Abstract
This study aimed to determine the scan delay for bolus tracking in the hepatic artery phase (HAP) of hepatic dynamic computed tomography (CT) using the cardiothoracic ratio (CTR) from CT scout images. We retrospectively studied 188 patients who underwent hepatic dynamic CT, 24 of whom had scan delays adjusted for CTR. The contrast enhancement of the abdominal aorta, portal vein, hepatic vein, and hepatic parenchyma was calculated for HAP. The adequacy of the scan timing for HAP was assessed using three classifications: early, appropriate, or late. The effect of HAP on scan timing adequacy was determined using multivariate logistic regression analysis, and the optimal cutoff value of CTR was evaluated using receiver operating characteristic analysis. The trigger times for bolus tracking (odds ratio: 1.58) and CTR (odds ratio: 1.23) were significantly affected by the appropriate scan timing of the HAP. The optimal cutoff value of CTR was 59.3%. The scan timing of HAP with a scan delay of 15 s was 14% of early and 86% of appropriate, and the proportion of early in CTR ≥ 60% (early, 52%; appropriate, 48%) was higher than that in CTR < 60% (early, 6%; appropriate, 94%). Adjusting the scan delay to 20 s in CTR ≥ 60% increased the proportion of appropriate (early, 4%; appropriate, 96%). The CTR of a CT scout image is an effective index for determining the scan delay for bolus tracking. Adjusting the scan delay by CTR can provide appropriate HAP images in more patients. Trial registration number: R-080; date of registration: 9 March 2023, retrospectively registered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Hepatic dynamic computed tomography (CT) is used to scan hepatic tumors, such as hepatocellular carcinoma [1, 2]. Hepatic arterial phase (HAP) imaging is used to detect hypervascular hepatic tumors [3, 4]. The scan timing of HAP is affected by the patient’s cardiovascular status, such as their cardiac output. As the cardiovascular status reduces, the circulation of contrast medium slows, resulting in delayed contrast bolus arrival and peak arterial enhancement [5,6,7]. Bolus tracking technology can monitor the time of arrival of the contrast medium in the abdominal aorta (trigger time) and can reduce the effect on the patient’s cardiovascular status [8, 9]. The scan delay for bolus tracking has been optimized in previous studies [4, 10,11,12,13]. However, in the current bolus-tracking technique, the scan delay is fixed, and the patient-specific cardiovascular status is not considered. In patients with low cardiovascular status, the arrival of contrast medium is delayed, resulting in earlier timing of HAP imaging [14, 15].
Patients with a low cardiovascular status undergo cardiac enlargement due to reduced cardiac function, resulting in an increased cardiothoracic ratio (CTR) [16, 17]. If CTR is measured on CT scout images and cardiac enlargement is evaluated [18], it is possible to identify patients with a low cardiovascular status who will require early HAP imaging. Thus, we considered that we could determine the scan delay for bolus tracking in these patients using the CTR from CT scout images prior to scanning and acquire appropriately timed HAP images.
This study aimed to investigate the effect of CTR on CT scout images on the timing of HAP in hepatic dynamic CT and evaluate its effectiveness as an index for determining the scan delay for bolus tracking.
2 Materials and methods
2.1 Patients
This retrospective study was approved by the ethics committee of our hospital (No. R-080) and the requirement for patient informed consent was waived. The study population comprised 188 patients (125 males and 63 females; mean age, 71.5 ± 10.9 years; range, 38–92 years) who underwent hepatic dynamic CT at our institute between January 2022 and January 2023. In 24 patients, the scan was performed with a scan delay for bolus tracking adjusted by the CTR determined by changing the scan protocol from September 2022. The exclusion criteria were patients on dialysis and those with a body weight of ≥ 95 kg (administered an iodine dose < 500 mg I/kg).
2.2 CT scan and contrast medium injection
A CT scanner with 320 detector rows (Aquilion ONE Prism edition; Canon medical systems, Otawara, Japan) was used. The CT scanning parameters for both protocols included a tube voltage of 100 kV, detector configuration of 80 × 0.5 mm; pitch factor of, 0.84; rotation time of 0.5 s; and scan field of view of 500 mm. The tube current was varied from 100 to 800 mA to maintain a noise index of 14 with a slice thickness of 5.0 mm and filtered back-projection reconstruction (kernel: FC13) using the automatic tube current modulation technique (volume EC, Canon medical systems). Patients were instructed to hold their breath at the end of exhalation during scanning. The CT images were reconstructed with a slice thickness of 1.0 mm or 2.0 mm with the deep learning reconstruction setting of the advanced intelligent clear-IQ body sharp mild (Canon medical systems).
