Abstract
To explore the interaction effects of ciprofloxacin and ampicillin with nickel on the growth of bacteria, Staphylococcus aureus strain ATCC 29213, Enterococcus faecalis ATCC 29212 and Escherichia coli ATCC 25922 were used. Minimum inhibitory concentrations (MICs) were determined for nickel, ciprofloxacin and ampicillin, and the checkerboard method was used to assess their cumulative effects on bacterial growth. The interactions between the metal and antibiotics were assessed by the fractional inhibitory concentration (FIC). The MICs for ciprofloxacin and ampicillin were 0.31 and 1 mg/L for E. faecalis, 0.62 and 1 mg/L for S. aureus and 0.005 and 2.5 for E. coli, respectively. The MIC for nickel was 1000 mg/L for all bacteria. The FIC results for ciprofloxacin and nickel demonstrated an antagonistic effect of the two agents on the growth of E. coli and E. faecalis and an additive effect on S. aureus. The FICs for ampicillin and nickel demonstrated a synergistic effect on the growth of E. faecalis and E. coli. Different interactions of metals and antibiotics were observed depending on the bacteria and the type of antibiotic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heavy metals are micronutrients, although at higher concentrations, they can have a toxic effect on living beings. Their importance is emphasised because of their nonbiodegradability and accumulation in organisms (Atieh et al. 2017). Nickel (Ni) is a silvery-white heavy metal found in the Earth’s core and present in living organisms, mostly in plants. It is of interest in medicine because it is the most common contact allergen in the world (Thyssen et al. 2007). Human nickel intake is mostly in food, with some foods such as chocolate, oatmeal and nuts being especially nickel rich, which can increase nickel intake to 900 µg/day (Flyvholm et al. 1984). Furthermore, it can be released into the human body by the oral corrosion of nickel-containing dental alloys used for dental instruments, restorations and orthodontic appliances (Wendl et al. 2017). There is some concerning evidence of elevated nickel levels in the tissues of patients who have had an orthodontic appliance for 1 year (Jamshidi et al. 2018).
Human organisms contain more prokaryotic bacterial cells than eukaryotic cells, referred to as human commensal bacteria or the human microbiota. The role of the microbiota is increasingly recognised as vital for health and homeostasis, with some terming it a human organ (Wang et al. 2007; O’Hara and Shanahan 2006). It is of major importance for modelling metabolic phenotypes, immune system function, nutrient absorption and protection against pathogens (Wang and Li 2015; Ley et al. 2006).
Commensals can exist in silent mode, but when introduced to a susceptible body location or to an immunocompromised, injured or diseased individual, they can cause serious morbidity. Their silent and asymptomatic introduction to the community presents an epidemiologic challenge (Nicolas-Chanoine et al. 2008). Some bacteria that demonstrate such behaviour are Staphylococcus aureus, Escherichia coli and Enterococcus faecalis (Price et al. 2017). Heavy metals have also demonstrated the ability to alter the nature of bacteria (Dickinson et al. 2019). S. aureus is a gram-positive facultative anaerobe present as a commensal on human skin and, in 30% of the population, on the nasal mucosa (Mulcahy and McLoughlin 2016). The presence of S. aureus in the oral cavity is underestimated as well (Smith et al. 2003). It is also a bacterium responsible for invasive, life-threatening infections, and unfortunately, its strains demonstrate increased antimicrobial resistance (Dumitrescu et al. 2010). E. coli is a gram-negative facultative anaerobic bacterium that colonises all mammals (Finegold et al. 1983). It is primarily a colon inhabitant, although it can be found in the upper digestive tract and even in the oral cavity (Foster 2004; Zawadzki et al. 2017). Pathogenic strains are the leading cause of urinal tract infections (Guglietta 2017). E. faecalis is a gram-positive commensal of the digestive system. Like the previously mentioned bacteria, it can have a pathogenic effect, causing infections of the urinary tract, bacteraemia and endocarditis (Huycke et al. 1998).
