peritoneal lavage cytology. We did observe, however, that these three patients presented stage pT3 and lymph node affection. Affection of regional lymph nodes was the variable that was most closely associated with NCSS and DFS in our study. During the follow-up period, none of these three patients developed any recurrence. Our overall peritoneal recurrence rate was 1.6%, which is lower than that described in the literature [14]. The incidence of peritoneal recurrence in patients with positive cytology is around 33.3% [26]. Currently we are continuing to monitor the evolution of these patients, and particularly closely that of the three with positive peritoneal lavage.
In the future, we can consider applying this technique as “special liquid biopsy” in early stage colon cancers. Now, we continue to perform the peritoneal lavage technique that we have described because it is simple and fast, and indeed we believe that it should be carried out systematically in all patients undergoing curative colorectal cancer resection. It can provide additional information for a group of patients which, while small, require meticulous monitoring and for whom clinical trials are needed to determine which type of chemotherapy is more effective – adjuvant or intraperitoneal.
We would also conclude that while peritoneal lavage cytology for the diagnosis of free tumour cells in patients undergoing curative colorectal cancer resection is an inexpensive method with high specificity, it is of low sensitivity. It is therefore not a useful, prognostically valuable, technique to apply to a large group of colorectal cancer patients. A multicentre study using a standard cytology technique would be needed to demonstrate the true usefulness of this procedure.
References
Ziselman EM, Harkavy SE, Hogan M, West W, Atkinson B (1984) Peritoneal washing cytology. Uses and diagnostic criteria in gynecologic neoplasms. Acta Cytol 28:105–110
Lowe E, McKenna H (1989) Peritoneal washing cytology: a retrospective analysis of 175 gynaecological patients. Aust N Z J Obstet Gynaecol 29:55–61
Miyashiro I, Takachi K, Doki Y, Ishikawa O, Ohigashi H, Murata K, Sasaki Y, Imaoka S, Nakaizumi A, Takenaka A, Furukawa H, Hiratsuka M (2005) When is curative gastrectomy justified for gastric cancer with positive peritoneal lavage cytology but negative macroscopic peritoneal implant? World J Surg 29:1131–1134
Ishikawa O, Wada H, Ohigashi H, Doki Y, Yokoyama S, Noura S, Yamada T, Sasaki Y, Imaoka S, Kasugai T, Matsunaga T, Takenaka A, Nakaizumi A (2003) Postoperative cytology for drained fluid from the pancreatic bed after “curative” resection of pancreatic cancers: does it predict both the patient’s prognosis and the site of cancer recurrence? Ann Surg 238:103–110
Doki Y, Kabuto T, Ishikawa O, Ohigashi H, Sasaki Y, Yamada T et al (2001) Does pleural lavage cytology before thoracic closure predict both patient’s prognosis and site of cancer recurrence after resection of esophageal cancer? Surgery 130:792–797
Mohan HM, O'Connor DB, O'Riordan JM, Winter DC (2013) Prognostic significance of detection of microscopic peritoneal disease in colorectal cancer: a systematic review. Surg Oncol 22:e1–e6
Bosanquet DC, Harris DA, Beynon J (2013) Systematic review and meta-analysis of intraoperative peritoneal lavage for colorectal cancer staging. Br J Surg 100:853–862
Nishikawa T, Sunami E, Tanaka T, Tanaka J, Kiyomatsu T, Kawai K (2015 Sep) el al. Incidence and prognostic significance of positive peritoneal lavage in colorectal cancer. Surg Today 45(9):1073–1081
Altomare DF, Tedeschi M, Rotelli MT, Bocale D, Piscitelli D, Rinaldi M (2011) Lack of prognostic role of pre- and postoperative peritoneal cytology and cytokeratin PCR-expression on local recurrence after curative anterior resection for mid-low rectal cancer. Updat Surg 63:109–113
Noura S, Ohue M, Seki Y, Yano M, Ishikawa O, Kameyama M (2009) Long-term prognostic value of conventional peritoneal lavage cytology in patients undergoing curative colorectal cancer resection. Dis Colon Rectum 52:1312–1320
Lemoine L, Sugarbaker P, Van der Speeten K (2016) Pathophysiology of colorectal peritoneal carcinomatosis: role of the peritoneum. World J Gastroenterol 22(34):7692–7707
Temesi R, Sikorszki L, Bezsilla J, Botos A, Kovacs J, Tihanyi T (2012) Impact of positive intraabdominal lavage cytology on the long-term prognosis of colorectal cancer patients. World J Surg 36:2714e21
Lloyd JM, McIver CM, Stephenson SA, Hewett PJ, Rieger N, Hardingham JE (2006) Identification of early-stage colorectal cancer patients at risk of relapse post-resection by immunobead reverse transcription-PCR analysis of peritoneal lavage fluid for malignant cells. Clin Cancer Res 12:417–423
Koppe MJ, Boerman OC, Oyen WJ, Bleichrodt RP (2006) Peritoneal carcinomatosis of colorectal origin: incidence and current treatment strategies. Ann Surg 243:212–222
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All the authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salamanca, I.M.G., Jaime, M.T.E., Penco, J.M.M. et al. Role of Peritoneal Cytology in Patients with Early Stage Colorectal Cancer. Pathol. Oncol. Res. 26, 1325–1329 (2020). https://doi.org/10.1007/s12253-019-00706-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-019-00706-0