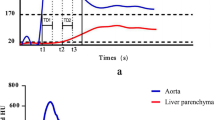
Hepatic dynamic CT images, including unenhanced HAP, portal venous, and equilibrium-phase scans, were obtained. To monitor the arrival of the contrast material, a monitoring scan of a computer-assisted bolus-tracking technique (Real Prep, Canon medical systems) at 100 kV and 15 mAs at 1.0 s intervals was started 20 s after the start of the contrast medium injection. HAP scanning was started automatically 15 or 20 s after contrast enhancement reached 200 Hounsfield units (HU) in the region of interest within the abdominal aorta. Portal venous phase scanning was started 20 s after HAP. The equilibrium phase is delayed by 180 s.
The contrast medium, adjusted to the patient’s body weight (500 mg I/kg), was injected through a 22-gauge catheter into the antecubital vein using a power injector (dual shot-type GX7; Nemoto-Kyorindo, Tokyo, Japan). with a fixed injection duration of 30 s. Contrast medium was selected according to the patient’s body weight (< 47 kg, Omnipaque 240; ≥ 48 kg and < 57 kg, Omnipaque 300, GE healthcare, Tokyo, Japan; ≥ 58 kg and < 73 kg, Iopamiron 370, Bayer, Osaka, Japan; ≥ 73 kg, Optiray 350, Guerbet, Tokyo, Japan).
2.3 Data analysis
Sex, age, body weight, height, and trigger time for bolus tracking were recorded for all patients during the examination. The CTR was defined as the maximum transverse cardiac diameter divided by the maximum transverse lung diameter measured on abdominal CT scout images (Fig. 1). The CT attenuation of the abdominal aorta, portal vein, hepatic vein, and hepatic parenchyma (mean CT attenuation in the right and left hepatic lobes) was measured on unenhanced and HAP images using circular regions of interest. The regions of interest were placed to encompass as much of the vascular lumen as possible, devoid of vascular walls and calcification thrombi in the abdominal aorta. In the portal and hepatic veins, the regions were placed to encompass as much of the vascular lumen as possible while carefully avoiding large vessels, bile ducts, and focal lesions in the hepatic parenchyma. Contrast enhancement was calculated by subtracting the CT attenuation of the unenhanced images from that of the HAP images.
2.4 Evaluation of scan timing for HAP
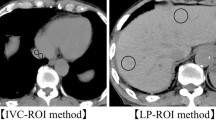
The scan timing adequacy of HAP was assessed using three classifications (early, appropriate, or late). The following contrast enhancements defined these categories [4]: early, portal enhancement < 70 HU, hepatic parenchymal enhancement < 20 HU, and no hepatic venous enhancement; appropriate, portal enhancement ≥ 70 HU and no hepatic venous enhancement: late, hepatic venous enhancement (Fig. 2).
Classification of the scan timing adequacy for the hepatic artery phase. Early portal enhancement of < 70 Hounsfield units (HU) (arrow), hepatic parenchymal enhancement of < 20 HU, and no hepatic venous enhancement (a). Appropriate: portal enhancement ≥ 70 HU (arrow) and no hepatic venous enhancement (b). Late: hepatic venous enhancement (arrowheads) (c)
2.5 Statistical analyses
The continuous variables were expressed as the mean ± standard deviation (SD), and categorical variables were expressed as percentages (numerator/denominator). Comparisons of continuous variables between the two groups were performed using the Mann–Whitney U test. The Chi-squared test was used for categorical variables. Multivariate logistic regression analysis was used to determine the effects of age, weight, trigger time of bolus tracking, CTR on CT scout images, and scan timing of HAP. The optimal cutoff value of CTR to adjust the scan delay for bolus tracking in HAP was evaluated using receiver operating characteristic (ROC) analysis. A p value < 0.05 was considered statistically significant. Statistical analyses were performed using a modified version of the R commander (EZR software) [19], a graphical user interface for R (The R foundation for statistical computing, Vienna, Austria).