Ciprofloxacin is a second-generation fluoroquinolone antibiotic with a wide activity spectrum (Oliphant and Green 2002). It was introduced into the market in 1987 (Torok et al. 2009). Initially, it was very effective even against methicillin-resistant S. aureus (Righter 1987), and although S. aureus strains are currently more resistant to it, it is still the drug of choice (Suleiman et al. 2012). Ciprofloxacin in combination with other antimicrobials can be effective against E. faecalis, although it is not the first antibiotic of choice (Holmberg et al. 2012). Moreover, ciprofloxacin affects commensal enterococci (de Lastours et al. 2017). Ampicillin is a broad-spectrum penicillin antibiotic used to treat gram-positive and gram-negative bacteria. It is effective against S. aureus but not against MRSA (Foxley et al. 2016). E. coli is often resistant to ampicillin (Vranic and Uzunovic 2016), while infections caused by some resistant strains of E. faecalis can be successfully treated with ampicillin (Conceição et al. 2014).
The interactions among the described bacteria, nickel and antibiotics are multifold. Although bacteria may benefit from lower concentrations of nickel (Kaluarachchi et al. 2010), higher concentrations have been shown to inhibit their growth (Macomber and Hausinger 2011). For the last 20–25 years, an interesting phenomenon has been described and intensively studied. Various strains of bacteria grown in the presence of subinhibitory concentrations of heavy metals, such as mercury, cobalt, copper, zinc and nickel, demonstrated resistance to these same metals. More significantly, bacteria that adapted to heavy metals demonstrated higher resistance to antibiotics (Resende et al. 2012; Calomiris et al. 1984; Nyamboya et al. 2013). The occurrence of strain resistance to antibiotics is one of the greatest challenges in modern medicine (Zaman et al. 2017). Moreover, metals can modulate an antibiotic effect. Both synergistic and antagonistic relationships between metals and antibiotics have been observed (Wolska et al. 2012; Freitas et al. 2018).
The aim of this study was to assess the concentrations of nickel ions that have a bacteriostatic effect on commensal bacteria. Furthermore, the potential interactions of nickel, antibiotics and commensal bacteria were tested.
Materials and methods
Strains and growth media
Staphylococcus aureus strain ATCC 29213 (American Type Cell Culture), Escherichia coli ATCC 25922 and Enterococcus faecalis ATCC 29212 were used. The bacteria were kept frozen at − 80 °C with the addition of 10% glycerol. For each experiment, an aliquot was thawed and grown in Mueller–Hinton (MH) broth (Biolife Italiana, Milano, Italy) for 24 h at 37 °C and then subcultured on Mueller–Hinton (MH) agar (Biolife Italiana, Milano, Italy). The concentration of bacteria was determined by measuring the optical density (OD) at 600 nm. An OD of 1 at 600 nm corresponded to approximately 1 × 109 CFU/mL (colony forming units per mL). Three series of tenfold dilutions were made to obtain a bacterial suspension of 106 CFU/mL. Bacterial inocula were later verified by diluting, plating the dilutions onto MH agar, and incubating for 24 h at 37 °C.
Preparation of reagents
All reagents used were of analytical or molecular biology grade and purchased from Sigma-Aldrich. Stock solution of NiCl2 × 6H2O (Sigma-Aldrich, St. Louis, USA) was prepared in double-distilled water, adjusted to pH 7, passed through a 0.45-µm syringe filter and stored at 4 °C. The stock concentration was 8000 mg/L. Stock solutions of ciprofloxacin and ampicillin (Sigma-Aldrich, St. Louis, USA) were prepared in sterile saline solution (0.9% NaCl) and passed through a 0.45-µm syringe filter. The working concentrations of the NiCl2 × 6H2O solution were prepared by diluting the stock solution to reach concentrations of 2000–125 mg/L.
Determination of minimum inhibitory concentration (MIC)
A resazurin-based microdilution method was used to determine the minimum inhibitory concentrations (MICs) of nickel and ciprofloxacin, which were used in the checkerboard method described below. Serial twofold dilutions of reagents ranging from 2000 to 125 mg/L for nickel, 0.08 to 5 mg/L for ciprofloxacin and 0.12 to 4 mg/L for ampicillin were made in a microtiter plate (Vacutest Kima s.r.l., Italy). Bacterial suspension (1 × 106 CFU/mL per well) and resazurin (0.015% solution) (Sigma-Aldrich, St. Louis, USA) were added to each well. Three wells were used as sterility controls, and three were used as growth controls. After 24 h of incubation at 37 °C, the plates were read visually. The lowest concentration that did not show a change in colour (blue) was defined as the MIC. All dilutions were inoculated on MH agar and incubated for 24 h at 37 °C.
