Abstract
Computed tomography (CT) examinations have been increasingly requested and become the major sources of patient exposure. The cancer risk from CT scans is contingent upon the amount of absorbed dose of organs. This study aims to determine the organ doses and risk of cancer incidence and mortality from CT examinations at high dose (cumulative effective dose, CED ≥ 100 mSv) in a single day to low dose (CED < 100 mSv) from common CT procedures. Data were gathered from two academic centers of patients aged 15 to 75 years old performed CT examinations during the period of 5 years. CED and organ dose were calculated using Monte Carlo simulation software. Lifetime attributable risk (LAR) was determined following Biological Effects of Ionizing Radiation (BEIR) VII report based on life table and baseline cancer rates of Thai population. At high dose, the highest LAR for breast cancer incidence in young female was 82 per 100,000 exposed patients with breast dose of 148 mGy (CT whole abdomen). The highest LAR for liver cancer incidence in male patient was 72 per 100,000 with liver dose of 133 mGy (multiple CT scans). At low dose, the highest average LAR for breast cancer incidence in young female was 23 per 100,000 while for liver cancer incidence in male patients was 22 per 100,000 (CTA whole aorta). Even though the LAR of cancer incidence and mortality was less than 100 per 100,000, they should not be neglected. The risk of cancer incidence may be increased in later life, particularly in young patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The man-made source of ionizing radiation continues to be the most common application of radiation in medicine, especially in diagnostic imaging modalities, including radiography, fluoroscopy, computed tomography (CT), mammography, and interventional radiology [1,2,3]. The United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) 2020/2021 [4] reported the distribution of examinations and radiation dose by medical imaging modality worldwide. From 2009 to 2018, the part of CT had been contributed 9.6 percent of all modalities, and the collective effective dose was 61.6 percent. National Council on Radiation Protection and Measurements (NCRP) publication 184 [5] reported the trend of CT examinations in the US increased by 20 percent per year. CT examinations had consistently increased since 1993 from 18.3 million, reaching a peak of 85.3 million in 2011 and then stabilizing, slightly decreased to 73.8 million procedures in 2017. The evolution of CT systems provide good quality imaging, fast gantry rotation time, high temporal resolution, and become an essential examination for diagnosis and follow-up of the diseases [6,7,8]. The significant impact of the expansion of imaging procedures, the number of examinations, and the frequency of repeated imaging led to a high cumulative effective dose and increased cancer risk [9,10,11]. The risk of radiation-induced cancer is dependent on the age at exposure, gender, the type of examinations, as well as the organs absorbed dose [12,13,14].
Biological effects of ionizing radiation (BEIR) VII Phase 2 [1] developed the risk model based on the primary source of epidemiological data from the Japanese atomic bomb survivors to estimate lifetime cancer incidence and mortality risks from exposure to low linear energy transfer (LET) radiation. Cancer risks were determined based on either excess relative risk model (ERR) or excess absolute risk model (EAR) adjusted for age at exposure, attained age, and gender. The risk models were applied to leukemia and solid cancer, according to the cancer sites as a function of organ dose in a unit of mGy. Furthermore, the linear no threshold model (LNT) was established as the association between low dose exposure and the risk of cancer occurring linearly without thresholds. This indicates that even the small amount of radiation could increase the risk of cancer in the later life [1, 2, 15, 16].
The cancer risk assessment of solid cancer incidence and mortality for low LET radiation was derived from the study of acute exposure at high dose and dose rates, then extrapolated to lower dose and dose rates. Consequently, the risk model embedded within the correction factor, the dose and dose-rate effectiveness factor (DDREF). DDREF represents the ratio between risks at high-dose or high-dose rates and low-dose or low-dose rates, BEIR VII report proposed a DDREF of 1.5 [1, 17, 18].
BEIR VII report classified low dose range from close to zero to 100 mSv, and the high dose from more than 100 mSv. Several publications reported that the risk of cancer from ionizing radiation is dependent on the amount of radiation dose [1, 2, 19, 20]. At low dose, radiation risk is associated with stochastic effect or cancer induction based on epidemiological data from Japanese atomic bomb survivors. The Radiation Effects Research Foundation (RERF) in Japan reported solid cancer has been found in 60 percent of survivors receiving radiation dose less than 100 mSv. In addition, the risk of cancer incidence increased linearly in high dose range when the effective dose exceeded 100 mSv [1, 18,19,20,21]. The cumulative effective dose (CED) of 100 mSv and above become more evidence, particularly from the CT scans of the chest, whole abdomen, and pelvis [15, 22,23,24]. Therefore, the radiation exposure delivered to patients by CT should be emphasized and concerned with long-term risk [25,26,27]. Although a single procedure typically offers a low dose, there is a concern that pediatric and young patients may obtain repeated CT exams over time [1, 28,29,30].