3 Results
Multivariate logistic regression analysis showed that the trigger times for bolus tracking (odds ratio: 1.58) and CTR (odds ratio: 1.23) were significantly affected by the scan timing of the HAP (Table 1). ROC analysis showed that the optimal cutoff value of CTR in appropriate scan timing of HAP was 59.3%, with a sensitivity of 73.9%, specificity of 87.9%, and area under the curve of 0.83 (95% confidence interval: 0.73–0.93) (Fig. 3).
Receiver operating characteristic (ROC) curve analysis for appropriate scan timing of the hepatic arterial phase (HAP) by the cardiothoracic ratio (CTR) on computed tomography scout images. The area under the curve was 0.83 with a 95% confidence interval: 0.73–0.93), and the optimal cutoff value of the CTR was 59.3%, with a sensitivity of 73.9% and specificity of 87.9%
The scan timings of HAP with a scan delay of 15 s for bolus tracking were 14% and 86% in the early and appropriate groups, respectively (Table 2). The mean trigger time of bolus tracking in the early group (25.3 s) was delayed by 3.8 s compared to that in the appropriate group (21.5 s). The mean CTR in the early group (61.9%) was higher than that in the appropriate group (54.8%). The mean contrast enhancement of the portal vein and hepatic parenchyma in the early group (portal vein, 54 HU; hepatic parenchyma, 10 HU) was lower than that in the appropriate group (portal vein, 122 HU; hepatic parenchyma, 21 HU). Sex and body weight were significantly different between the early and appropriate groups, whereas the other factors were not significantly different (Table 3). Classified by 60% of CTR, the scan timing of HAP in the patients with CTR ≥ 60% (early group, 52%; appropriate group, 48%) was higher in the early group and lower in the appropriate group compared with that in the patients with CTR < 60% (early group, 6%; appropriate group, 94%) (Table 2).
In the patients with CTR ≥ 60%, the scan timing of the HAP with a scan delay of 20 s for bolus tracking (early group, 4%; appropriate group, 96%) was lower in the early group and higher in the appropriate group compared with that with a scan delay of 15 s for bolus tracking (early group, 52%; appropriate group, 48%) (Table 2, Fig. 4). Age, trigger time for bolus tracking, and CTR were significantly different between the appropriate group and the scan delay of 20 s for bolus tracking; there were no significant differences in the other factors (Table 4).
A 70-year-old man with 64.5% of the cardiothoracic ratio on the abdominal computed tomography scout image (a). A hepatic arterial phase (HAP) image with a scan delay of 15 s for bolus tracking shows poor portal venous enhancement (arrows) and early scan timing for HAP (b). An HAP image with a scan delay of 20 s for bolus tracking shows adequate portal venous enhancement (arrowheads) and is appropriate scan timing for HAP (c)
4 Discussion
We revealed that the CTR on the CT scout image is an index for determining the scan delay for bolus tracking before scanning to obtain the appropriate HAP image in hepatic dynamic CT. The fixed scan delay for bolus tracking did not obtain the appropriate HAP images in several cases, and in particular, a CTR ≥ 60% in patients resulted in delayed trigger time of bolus tracking and higher proportion of early HAP. The CTR on the CT scout image could identify patients with reduced cardiac function and delayed contrast bolus arrival, and adjusting the scan delay for bolus tracking in CTR ≥ 60% produced the appropriate HAP images in more patients.
Cardiac size increases due to reduced cardiac function, which increases the CTR [16, 17]. Circulation of contrast medium is slowed because of decreased cardiac output due to reduced cardiac function, and contrast bolus arrival and peak arterial enhancement are also delayed [5,6,7]. Thus, CTR correlates with cardiac output, and CTR expansion is predicted to decrease cardiac output and slow the circulation of the contrast media. As a result, the trigger time for bolus tracking and the CTR on the CT scout image affected the scan timing of HAP in this study. Previous studies have proposed that the scan delay for bolus tracking can be adjusted by the bolus-tracking software and the trigger time of bolus tracking [14, 15]. However, automated and CT scanner-integrated bolus-tracking software is not currently available as it is non-commercial [15]. In addition, the trigger time for bolus tracking cannot be predicted before scanning, and the scan delay for bolus tracking could not be adjusted [14]. Therefore, we adopted the CTR, which can be measured on CT scout images, as an index to identify patients with reduced cardiac function before scanning and to adjust the scan delay for bolus tracking in the present clinical practice.