Checkerboard synergy method
To examine the interactions of metals and antibiotics and their effects on bacterial growth, a checkerboard method was used. Stock solutions and serial twofold dilutions of nickel and ciprofloxacin to at least twofold MIC were prepared in MH broth and distributed into the wells of a sterile microtiter plate. The metal of the combination was serially diluted along the ordinate, while the antibiotic was diluted along the abscissa. A bacterial inoculum of 1 × 106 CFU/mL in MH broth was prepared from each bacterial species and added, with resazurin (0.015% solution), to the wells with diluted reagents to reach a final volume of 200 µL. With this preparation process, different combinations of antibiotic and metal concentrations were obtained, and the concentration of metals diminished by rows while that of antibiotics diminished by columns. Columns 1 and 12 and rows A and H were filled with distilled water to prevent the inner wells from drying out. Column 2 was filled with nickel solution and served as a control and MIC confirmation. Row B, analogously, was a ciprofloxacin or ampicillin solution control. Rows C–G and columns 3–11 were filled with various combinations of nickel and ciprofloxacin or ampicillin. The plates were incubated at 37 °C for 24 h under aerobic conditions. Then, the growth of bacteria in the wells was read visually by the change in the colour of resazurin to provide insight into the wells of interest, which were further investigated.
The interactions between various concentrations of the antibiotics ciprofloxacin and ampicillin with nickel were assessed by the fractional inhibitory concentrations (FICs). FIC was calculated in the following manner:
Interaction was defined as synergic when ΣFIC < 0.5, additive when 0.5 ≤ ΣFIC ≤ 1, indifferent when 1 < ΣFIC ≤ 4 and antagonistic when ΣFIC > 4 (Tserennadmid et al. 2011).
Growth curve assay for the determination of the interaction of metals and antibiotics
After screening with the resazurin checkerboard method, new checkerboard plates were prepared as previously described and incubated in a microplate reader (Microplate Reader ELX 808, Biotek, Vermont, USA) for 24 h to obtain growth curves with measurements of optical density (OD) every hour. Measurements were performed in triplicate. Growth curves of bacteria not exposed to nickel and antibiotics were compared to those exposed to various combinations of different concentrations.
The exponential (log) phase of bacterial growth was evaluated by constructing a logarithmic line of the phase and determining the linear function \(y=ax+b\), where “a” is the slope of the line, i.e., the growth rate or speed of the log phase. ANOVA and the Student–Neuman–Keuls test were performed for statistical analysis. The effect size, i.e., the magnitude of the difference between the experimental conditions and the amount of variability accounting for the experimental conditions, was assessed by r, R2 and η2. The following criteria were used for interpretation: r < 0.1 = insignificant effect size, 0.1–0.3 = small effect size, 0.3–0.5 = medium, 0.5–0.7 = large and > 0.7 very large effect size; for squared values R2 and η2, 0.02–0.13 = small effect size, 0.13–0.26 = medium and > 0.26 = large effect size (Rosenthal 1996). Statistical data were obtained using commercial statistical software IBM SPSS (IBM Corp, Armonk, NY, SPSS).
Results
MIC of ampicillin, ciprofloxacin and Ni
The MIC for ampicillin was 1 mg/L for S. aureus and E. faecalis and 2.5 mg/L for E. coli. The MICs for ciprofloxacin obtained for E. faecalis were 0.31 mg/L and 0.62 mg/L for S. aureus and 0.005 for E. coli. The MIC for nickel was 1000 mg/L for all bacteria.
ΣFIC
The ΣFIC values for all three bacteria are presented in Table 1 for ciprofloxacin and Table 2 for ampicillin.
Growth rates of S. aureus
The concentration of ciprofloxacin significantly decreased the growth rate of S. aureus with a very large effect size and a threshold concentration of 0.62 mg/L in comparison to 0.31 mg/L (0.037 ± 0.032 vs. 0.149 ± 0,024; p < 0.001; η2 = 0.938). At a nickel concentrations of 500 mg/L, 1.25 mg/L ciprofloxacin blocked the growth rate in comparison to 0.62 mg/L and lower (p < 0.001; η2 = 0.873), while at nickel concentrations of 125 and 250 mg/L, 0.31 mg/L ciprofloxacin decelerated the growth compared to lower concentrations starting with 0.16 mg/L (0.068 ± 0.054 vs. 0.156 ± 0.048 and 0.087 ± 0.059 vs. 0.158 ± 0.034, p < 0.001; η2 = 0.890 and 0.913, respectively). There was no bacterial growth at 1000 and 2000 mg/L nickel.
