Abstract
Limited treatment options in infectious diseases caused by resistant microorganisms created the need to search new approaches. Several herbal extracts are studied for their enormous therapeutic potential. Silymarin extract, from Silybum marianum (milk thistle), is an old and a new remedy for this goal. The purpose of this study is to evaluate the antibacterial and antiadherent effects of silymarin besides biofilm viability activity on standard bacterial strains. Minimal inhibitory concentration (MIC), minimal bactericidal concentration (MBC), antiadherent/antibiofilm activity, and effects on biofilm viability of silymarin were evaluated against standard bacterial strains. MIC values were observed between 60 and >241 μg/mL (0.25–>1 mmol/L). Gram-positive bacteria were inhibited at concentrations between 60 and 120 μg/mL. Gram-negative bacteria were not inhibited by the silymarin concentrations included in this study. MBC values for Gram-positive bacteria were greater than 241 μg/mL. Adherence/biofilm formations were decreased to 15 μg/mL silymarin concentration when compared with silymarin-untreated group. Silymarin reduced the biofilm viabilities to 13 and 46 % at 1 and 0.5 mmol/L concentrations, respectively. We demonstrated that silymarin shows antibacterial and antiadherent/antibiofilm activity against certain standard bacterial strains which may be beneficial when used as a dietary supplement or a drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Silybum marianum, commonly known as milk thistle, has been used from ancient times as herbal extract. The plant is indigenous for different parts of the world such as Europe, the USA, and South Africa (www.cancer.gov; Lahlah et al. 2012). Nowadays, it has been preferred as an alternative medicine in some countries (Bibi et al. 2011). Milk thistle is available in the USA as a dietary supplement. It is prescribed in Europe for its safety and well tolerance (Post-White et al. 2007; Ramasamy and Agarwal 2008; Ghosh et al. 2010; www.cancer.gov).
The active constituents of milk thistle are obtained from its dried seeds. The seeds contain approximately 70 to 80 % silymarin and 20 to 30 % chemically undefined fraction composed of polymeric and oxidized polyphenolic compounds. Silymarin is a mixture of flavonolignan isomers: silybin, isosilybin, dehydrosilybin, silychristin, silydianin, and a few flavonoids mainly taxifolin (Sanchez-Sampedro et al. 2007; Simánek et al. 2000). Among these isomers, the major and the most active component is silybin or the synonymous silibinin, which is responsible for its main biological effects. Either silymarin- or silybin-containing products are used in Europe as Legalon®, Thisilyn®, Siliphos®, and Silipide® (Ramasamy and Agarwal 2008; Polyak et al. 2013).
The well-known in vitro effects of silymarin are its antioxidant, anti-inflammatory, anticarcinogenic, antimetastatic, antifibrotic, and antiangiogenic effects and its activity against lipid peroxidation and its ability to stimulate liver regeneration. In clinical trials, its hepatoprotective, antidiabetic, cardioprotective, and antiviral effects were also shown. Silymarin has ability to inhibit some well-known hepatotrop viruses. Its antiviral effectiveness against Hepatitis B and especially Hepatitis C viruses is well defined. However, there are limited data about its antibacterial activity (Gordon et al. 2006; Tamayo and Diamond 2007; Wagoner et al. 2010; Polyak et al. 2013; Wei et al. 2013).
Biofilms are microorganism communities attached to biotic or abiotic surfaces embedded in a extracellular polymeric matrix. Biofilm formation is a multistep process. Colonization and attachment or adherence to a surface are the initial stages (Coenye and Nelis 2010). Biofilms play an essential role in infectious diseases. They especially cause chronic infections in tissues and also may be an infection source by developing on medical devices. Some examples for tissue and medical device-associated biofilms are as follows: chronic lung infections in cystic fibrosis, chronic wound infections, biofilms on orthopedic devices, endotracheal tubes, intravenous catheters, indwelling urinary catheters, etc. (Høiby et al. 2015). Biofilm-based infections are resistant to antibiotics and many other conventional antimicrobial agents (Bjarnsholt 2013). However, there is lack of evidence about antiadherence activity of silymarin, which is vital for biofilm formation.
The main goal of this study is to determine the antibacterial and antiadherent/antibiofilm effects of silymarin as a complex against standard bacterial strains.
Materials and methods
Strains tested
This study includes eight standard American Type Culture Collection (ATCC) strains. Five are Gram-positive bacteria, and three are Gram-negative bacteria. The Gram-positive bacteria are Staphylococcus epidermidis ATCC 12228, S. epidermidis ATCC 35984, Staphylococcus aureus ATCC 29213, Methicillin-resistant S. aureus (MRSA) ATCC 43300, and Enterococcus faecalis ATCC 29212.