The optimal cutoff value of CTR on CT scout images for appropriate HAP imaging was 59.3%. When comparing CTR at 60% of the optimal cutoff value, the proportion of the early group in the patients with CTR ≥ 60% (52%) was higher than that in the patients with CTR < 60% (6%) at a scan delay of 15 s for bolus tracking. Noda et al. suggested that the scan delay for bolus tracking should be adjusted based on the trigger time of bolus tracking [14]. The average trigger time for bolus tracking in the early intervention group (25.3 s) was delayed by approximately 4 s compared with that in the appropriate intervention group (21.5 s). Since scan delay for bolus tracking cannot be individually adjusted before scanning, the scan delay for bolus tracking in the patients with a CTR ≥ 60% was determined to be 20 s.
A scan delay of 20 s for bolus tracking (98%) obtained appropriate HAP images in more patients than that of 15 s (47%) in patients with CTR ≥ 60%. The patients with CTR ≥ 60% were predicted to be scanned during the early timing of HAP because of reduced cardiac function and delayed contrast bolus arrival. Thus, adjusting the scan delay to 20 s showed no significant difference in contrast enhancement of the aorta, portal vein, and hepatic parenchyma in appropriate HAP and improved the proportion of appropriate HAP. However, one patient obtained an earlier HAP image, the trigger time of which was 36.4 s, significantly delayed compared to the mean value. In patients with such a considerable delay in the arrival of the contrast bolus, a scan delay of 20 s for bolus tracking, determined from the difference between the mean trigger times, was limited to obtain appropriate HAP images. Although half of the patients scanned with a scan delay of 15 s for bolus tracking obtained appropriate HAP images, those scanned with a scan delay of 20 s for bolus tracking did not obtain late HAP images. The appropriate time range for HAP is 10–15 s [10, 13], and we believe that even a scan delay of 5 s could result in scans within the appropriate time range for HAP. Therefore, adjusting the scan delay for bolus tracking using the CTR on the CT scout image is effective in current clinical practice.
Impairment of the contrast bolus delivery across the vein, such as thoracic outlet syndrome, delays contrast bolus arrival and peak arterial enhancement [20, 21]. The proportion of early HAP images was 6% in patients with CTR < 60%, and venous impairment was assumed to be the cause of early HAP. In these patients, appropriate HAP images could not be obtained because the scan delay for bolus tracking could not be adjusted. Thus, a bolus-tracking technology that can individually adjust the scan delay is required to obtain appropriate HAP images for all patients.
This study has some limitations. First, the patient population was relatively small and there were significant differences in patient characteristics between the two groups. Second, the monitoring scan for bolus tracking was started 20 s after the administration of the contrast medium to ensure the safety of contrast administration and reduce the radiation dose to the patient caused by the monitoring scan. Therefore, the trigger times before 20 s were not accurately evaluated. Finally, CTR was measured using CT scout image scanning with breath-holding at the end of exhalation. The CTR on the CT scout image is different from breath-holding on inspiration or expiration [22]; consequently, the cutoff value of the CTR for adjusting the scan delay for bolus tracking is different.
5 Conclusion
The scan delay for bolus tracking was fixed and early HAP images were obtained based on the cardiovascular status of the patient on hepatic dynamic CT. The CTR on the CT scout image is an effective index for identifying patients with reduced cardiac function and delayed contrast bolus arrival before scanning and for determining the scan delay for bolus tracking to obtain appropriate HAP images. In the patients with CTR ≥ 60%, the adjustment of scan delay for bolus tracking can produce appropriate HAP images in more patients.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Park S, Joo I, Lee DH, et al. Diagnostic performance of LI-RADS treatment response algorithm for hepatocellular carcinoma: adding ancillary features to MRI compared with enhancement patterns at CT and MRI. Radiology. 2020;296(3):554–61.
Nakamura Y, Higaki T, Honda Y, et al. Advanced CT techniques for assessing hepatocellular carcinoma. Radiol Med. 2021;126(7):925–35.
Murakami T, Kim T, Takamura M, et al. Hypervascular hepatocellular carcinoma: detection with double arterial phase multi-detector row helical CT. Radiology. 2001;218(3):763–7.
Sultana S, Awai K, Nakayama Y, et al. Hypervascular hepatocellular carcinomas: bolus tracking with a 40-detector CT scanner to time arterial phase imaging. Radiology. 2007;243(1):140–7.