Regarding ampicillin, the concentration that significantly decreased the growth rate in comparison to lower concentrations was 2 µg/mL with a very large effect size (0 ± 0 vs. 0.132 ± 0.029; p < 0.001; η2 = 0.898). At a nickel concentration of 125 µg/mL, 1 µg/mL ampicillin was the threshold concentration that significantly decreased the growth rate (0.102 ± 0.088 vs. 0.200 ± 0.019, p < 0.001; η2 = 0.871).
Growth rates of E. faecalis
The concentration of ciprofloxacin was a significant decelerator of the acceleration phase of the growth of E. faecalis, with a very large effect size and a threshold concentration of 0.31 mg/L (0.043 ± 0.075; p < 0.001; η2 = 0.729). That concentration did not differ significantly from 0.16 and 0.08, but it did differ from bacteria without ciprofloxacin (0.177 ± 0.005). At a nickel concentration of 250 mg/L, the concentration of ciprofloxacin was a significant decelerator of growth with a large effect size (p = 0.003; η2 = 0.703), with a concentration of 0.62 blocking growth. At nickel concentrations of 125 and 500 mg/L, there were no detected threshold concentrations of ciprofloxacin that significantly decelerated the growth rate in comparison to other concentrations.
The concentration of ampicillin that significantly decreased the growth rate in comparison to lower concentrations was 1 mg/L (0.052 ± 0.090 vs. 0.182 ± 0.020; p < 0.001; η2 = 0.886). At a nickel concentration of 125 mg/L, the concentration of ampicillin was 0.5 mg/L (0.0 ± 0.0 vs. 0.177 ± 0.71, p < 0.001, η2 = 0.908). At 250 mg/L nickel, the threshold concentration of ampicillin was 0.5 mg/L, and at 500 mg/L nickel, the threshold concentration was 0.25 mg/L ampicillin (p < 0.001, η2 = 0.980).
Growth rates of E. coli
The threshold concentration of ciprofloxacin that significantly decreased the growth rate of E. coli was 0.005 mg/L (p < 0.001; η2 = 0.998). When combined with nickel concentrations of 125 mg/L and 250 mg/L, the concentration of 0.005 mg/L ciprofloxacin was again the threshold. At 500 mg/L nickel, the threshold concentration that significantly decreased the growth rates in comparison to the lower concentration was 0.04 mg/L ciprofloxacin (p < 0.001; η2 = 0.680).
For ampicillin, the threshold concentration was 2.5 mg/L with a large effect size (0.075 ± 0.048 vs. 0.230 ± 0.030; p < 0.001; η2 = 0.959). In 125 and 250 mg/L nickel, the threshold concentration of ampicillin was the same (p < 0.001, η2 = 0.970 and η2 = 0.986).
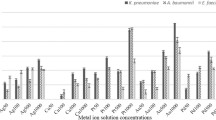
Growth curves OD/t
The growth curves of bacteria demonstrated the synergistic effect of 2.5 mg/L ampicillin and 500 mg/L nickel on E. coli. Similar results were observed for E. faecalis at concentrations of 1 mg/L ampicillin and 500 mg/L nickel (Fig. 1). The growth curves of S. aureus showed no synergism or antagonism between ampicillin and nickel.
At concentrations of 0.31 mg/L ciprofloxacin and 125 mg/L nickel, a synergistic effect was observed on the growth curves of S. aureus (Fig. 2). Antagonistic effects were seen for ciprofloxacin and nickel on the bacterial growth of E. faecalis and E. coli. For E. coli, a nickel concentration of 250 mg/L acted antagonistically on 0.005 mg/L ciprofloxacin (Fig. 2). The same was observed in E. faecalis for 500 mg/L nickel and 0.62 mg/L ciprofloxacin (Fig. 2).
Growth curves of S. aureus, E. faecalis and E. coli and in different ciprofloxacin and nickel concentrations (Ni, nickel - concentrations in 0, 125 and 500; cip, ciprofloxacin - concentrations in 0, 0.31 and 0.62; curve displays mean values of optical density - OD at 600 nm throughout 24 h, measured in triplicate)
Discussion
The MIC for ciprofloxacin obtained for S. aureus was slightly higher than the values according to EUCAST, which were in the range of 0.125–0.5 mg/L, although a different method was used. The inhibitory concentrations for E. faecalis and E. coli were in concordance with EUCAST, where ranges of 0.25–2 mg/L and 0.004–0.016 mg/L were reported. The MICs for ampicillin against E. faecalis and E. coli were consistent with the EUCAST ranges of 0.5–2 and 2–8 mg/L, respectively (European Committee on Antimicrobial Susceptibility Testing 2019).