The Gram-negative bacteria are extended-spectrum beta-lactamase-producing Klebsiella pneumoniae ATCC 700603, Pseudomonas aeruginosa ATCC 27853, and Escherichia coli ATCC 25922. Each isolate was stored at −20 °C until use. Before test procedure, they were subcultured on 5 % sheep blood containing agar for Gram-positive bacteria for the determination of contamination and 5 % sheep blood containing agar and MacConkey agar for Gram-negative bacteria for the determination of either contamination or lactose fermentation. After inoculation on appropriate media, bacteria were incubated at 37 °C for 24 h under aerobe conditions in moisturized incubator.
Chemicals
The silymarin powder (S0292, Sigma, USA) and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) (M2003, Sigma) were purchased commercially from the manufacturer. The complex is composed of silybin A, silybin B, isosilybin A, isosilybin B, silychristin, silydianin taxifolin, and apigenin 7-glucoside (approximately 45 % silybin by weight) (www.sigmaaldrich.com). It has been dissolved in dimethyl sulfoxide (DMSO) (Polyak et al. 2010; Gharagozloo et al. 2013). The final concentration of DMSO was never exceeding 1 %.
Minimum inhibitory concentrations for silymarin
The minimum inhibitory concentrations (MICs) of silymarin were determined by a twofold serial broth dilution method in cation-adjusted Mueller-Hinton medium (BD, USA) according to the Clinical and Laboratory Standards Institute (CLSI 2012) recommendations by using sterile U-bottom 96-well polystyrene tissue culture microtiter plates. Twofold serial dilutions of silymarin were ranging from 0.47 to 241 μg/mL (0.5–0.0009 mmol/L). The dilution range also included the achievable peak plasma level of silymarin. Cultures were diluted into microtiter plates to achieve a final inoculum of 105 colony-forming unit (CFU)/mL containing silymarin at various concentrations. A row containing only DMSO was also tested to show the antibacterial effect of the solvent. Wells containing only broth was used as sterility control, and wells containing only bacteria were used as growth control. After 24 h of incubation at 37 °C, the MIC was determined as the lowest concentration of the agent that completely inhibits visible growth as evaluated by the naked eye. MIC values were also determined spectrophotometrically at 570 nm (BioTek Instruments, ELX 800, USA).
Minimum bactericidal concentrations for silymarin
The minimum bactericidal concentrations (MBCs) were determined from broth dilution MIC tests by subculturing to agar plates that do not contain the test agent. The MBC is defined as the lowest concentration of the agent that reduces the viability of the initial bacterial inoculum by ≥99.9 %.
Quantification of biofilm formation
Quantification of biofilm formation was conducted using microtiter plate assay as previously described (Christensen et al. 1985; Stepanovic et al. 2000; Hassan et al. 2011).
S. epidermidis ATCC 12228 and S. epidermidis ATCC 35984 standard strains were used for determination of adherence/biofilm activity. S. epidermidis ATCC 12228 is a well-known nonbiofilm producer standard strain. It has been used as a negative control for determination of adherence/biofilm formation. S. epidermidis ATCC 35984 is a well-known biofilm producer standard strain, and also, it has been used as positive control. Presence of phase variations of bacteria was distinguished on Congo red agar. The predominant colony was selected for further testing.
Test procedure was performed by using sterile flat-bottom 96-well polystyrene tissue culture microtiter plates. All tests were performed in triplicate and repeated for three times. After preparing bacterial inoculum (~106 CFU/mL) in tryptic soy broth, plates were incubated at 37 °C for 24 h. After washing and fixation steps, quantification of adherence/biofilm formation was determined by staining techniques (crystal violet) at two different time periods (30 min and 1 h) by using modified Christensen’s method (Christensen et al. 1985). For the measurement of the results, the absorbance (A) of each well is measured at 570 nm using microtiter plate reader (BioTek Instruments, ELX 800, USA). The results were interpreted according to Hassan et al. (2011) with slight modifications. The cutoff value was obtained from uninoculated medium. The results were interpreted as follows:
Antiadherent/antibiofilm activity of silymarin
Antiadherent/antibiofilm activity of silymarin was also determined in a dose-dependent manner. S. epidermidis ATCC 12228 and S. epidermidis ATCC 35984 standard strains were used for determination of antiadherence/antibiofilm activity. Test procedure was performed by using sterile flat-bottom 96-well polystyrene tissue culture microtiter plates. After serial twofold dilutions of silymarin, bacteria were inoculated at a final concentration of ~106 CFU/mL in tryptic soy broth. The following steps were performed as described in determination of adherence/biofilm activity section. Silymarin concentrations were ranging from 0.47 to 241 μg/mL.