Many publications showed the risk of cancer from various CT protocols, such as abdomen, chest, head, and heart, were estimated by linear interpolation method as described in BEIR VII table 12D-1,2 [15, 24, 31]. Lim H et al. [32] determined the risk of cancer incidence and mortality from medical radiation imaging using Korean background cancer incidence and mortality. Harbron RW et al. [27] reported cancer risks attributable to radiation exposure from cardiac catheterizations based on UK background cancer rates. A few studies reported LAR applied to the population based on life table and baseline cancer rate receiving high to low radiation dose [3, 27, 32, 33]. Therefore, this study aims to determine the organ absorbed dose and risk of cancer incidence and mortality from CT examinations at high dose (CED ≥ 100 mSv) in a single day to low dose (CED < 100 mSv) from the common CT procedures. The study utilizes the BEIR VII model and abridged life table data as well as baseline cancer incidence and mortality rates for the Thai population.
2 Materials and methods
2.1 Data population and radiation dose determination
The retrospective study was approved by the Institutional Review Boards (IRB) from two academic centers. The data were collected from the adult patients aged 15 to 75 years old who underwent CT examinations for a period of five years from January 2018 to December 2022. The patient data was divided into two age group: below 40 years old–called young patients, and above 40 years old–called elder patients. The patient data and patient dose were collected from digital imaging and communications in medicine (DICOM) header and commercial software, Radimetrics™ Enterprise Platform (Bayer HealthCare, Whippany, NJ, USA). Modern CT equipment: model Aquilion Prime 80 detector rows (Canon Medical Systems, Otawara, Japan), model Brilliance iCT 256 Slice (Philips Healthcare, Cleveland, OH, USA), model Revolution Apex 256 detector rows, Revolution 256 detector rows (GE Healthcare, Milwaukee, WI, USA) and model SOMATOM Force dual-source 192 detector rows (Siemens Healthineers, Forchheim, Germany) had been used to acquire and process the medical imaging in this study.
Radimetrics™ Enterprise Platform provides several measures of radiation dose from CT scan, encompassing organ dose and effective dose estimations obtained using Monte Carlo simulations. The patients are represented as stylized phantoms, where the organs are modeled using simple geometric shapes described by mathematical equations. The organ dose is calculated from the ratio of the simulated organ dose to the simulated CTDIvol multiplied by the reported CTDIvol [34].
The verification of the accuracy of the volume computed tomography dose index (CTDIvol) displayed on the CT scanner monitor was conducted using two cylindrical phantoms made of polymethyl methacrylate (PMMA) of 16 and 32 cm in diameter with 15 cm length. A pencil ionization chamber (IC) with a sensitive length of 100 mm was utilized for CT dosimetry. The measured CTDIvol was obtained by axial scanning of each cylindrical phantom with IC insertions at various kVp values from 80 to 140. The measured and the displayed CTDIvol were compared with the acceptable limit at ± 20%.
The radiation-induced risk of cancer incidence and mortality in high dose range were evaluated from the patients who received the CED at 100 mSv and above in a single day. To estimate the cancer risk from the low dose range, CED below 100 mSv, from common CT procedures of brain without and with contrast enhanced phase, chest with contrast-enhanced phase, whole abdomen with triphasic phased including without contrast enhanced, arterial and portal phase, and angiography of whole aorta, without contrast, arterial and delayed phase had been acquired. The protocols were designed by the radiologists based on the patient clinical indications. The patient effective dose (mSv) and the organ dose (mGy) calculated from Monte Carlo (Radimetrics™ Enterprise Platform) simulated the organs of lungs, liver, colon, breast, uterus, and brain had been used to estimate the risk of cancer.
2.2 Lifetime attributable risk (LAR) estimation
LAR was determined according to the BEIR VII report [1] which provided model and parameters for specific organs of each gender including parameters of age at exposure, attained age, organ dose and dose and dose rate effectiveness factor (DDREF). LAR of cancer incidence and mortality in each patient, including the organ doses of lung, liver, colon, uterus, breast, and brain were estimated using Eq. (1).
LAR is defined as the summation from a equals e + L to amax, where a is attained age (years), amax is maximum age (80 years), L is a risk-free latent period (5 years for solid cancers), e is the age at exposure (15 to 75 years), D is an organ dose, and S(a)/S(e) is the conditional probability of a person alive and cancer-free at age-at exposure, e, to reach at least an attained age- a, obtained from abridged life table provided by National statistical office of Thailand [35]. M (D, e, a) is the excessive cancer risk model, which can be calculated using relative risk transport and absolute risk transport based on the excess relative risk (ERR) model and the excess absolute risk (EAR) model from Eq. (2) to (5).
Excess for cancer incidence risk:
Excess for cancer mortality risk:
where EAR and ERR are models from BEIR VII, λI(a) represents sex and age specific of baseline cancer incidence rates, whereas the λM(a) represents sex and age specific cancer mortality rates obtained from cancer statistics Thailand for the year 2020, published by the World Health Organization (WHO), International Agency for Research on Cancer [36].