This study found similar inhibitory concentrations of nickel to those in previous research performed on multiple bacteria. The range of nickel minimum inhibitory concentrations was 512–1024 mg/L. The bacteria tested were enterobacteria, nonfermenting gram-negative rods and gram-positive cocci from water samples (Resende et al. 2012).
The growth rates of S. aureus made it evident that the concentration of ciprofloxacin decelerates the exponential phase of growth, with the concentration of 0.62 mg/L being the threshold for significant deceleration, confirming the MIC results. When 125 or 250 mg/L nickel was present, the threshold deteriorated to 0.32 mg/L ciprofloxacin. It seems that some concentrations of Ni might have a synergistic effect with ciprofloxacin on the growth rate of S. aureus. Nickel concentration also had a significant effect on the exponential phase of growth. Although some synergism was statistically observed, the FIC results demonstrated no synergism or antagonism between ciprofloxacin and nickel on S. aureus growth. A similar result was found in a study that evaluated the synergistic effect of bismuth sulfide and ciprofloxacin (Ma et al. 2017).
Ampicillin and nickel had a synergistic effect on the growth of E. faecalis and E. coli with no effect seen on the growth of S. aureus. A study from 2016 demonstrated a synergistic effect of zinc oxide and ampicillin on an array of bacterial strains (Sharma et al. 2016). A synergistic effect of beta lactam antibiotics and ions of copper, silver and zinc was also observed (Möhler et al. 2017).
The ciprofloxacin concentration decelerated the growth of E. faecalis, as did the nickel concentration. A concentration of 0.31 mg/L was the cut-off that decelerated exponential growth when no nickel was added.
Interestingly, the FIC results showed an antagonistic relationship of the antibiotic and metal in E. faecalis and E. coli, which is most pronounced at a nickel concentration of 500 mg/L. Growth curves corroborate these results.
There are two main explanations for this phenomenon. One is that the chelation of metals and antibiotics invokes a decreased antimicrobial effect (Chen et al. 2015). The second is the occurrence of bacterial resistance, as it has been shown that the presence of heavy metals stimulates the expression of genes in bacteria that are responsible for various mechanisms of antimicrobial resistance. Specifically, bacteria that become resistant to nickel demonstrate the activation of efflux pumps, the elimination of nickel via vacuoles and the production of nickel sulfides to decrease the concentration of nickel in nearby surroundings (Macomber and Hausinger 2011). Efflux pumps are a significant contributor to resistance to fluoroquinolones, especially in strains demonstrating very elevated MIC values (Everett et al. 1996).
The results of this study might imply several interesting phenomena. First, nickel has an antagonistic effect on antibiotics. Further research might elucidate whether elevated nickel intake or the long-term presence of dental devices and appliances that corrode might lead to interference with antibiotic treatment. Second, the highest antagonism of metal against antibiotics was at a subinhibitory concentration of nickel, 500 mg/L. The importance of subinhibitory concentrations of heavy metals and antibiotics as a promotor of resistance development has already been emphasised in scientific evidence (Zhang et al. 2018; Bhattacharya et al. 2017).
Additionally, it seems that bacterial type plays a role in the mutual effect of nickel and ciprofloxacin, which additionally implies that the bacterial resistance mechanism could be the reason for diminished antimicrobial susceptibility. However, one can hypothesise that the 24-h incubation performed in this study might not be enough for the occurrence of this phenomenon.
In vitro studies that measured the levels of nickel in saliva reported a concentration of 0.414 mg/L released from Ni–Cr dental alloys (Reclaru et al. 2012), 0.0269 ppm/day from stainless steel dental crowns (Ramazani et al. 2014) and 27.04 µg/day from orthodontic wires (Katic et al. 2017). In vivo studies show salivary levels of nickel in orthodontic patients to be 0.0853 mg/L (Gölz et al. 2016), and nickel found in the oral mucosa cells of orthodontic patients ranged up to 0.0217 mg/L (Downarowicz and Mikulewicz 2017). Although these concentrations are significantly lower than those causing interactions with ciprofloxacin or bacteria, it is difficult to assess the cumulative concentration to which bacteria could be exposed. Additionally, it should be emphasised that orthodontic treatment lasts approximately 2.5 years, during which time appliances remain in the oral cavity and release nickel ions by corrosion (Wang et al. 2018). Perhaps a collection of commensal bacteria in patients with dental devices and orthodontic appliances could provide an answer.