Determination of biofilm viability
MTT assay was performed to determine the biofilm viability according to previous protocols with minor modifications (Walencka et al. 2005; Ji-Lu et al. 2012). After 24-h biofilm formation, each well was emptied. Then, 150 μL phosphate-buffered saline (PBS)/well and 50 μL MTT solution/well (0.3 % PBS) were added. The plate was incubated at 37 °C for 2 h. Well content was emptied and filled with 150 μL DMSO and 25 μL glycine buffer at the end of the incubation period. After incubation at room temperature for 15 min, the absorbencies were determined at 570 nm (Bio Tek ELX 800, Germany).
Results
MICs for silymarin
The silymarin MIC values were ranging from 60 to >241 μg/mL. Gram-positive bacteria were inhibited at concentrations between 60 and 120 μg/mL. There was only twofold dilution difference between Gram-positive bacteria in similar acceptable values. Gram-negative bacteria were not inhibited by the silymarin concentrations included in this study (Table 1).
MBCs for silymarin
MBC values for Gram-positive bacteria were greater than 241 μg/mL.
Antiadherent/antibiofilm activity of silymarin on biofilm nonproducer and producer standard strains
Before silymarin treatment, S. epidermidis ATCC 12228 standard strain was nonadherent/nonbiofilm producer. After dose-dependent silymarin treatment, S. epidermidis ATCC 12228 standard strain was still nonadherent/nonbiofilm producer.
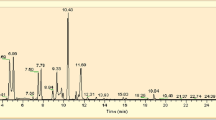
The well-known biofilm producer standard strain S. epidermidis ATCC 35984 showed adherent/biofilm activity. After dose-dependent silymarin treatment, the biofilm producer standard strain S. epidermidis ATCC 35984 was observed as nonadherent/nonbiofilm producer. Antiadherent/antibiofilm activity of silymarin ended at 15 μg/mL (31.25 μmol/L) (Fig. 1).
Determination of biofilm viability
After silymarin treatment, biofilm viability was reduced in a dose-dependent manner. The biofilm viabilities were 13, 46, and 99 % at 1, 0.5, and 0.03 mmol/L concentrations, respectively (Fig. 2).
Discussion
Treatment options are limited in infectious diseases caused by resistant or multidrug-resistant microorganisms. This has created the need to search new approaches. Herbal extracts take place in medicine as an old and a new remedy (Baylan 2010; Edwards-Jones 2013). Although there are various medicinal plants, S. marianum is a widely researched plant because of its safe use, well tolerance, and minimal toxic or adverse effects (Abenavoli et al. 2010; Post-White et al. 2007; Tamayo and Diamond 2007).
In this study, we investigated the antibacterial and antiadherent/antibiofilm effects of silymarin against standard bacterial strains. We evaluated the antibacterial effects of silymarin against several Gram-positive (S. epidermidis ATCC 12228, S. epidermidis ATCC 35984, S. aureus ATCC 29213, MRSA ATCC 43300, and Enterococcus fecalis ATCC 29212) and Gram-negative (extended-spectrum beta-lactamase-producing K. pneumonia ATCC 700603, P. aeruginosa ATCC 27853, and E. coli ATCC 25922) standard bacterial strains. The extract showed antibacterial activity against Gram-positive bacteria. MIC values for Gram-positive bacteria were ranging from 60 to >241 μg/mL. However, Gram negatives were not inhibited. Minimal bactericidal concentrations of silymarin were greater than the concentrations included in this study for Gram-positive bacteria. Even if we could not compare the MICs with previous studies due to the differences in the methods used, with an overall aspect, our results are consistent with Lee et al. (2003) and Lahlah et al. (2012). Thus, silymarin has antibacterial activity especially for Gram positives. Antiviral effects of silymarin were observed both on experimental and clinical settings. Although antiviral action of silymarin is reported as blocking of virus entry and transmission (Tamayo and Diamond 2007; Wagoner et al. 2010), its antibacterial effects are attributed to RNA and protein inhibition (Lee et al. 2003; Lahlah et al. 2012).