Bae KT. Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology. 2010;256(1):32–61.
Sakai S, Yabuuchi H, Chishaki A, et al. Effect of cardiac function on aortic peak time and peak enhancement during coronary CT angiography. Eur J Radiol. 2010;75(2):173–7.
Nijhof WH, Hilbink M, Jager GJ, Slump CH, Rutten MJ. A non-invasive cardiac output measurement as an alternative to the test bolus technique during CT angiography. Clin Radiol. 2016;71(9):940.e1-5.
Mehnert F, Pereira PL, Trübenbach J, Kopp AF, Claussen CD. Biphasic spiral CT of the liver: automatic bolus tracking or time delay? Eur Radiol. 2001;11(3):427–31.
Yamaguchi I, Hayashi H, Suzuki M, Ichikawa K, Kidoya E, Kimura H. Operation of bolus tracking system for prediction of aortic peak enhancement at multidetector row computed tomography: pharmacokinetic analysis and clinical study. Radiat Med. 2008;26(5):278–86.
Kanematsu M, Goshima S, Kondo H, et al. Optimizing scan delays of fixed-duration contrast injection in contrast-enhanced biphasic multidetector-row CT for the liver and the detection of hypervascular hepatocellular carcinoma. J Comput Assist Tomogr. 2005;29(2):195–201.
Goshima S, Kanematsu M, Kondo H, et al. MDCT of the liver and hypervascular hepatocellular carcinomas: optimizing scan delays for bolus-tracking techniques of hepatic arterial and portal venous phases. AJR Am J Roentgenol. 2006;187(1):W25-32.
Yamaguchi I, Kidoya E, Suzuki M, Kimura H. Optimizing scan timing of hepatic arterial phase by physiologic pharmacokinetic analysis in bolus-tracking technique by multi-detector row computed tomography. Radiol Phys Technol. 2011;4(1):43–52.
Kagawa Y, Okada M, Yagyu Y, et al. Optimal scan timing of hepatic arterial-phase imaging of hypervascular hepatocellular carcinoma determined by multiphasic fast CT imaging technique. Acta Radiol. 2013;54(8):843–50.
Noda Y, Kawai N, Ishihara T, et al. Optimized scan delay for late hepatic arterial or pancreatic parenchymal phase in dynamic contrast-enhanced computed tomography with bolus-tracking method. Br J Radiol. 2021;94(1122):20210315.
Yu J, Lin S, Lu H, et al. Optimize scan timing in abdominal multiphase CT: bolus tracking with an individualized post-trigger delay. Eur J Radiol. 2022;148:110139.
Schwinger RHG. Pathophysiology of heart failure. Cardiovasc Diagn Ther. 2021;11(1):263–76.
Zhu Y, Xu H, Zhu X, et al. Association between cardiothoracic ratio, left ventricular size and systolic function in patients undergoing computed tomography coronary angiography. Exp Ther Med. 2014;8(6):1757–63.
Johnson PT, Scott WW, Gayler BW, Lewin JS, Fishman EK. The CT scout view: does it need to be routinely reviewed as part of the CT interpretation? AJR Am J Roentgenol. 2014;202(6):1256–63.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transpl. 2013;48(3):452–8.
Chaturvedi A, Oppenheimer D, Rajiah P, Kaproth-Joslin KA, Chaturvedi A. Contrast opacification on thoracic CT angiography: challenges and solutions. Insights Imaging. 2017;8(1):127–40.
Muroga K, Minochi Y, Fukuzawa A. Improvement in arterial enhancement using diluted injection of contrast medium in CT angiography. Acta Radiol. 2023;64(2):489–95.
Tomita H, Yamashiro T, Matsuoka S, Matsushita S, Kurihara Y, Nakajima Y. Changes in cross-sectional area and transverse diameter of the heart on inspiratory and expiratory chest CT: correlation with changes in lung size and influence on cardiothoracic ratio measurement. PLoS ONE. 2015;10(7):e0131902.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This retrospective study was approved by the ethics committee of our hospital (No. R-080) and the requirement for patient informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Muroga, K., Kitahara, K. Adjustment of scan delay for bolus tracking with cardiothoracic ratio of CT scout image for hepatic artery phase of hepatic dynamic CT. Radiol Phys Technol 17, 651–657 (2024). https://doi.org/10.1007/s12194-024-00814-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-024-00814-w