Overall, it seems that nickel could have repercussions on the human body more important than the direct effect on human cells, namely, its influence on the human microbiota and interference with antibiotics. Additionally, nickel in the body could interfere with the uptake of antibiotics, although further research is necessary to elucidate the causal inference.
A study with longer exposure of bacteria is definitely needed to confirm the potential adaptation to nickel and the development of resistance mechanisms.
Availability of data and materials
Data are available.
References
Atieh MA, Ji Y, Kochkodan V (2017) Metals in the environment: toxic metals removal. Bioinorg Chem Appl 4309198
Bhattacharya G, Dey D, Das S, Banerjee A (2017) Exposure to sub-inhibitory concentrations of gentamicin, ciprofloxacin and cefotaxime induces multidrug resistance and reactive oxygen species generation in meticillin-sensitive Staphylococcus aureus. J Med Microbiol 66:762–769
Calomiris JJ, Armstrong JL, Seidler RJ (1984) Association of metal tolerance with multiple antibiotic resistance of bacteria isolated from drinking water. Appl Environ Microbiol 47:1238–1242
Chen S, Li X, Sun G, Zhang Y, Su J, Ye J (2015) Heavy metal induced antibiotic resistance in bacterium LSJC7. Int J Mol Sci 29:23390–23404
Conceição N, da Silva LE, Darini AL, Pitondo-Silva A, de Oliveira AG (2014) Penicillin-resistant, ampicillin-susceptible Enterococcus faecalis of hospital origin: pbp4 gene polymorphism and genetic diversity. Infect Genet Evol 28:289–295
de Lastours V, Maugy E, Mathy V, Chau F, Rossi B, Guérin F, Cattoir V, Fantin B, CIPHARES Study Group (2017) Ecological impact of ciprofloxacin on commensal enterococci in healthy volunteers. J Antimicrob Chemother 72:1574–1580
Dickinson AW, Power A, Hansen MG, Brandt KK, Piliposian G, Appleby P, O’Neill PA, Jones RT, Sierocinski P, Koskella B, Vos M (2019) Heavy metal pollution and co-selection for antibiotic resistance: A microbial palaeontology approach. Environ Int 132:105–117
Downarowicz P, Mikulewicz M (2017) Trace metal ions release from fixed orthodontic appliances and DNA damage in oral mucosa cells by in vivo studies: A literature review. Adv Clin Exp Med 26:1155–1162
Dumitrescu O, Dauwalder O, Boisset S, Reverdy MÉ, Tristan A, Vandenesch F (2010) Staphylococcus aureus resistance to antibiotics: key points in. Med Sci (paris) 26:943–949
European Committee on Antimicrobial Susceptibility Testing (2019) Routine and extended internal quality control for MIC determination and disk diffusion as recommended by EUCAST. Version 9.0. http://www.eucast.org. Accessed Date September 14, 2020
Everett MJ, Jin YF, Ricci V, Piddock LJ (1996) Contributions of individual mechanisms to fluoroquinolone resistance in 36 Escherichia coli strains isolated from humans and animals. Antimicrob Agents Chemother 40:2380–2386
Finegold SM, Sutter VL, Mathisen GE (1983) Normal indigenous intestinal microflora. In: Hentges DJ (ed) Human intestinal microflora in health and disease. New York, N.Y. : Academic Press, Inc, p 3–31
Flyvholm MA, Nielsen GD, Andersen A (1984) Nickel content of food and estimation of dietary intake. Z Lebensm Unters Forsch 179:427–431
Foster JW (2004) Escherichia coli acid resistance: tales of an amateur acidophile. Nat Rev Microbiol 2:898–907
Foxley MA, Friedline AW, Jensen JM, Nimmo SL, Scull EM, King JB, Strange S, Xiao MT, Smith BE, Thomas KJ III, Glatzhofer DT, Cichewicz RH, Rice CV (2016) Efficacy of ampicillin against methicillin-resistant Staphylococcus aureus restored through synergy with branched poly(ethylenimine). J Antibiot (Tokyo) 69:871–878