Plant-derived extracts have several modes of actions to inhibit different prokaryotic and eukaryotic microorganisms. Some of the components of a plant-derived extract may affect the main component’s behavior. As a result, it is difficult to explain which constituent is responsible for its biological results without making further detailed molecular analysis (Simánek et al. 2000; Cushnie and Lamb 2005; Bakkali et al. 2008; Alviano et al. 2012).
Silymarin which is extracted from milk thistle is a chemical compound composed of several bioactive components. Silybin is one of the major bioactive components of silymarin. It is more potent than silymarin as an antibacterial agent against standard and clinical MRSA strains and some Streptococcus spp. (Lee et al. 2003; Kang et al. 2011; Lee et al. 2012).
The major limitations for some in vitro studies seem to be the type, the source, and the dose of the extract (silymarin, silybin) and as well as the method used (Lee et al. 2003; Kang et al. 2011; Lee et al. 2012; Lahlah et al. 2012). In our study, for obtaining reliable results we neither preferred natural herbal extract nor prescribed forms of silymarin. The dose selection was made according to plasma peak level of silymarin when taken orally (Wen et al. 2008).
There is also lack of information about the type and the effective dose of the extract used for clinical trials (Tamayo and Diamond 2007; Lucey et al. 2009). Promising results about pharmacodynamic, pharmacokinetic, herb-drug interaction, and randomized double-blind clinical studies have been reported for preventive effects of silymarin (Tamayo and Diamond 2007). In a phase I randomized clinical study at a daily dose of 13 g, the achievable peak plasma level of silybin is 100 μmol/L (0.1 mmol/L) (Flaig et al. 2007; www.cancer.gov). Also in vitro studies show that silymarin acts on cancer cell lines in a dose-dependent manner (Agarwal et al. 2003). According to literature and our study results, it may be considered that the type and the dose of the extract used should be taken into account. Although oral administration is approved in clinical trials, intravenous administration is still under investigation (Ramasamy and Agarwal 2008; Polyak et al. 2013).
Biofilm is accumulation of microorganisms found in an extracellular polymeric matrix, different from planktonic cells. The ability of some microorganisms to form biofilms contributes to antibiotic resistance and treatment failures (Hall et al. 2014). Biofilm formation includes multiple steps. The first and the most important step is to adhere or attach to a biotic or abiotic surface. The chronic nature of many infectious diseases is attributed to the formation of bacterial biofilms as they are difficult to treat (Walencka et al. 2006). Particularly intravascular catheters can be the source for biofilm formation and related infections in patients with indwelling devices (Donlan 2001, 2011). As well as antibacterial activity, the impressive finding of our study is that silymarin showed antiadherent/antibiofilm activity against biofilm-forming strain.
Antibiotic susceptibilities between planktonic and biofilm populations differ. The method used for evaluating the minimal inhibitory concentration measures the actions of agents against planktonic organisms especially important for acute infections. However, the MIC alone is not sufficient to evaluate the effectiveness of the agent used. The measurement of bacterial viability plays a major role to evaluate the efficacy of the agents used in the experiment (Ceri et al. 1999; Stoddart 2011). According to our results, silymarin reduced the viability of biofilm-forming cells in a dose-dependent manner lower than MIC values.
In conclusion, we found that silymarin shows antibacterial and antiadherent/antibiofilm activity. To the best of our knowledge, this is the first report about antiadherent/antibiofilm activity of silymarin. The major finding of this study is that the extract shows antiadherent activity at lower doses than MIC value. It can be considered that when silymarin is used as a dietary supplement or a drug, antiadherent/antibiofilm activity may also be beneficial to inhibit the bacterial adherence. This suggests that silymarin may act not only as hepatoprotective, antioxidant, anti-inflammatory, etc. but also as antibacterial and antiadherent. Although each components of silymarin may show different biological activities, we think that antibacterial antiadherent/antibiofilm effects of silymarin as a complex should not be omitted. Finally, our results highlight silymarin in a different aspect which will be important for improving the usage of silymarin as a prescribed agent.
References
Abenavoli L, Capasso R, Milic N, Capasso F (2010) Milk thistle in liver diseases: past, present, future. Phytother Res 24:1423–1432
Agarwal C, Singh RP, Dhanalakshmi S, Tyagi AK, Tecklenburg M, Sclafani RA, Agarwal R (2003) Silibinin upregulates the expression of cyclin-dependent kinase inhibitors and causes cell cycle arrest and apoptosis in human colon carcinoma HT-29 cells. Oncogene 22:271–82
Alviano DS, Barreto AL, Dias Fde A, Rodrigues Ide A, Rosa Mdo S, Alviano CS, Soares RM (2012) Conventional therapy and promising plant-derived compounds against trypanosomatid parasites. Front Microbiol 6(3):283
Bakkali F, Averbeck S, Averbeck D, Idaomar M (2008) Biological effects of essential oils—a review. Food Chem Toxicol 46(2):446–75
Baylan O (2010) Fosfomycin: past, present and future. Mikrobiyol Bul 44:311–321
Bibi Y, Nisa S, Chaudhary FM, Zia M (2011) Antibacterial activity of some selected medicinal plants of Pakistan. BMC Complement Altern Med 11:52
Bjarnsholt T (2013) The role of bacterial biofilms in chronic infections. APMIS Suppl 136:1–51. doi:10.1111/apm.12099
Ceri H, Olson ME, Stremick C, Read RR, Morck D, Buret A (1999) The Calgary biofilm device: new technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J Clin Microbiol 37(6):1771–6
Christensen GD, Simpson WA, Younger JJ, Baddour LM, Barrett FF, Melton DM, Beachey EH (1985) Adherence of coagulase negative staphylococci to plastic tissue cultures: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol 22:996–1006
Clinical and Laboratory Standards Institute (CLSI) (2012) Performance standards for antimicrobial susceptibility testing; twenty-second informational supplement M100-S22. CLSI, Wayne
Coenye T, Nelis HJ (2010) In vitro and in vivo model systems to study microbial biofilm formation. J Microbiol Methods 83:89–105
Cushnie TP, Lamb AJ (2005) Antimicrobial activity of flavonoids. Int J Antimicrob Agents 26(5):343–56
Donlan RM (2001) Biofilm formation: a clinically relevant microbiological process. Healthcare Epidemiology CID 33:1387–1392
Donlan RM (2011) Biofilm elimination on intravascular catheters: important considerations for the infectious disease practitioner. Healthcare Epidemiology CID 52:1039–1045
Edwards-Jones V (2013) Alternative antimicrobial approaches to fighting multi-drug resistant infections. In: Rai M, Kon K (eds) Frightening multidrug resistance with herbal extracts, essential oils and their components. Elsevier, USA, pp 1–9
Flaig TW, Gustafson DL, Su LJ, Zirrolli JA, Crighton F, Harrison GS, Pierson AS, Agarwal R, Glodé LM (2007) A phase I and pharmacokinetic study of silybin-phytosome in prostate cancer patients. Invest New Drugs 25:139–146
Gharagozloo M, Javid EN, Rezaei A, Mousavizadeh K (2013) Silymarin inhibits cell cycle progression and mTOR activity in activated human T cells: therapeutic implications for autoimmune diseases. Basic Clin Pharmacol Toxicol 112(4):251–6
Ghosh A, Ghosh T, Jain S (2010) Silymarin-a review on the pharmacodynamics and bioavailability enhancement approaches. J Pharm Sci Tech 2:348–355
Gordon A, Hobbs DA, Bowden DS, Bailey MJ, Mitchell J, Francis AJ, Roberts SK (2006) Effects of Silybum marianum on serum hepatitis C virus RNA, alanine aminotransferase levels and well-being in patients with chronic hepatitis C. J Gastroenterol Hepatol 21:275–280
Hall MR, McGillicuddy E, Kaplan LJ (2014) Biofilm: basic principles, pathophysiology, and implications for clinicians. Surg Infect (Larchmt) 15(1):1–7
Hassan A, Usman J, Kaleem F, Omair M, Khalid A, Iqbal M (2011) Evaluation of different detection methods of biofilm formation in the clinical isolates. Braz J Infect Dis 15:305–311
Høiby N, Bjarnsholt T, Moser C, Bassi GL, Coenye T, Donelli G, Hall-Stoodley L, Holá V, Imbert C, Kirketerp-Møller K, Lebeaux D, Oliver A, Ullmann AJ, Williams C (2015) ESCMID guideline for the diagnosis and treatment of biofilm infections 2014. Clin Microbiol Infect. doi:10.1016/j.cmi.2014.10.024
http://www.cancer.gov/cancertopics/pdq/cam/milkthistle/HealthProfessional/page1 access: 07/10/2014