Freitas TS, Oliveira FS, Cruz RP, Pereira R, Silva A, Moura J, Luz-Lima C, Viana BC, da Silva JH, Freire P, Coutinho H (2018) Modulation of antibiotic effect by Fe2(MoO4)3 microstrutures. Eur J Pharm Sci 123:295–300
Gölz L, Knickenberg AC, Keilig L, Reimann S, Papageorgiou SN, Jäger A, Bourauel C (2016) Nickel ion concentrations in the saliva of patients treated with self-ligating fixed appliances: a prospective cohort study. J Orofac Orthop 77:85–93
Guglietta A (2017) Recurrent urinary tract infections in women: risk factors, etiology, pathogenesis and prophylaxis. Future Microbiol 12:239–246
Holmberg A, Mörgelin M, Rasmussen M (2012) Effectiveness of ciprofloxacin or linezolid in combination with rifampicin against Enterococcus faecalis in biofilms. J Antimicrob Chemother 67:433–439
Huycke MM, Sahm DF, Gilmore MS (1998) Multiple-drug resistant enterococci: the nature of the problem and an agenda for the future. Emerg Infect Dis 4:239–249
Jamshidi S, Rahmati Kamel M, Mirzaie M, Sarrafan A, Khafri S, Parsian H (2018) Evaluation of scalp hair nickel and chromium level changes in patients with fixed orthodontic appliance: a one-year follow-up study. Acta Odontol Scand 76:1–5
Kaluarachchi H, Chan Chung KC, Zamble DB (2010) Microbial nickel proteins. Nat Prod Rep 27:681–694
Katic V, Curkovic L, Bosnjak MU, Peros K, Mandic D, Spalj S (2017) Effect of pH, fluoride and hydrofluoric acid concentration on ion release from NiTi wires with various coatings. Dent Mater J 36:149–156
Ley RE, Peterson DA, Gordon JI (2006) Ecological and evolutionary forces shaping microbial diversity in the human intestine. Cell 24:837–848
Ma L, Wu J, Wang S, Yang H, Liang D, Lu Z (2017) Synergistic antibacterial effect of Bi2S3 nanospheres combined with ineffective antibiotic gentamicin against methicillin-resistant Staphylococcus aureus. J Inorg Biochem 168:38–45
Macomber L, Hausinger RP (2011) Mechanisms of nickel toxicity in microorganisms. Metallomics 3:1153–1162
Möhler JS, Kolmar T, Synnatschke K, Hergert M, Wilson LA, Ramu S, Elliott AG, Blaskovich MA, Sidjabat HE, Paterson DL, Schenk G, Cooper MA, Ziora ZM (2017) Enhancement of antibiotic-activity through complexation with metal ions - Combined ITC, NMR, enzymatic and biological studies. J Inorg Biochem 167:134–141
Mulcahy ME, McLoughlin RM (2016) Host–bacterial crosstalk determines Staphylococcus aureus nasal colonization. Trends Microbiol 24:872–886
Nicolas-Chanoine MH, Blanco J, Leflon-Guibout V, Demarty R, Alonso MP, Canica MM, Park YJ, Lavigne JP, Pitout J, Johnson JR (2008) Intercontinental emergence of Escherichia coli clone O25:H4-ST131 producing CTX-M-15. J Antimicrob Chemother 61:273–281
Nyamboya RA, Okemo PO, Ombori O (2013) Heavy metal and antibiotic resistance of fecal pathogens from wastewaters of abattoirs in Nairobi. J Appl Biosci 64:4858–4866
O’Hara AM, Shanahan F (2006) The gut flora as a forgotten organ. EMBO Rep 7:688–693
Oliphant CM, Green GM (2002) Quinolones: a comprehensive review. Am Fam Physician 65:455–464
Price LB, Hungate BA, Koch BJ, Davis GS, Liu CM (2017) Colonizing opportunistic pathogens (COPs): the beasts in all of us. PLoS Pathog 13:e1006369
Ramazani N, Ahmadi R, Darijani M (2014) Assessment of nickel release from stainless steel crowns. J Dent (Tehran) 11:328–334
Reclaru L, Unger RE, Kirkpatrick CJ, Susz C, Eschler PY, Zuercher MH, Antoniac I, Lüthy H (2012) Ni-Cr based dental alloys; Ni release, corrosion and biological evaluation. Mater Sci Eng C Mater Biol Appl 32:1452–1460
Resende JA, Silva VL, Fontes CO, Souza-Filho JA, Rocha de Oliveira TL, Coelho CM, César DE, Diniz CG (2012) Multidrug-resistance and toxic metal tolerance of medically important bacteria isolated from an aquaculture system. Microbes Environ 27:449–455