http://www.sigmaaldrich.com/catalog/analytical/supelco/g005739?lang=en®ion=TR 02/25/2015
Ji-Lu S, Shao-Kang Z, Jing-Yu C, Bei-Zhong H (2012) Efficacy of acidic and basic electrolyzed water in eradicating Staphylococcus aureus biofilm. Can J Microbiol 58:448–454
Kang HK, Kim HY, Cha JD (2011) Synergistic effects between silibinin and antibiotics on methicillin-resistant Staphylococcus aureus isolated from clinical specimens. Biothecnol J 13:397–408
Lahlah ZF, Meziani M, Maza A (2012) Silymarin natural antimicrobial agent extracted from Silybum marianum. Journal Academia 2:164–169
Lee DG, Kim HK, Park Y, Park SC, Woo ER, Jeong HG, Hahm KS (2003) Gram positive bacteria specific properties of silybin derived from Silbum marianum. Arch Pharm Res 26:597–600
Lee YS, Jang KS, Cha JD (2012) Synergistic antibacterial effect between silibinin and antibiotics in oral bacteria. J Biomed Biotechnol 2012:618081. doi:10.1155/2012/618081
Lucey MR, Mathurin P, Morgan TR (2009) Alcoholic hepatitis. N Engl J Med 360:2758–69
Polyak SJ, Morishima C, Lohmann V, Pal S, Lee DY, Liu Y, Graf TN, Oberlies NH (2010) Identification of hepatoprotective flavonolignans from silymarin. Proc Natl Acad Sci U S A 107(13):5995–9
Polyak SJ, Ferenci P, Pawlotsky JM (2013) Hepatoprotective and antiviral functions of silymarin components in hepatitis C virus infection. Hepatology 57:1262–1271
Post-White J, Ladas EJ, Kelly KM (2007) Advances in the use of milk thistle (Silybum marianum). Integr Cancer Ther 6:104–109
Ramasamy K, Agarwal R (2008) Multitargeted therapy of cancer by silymarin. Cancer Lett 8:352–362
Sanchez-Sampedro A, Kim HK, Choi YH, Verpoorte R, Corchete P (2007) Metabolomic alterations in elicitor treated Silybum marianum suspension cultures monitored by nuclear magnetic resonance spectroscopy. J Biotechnol 130:133–142
Simánek V, Kren V, Ulrichová J, Vicar J, Cvak L (2000) Silymarin: what is in the name…? An appeal for a change of editorial policy. Hepatology 32(2):442–4
Stepanovic S, Vukovic D, Savic B, Svabic-Vlahovic M (2000) A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J Microbiol Methods 40(2):175–9
Stoddart MJ (2011) Cell viability assays: introduction. Methods Mol Biol 740:1–6
Tamayo C, Diamond S (2007) Review of clinical trials evaluating safety and efficacy of milk thistle (Silybum marianum [L.]gaertn.). Integr Cancer Ther 6:146–157
Wagoner J, Negash A, Kane OJ, Martinez LE, Nahmias Y, Bourne N, Owen DM, Grove J, Brimacombe C, McKeating JA, Pécheur EI, Graf TN, Oberlies NH, Lohmann V, Cao F, Tavis JE, Polyak SJ (2010) Multiple effects of silymarin on the hepatitis C virus lifecycle. Hepatology 51:1912–1921
Walencka E, Sadowska B, Rozalska S, Hryniewicz W, Rózalska B (2005) Lysostaphin as a potential therapeutic agent for staphylococcal biofilm eradication. Pol J Microbiol 54(3):191–200
Walencka E, Sadowska B, Rozalska S, Hryniewicz W, Rozalska B (2006) Staphylococcus aureus biofilm as a target for single or repeated doses of oxacillin, vancomycin, linezolid and/or lysostaphin. Folia Microbiol 51:381–386
Wei F, Liu SK, Liu XY, Li ZJ, Li B, Zhou YL, Zhang HY, Li YW (2013) Meta-analysis: silymarin and its combination therapy for the treatment of chronic hepatitis B. Eur J Clin Microbiol Infect Dis 32:657–669
Wen Z, Dumas TE, Schrieber SJ, Hawke RL, Fried MW, Smith PC (2008) Pharmacokinetics and metabolic profile of free, conjugated, and total silymarin flavonolignans in human plasma after oral administration of milk thistle extract. Drug Metab Dispos 36(1):65–72
Acknowledgments
This study was approved by Baskent University Institutional Review Board (Project no: 14/09) and supported by Baskent University Research Fund.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Evren, E., Yurtcu, E. In vitro effects on biofilm viability and antibacterial and antiadherent activities of silymarin. Folia Microbiol 60, 351–356 (2015). https://doi.org/10.1007/s12223-015-0399-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12223-015-0399-6