Righter J (1987) Ciprofloxacin treatment of Staphylococcus aureus infections. J Antimicrob Chemother 20:595–597
Rosenthal JA (1996) Qualitative descriptors of strength of association and effect size. J Soc Serv Res 21:37–59
Sharma N, Jandaik S, Kumar S (2016) Synergistic activity of doped zinc oxide nanoparticles with antibiotics: ciprofloxacin, ampicillin, fluconazole and amphotericin B against pathogenic microorganisms. An Acad Bras Cienc 88:1689–1698
Smith AJ, Robertson D, Tang MK, Jackson MS, MacKenzie D, Bagg J (2003) Staphylococcus aureus in the oral cavity: a three-year retrospective analysis of clinical laboratory data. Br Dent J 195:701–703
Suleiman IA, Bamiro BS, Tayo F (2012) Cost effectiveness of three drugs for the treatment of S. aureus infections in Nigeria. Int J Clin Pharm 34:739–745
Thyssen JP, Linneberg A, Menné JJD (2007) The epidemiology of contact allergy in the general population—prevalence and main findings. Contact Dermatitis 57:287–299
Torok E, Moran E, Cooke F (2009) Oxford handbook of infectious diseases and microbiology. OUP, Oxford
Tserennadmid R, Takó M, Galgóczy L, Papp T, Pesti M, Vágvölgyi C, Almássy K, Krisch J (2011) Anti yeast activities of some essential oils in growth medium, fruit juices and milk. Int J Food Microbiol 144:480–486
Vranic SM, Uzunovic A (2016) Antimicrobial resistance of Escherichia coli strains isolated from urine at outpatient population: a single laboratory experience. Mater Sociomed 28:121–124
Wang B, Li L (2015) Who determines the outcomes of HBV exposure? Trends Microbiol 23:328–329
Wang B, Yao M, Lv L, Ling Z, Li L (2007) The human microbiota in health and disease. Engineering 3:71–82
Wang Y, Liu C, Jian F, McIntyre GT, Millett DT, Hickman J, Lai W (2018) Initial arch wires used in orthodontic treatment with fixed appliances. Cochrane Database Syst Rev 7:CD007859
Wendl B, Wiltsche H, Lankmayr E, Winsauer H, Walter A, Muchitsch A, Jakse N, Wendl M, Wendl T (2017) Metal release profiles of orthodontic bands, brackets, and wires: an in vitro study. J Orofac Orthop 78:494–503
Wolska KI, Grześ K, Kurek A (2012) Synergy between novel antimicrobials and conventional antibiotics or bacteriocins. Pol J Microbiol 61:95–104
Zaman SB, Hussain MA, Nye R, Mehta V, Mamun KT, Hossain N (2017) A review on antibiotic resistance: alarm bells are ringing. Cureus 9:e1403
Zawadzki PJ, Perkowski K, Padzik M, Mierzwińska-Nastalska E, Szaflik JP, Conn DB, Chomicz L (2017) Examination of oral microbiota diversity in adults and older adults as an approach to prevent spread of risk factors for human infections. Biomed Res Int 8106491
Zhang Y, Gu AZ, Cen T, Li X, He M, Li D, Chen J (2018) Sub-inhibitory concentrations of heavy metals facilitate the horizontal transfer of plasmid-mediated antibiotic resistance genes in water environment. Environ Pollut 237:74–82
Acknowledgements
We thank Andrea Bukša, associate professor Željka Maglica and Hrvoje Križan for their help in the research.
Funding
This work has been supported by the following projects of the Croatian Science Foundation “Immunological and regenerative implications of corrosion of dental materials in children and adolescents” (IP-2014–09-7500) and “Environmental factors and microbial interactions in the structure of the dental biofilm” (IP-2020–02-4027).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pavlić, A., Gobin, I., Begić, G. et al. The effect of nickel ions on the susceptibility of bacteria to ciprofloxacin and ampicillin. Folia Microbiol 67, 649–657 (2022). https://doi.org/10.1007/s12223-022-00960-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-022-00960-x