According to the models established based on the data of Japanese atomic bomb survivors, which the baseline cancer rates differ from other populations. In this case, the application of risk estimates to a U.S. population was considered. The BEIR VII committee [1] provides estimates for various cancer sites, employing two assumptions; relative risk transport, the excess relative risk, ERR is proportional to baseline risks, and absolute risk transport assumed that the excess absolute risk, EAR is unrelated to the baseline risks. The weighted estimates had been proposed, taking into account the uncertainty of transporting risks.
For the estimation of LAR, the risk-transfer weight or weighting factor was obtained with EAR and ERR transport models for the site of solid cancers (liver, colon, uterus, and brain), BEIR VII recommended a weighting factor(ω) of 0.7. The weighting factor(ω) of 0.7 was estimated using ERR transport and 0.3 to estimate using EAR transport. For lung cancer, the weighting factor was reversed, 0.7 for the EAR transport and 0.3 for the ERR transport. The LAR of breast cancer was estimated based on the EAR model.
For the LAR estimation, the ERR and EAR models were combined via the weighting factor(ω) as expressed in Eq. (6), and subsequently adjusted by dividing DDREF of 1.5, as suggested by the BEIR VII report.
2.3 Statistical analysis
All statistical analyses of patient demographic data and patient dose were calculated by SPSS version 22 IBM, New York, USA. R Studio version 1.4.1103 has been used to calculate the cancer risk. LAR was compared between female and male patients using independent t-tests, with a statistical significance of p-value < 0.05 based on 2 tailed tests.
3 Results
3.1 Verification of the displayed CTDIvol
The CTDIvol displayed on the monitors of the five CT scanners was verified by comparing the displayed and measured CTDIvol. All of them were within ± 20%, which is the acceptable limit of the difference [37].
3.2 Data population
For a period of five years, 285,286 CT examinations had been collected by two academic centers in Thailand. The majority of CT examinations were CT chest (27.2 percent), whole abdomen (20.3 percent), brain (13.3 percent), and vascular (9.0 percent). The rest of the CT examinations were extremities, spine, cardiac, and neck, at 30.2 percent in total.
3.3 Radiation dose and LAR
The number of patients who underwent CT examinations and receiving high dose, CED 100 mSv and above in a single day was 27, accounting for 0.009 percent of total 285,286 CT examinations. 7 of 27 were young patients with the age below 40 years old, and 20 of 27 were elder patients, with the age above 40 years old. The acquisition protocols for patients following the multiple CT scans in 6 cases (22.2 percent) include 1 case of CT C-spine, whole abdomen, CTA neck and CTA chest, 1 case of brain, neck and whole abdomen, 1 case of brain, C-spine, and whole abdomen, 1 case of brain, C-Spine, CTA run off of upper extremity, 1 case of shoulder, chest and whole abdomen, and 1 case of CTA run off of lower extremity, chest and whole abdomen, 6 cases (22.2 percent) of whole abdomen, 3 cases (11.1 percent) of chest and whole abdomen, and 3 cases (11.1 percent) of angiography of the thoracic aorta were included. The rest consisted of 9 cases (33.3 percent) of single procedure.
The common CT procedures including brain, chest, whole abdomen, and angiography of the whole aorta were classified by gender. The mean CED ± S.D. in young patients of CT brain in female (118 patients), male (25 patients) was 5.4 ± 0.6 and 6.0 ± 0.7 mSv, CT chest in female (180 patients), male (89 patients) was 9.9 ± 2.6 and 8.5 ± 2.2 mSv, CT whole abdomen in female (33 patients), male (30 patients) was 29.5 ± 9.8 and 22.9 ± 8.1 mSv and angiography of the whole aorta in female (21 patients), male (97 patients) was 37.9 ± 13.6 and 34.3 ± 10.2 mSv respectively.
Table 1 shows the demography of young patients (3 females, 4 males) receiving high dose with age range of 22–39 years old, comprising the age at exposure, gender, body weight, clinical indications, CT protocols, CED (mSv) and organ doses (mGy) included the lungs, liver, colon, breasts, uterus, and brain.
Among elder age group receiving high dose, the mean ± S.D. (range) organ dose of the 20 patients (12 females, 8 males) were: lung 152.7 ± 78.5(38.7–313.4) mGy, liver, 164.0 ± 38.6(120.7–246.4) mGy, colon, 105.4 ± 62.3(5.8–226.8) mGy, breast 147.9 ± 76.5(16.1–305.9) mGy, uterus, 79.8 ± 57.7(1.5–166.1) mGy, and brain, 19.9 ± 39.6(0.1–153.3) mGy. The mean CED ± S.D. (range) of elder age group was 115.7 ± 15.2(101.5–159.9) mSv.
Table 2 shows the average organ dose (mGy) in young patients as classified by gender, from common CT procedures including brain, chest, whole abdomen, and angiography of the whole aorta.
Table 3 illustrates LAR of cancer incidence and mortality from CT examinations to young patients in the high dose range provides LAR per 100,000 for cancer incidence and cancer mortality in 6 sites, along with 7 patients. The highest LAR for breast cancer incidence in young female was 82 in 100,000. The highest LAR for liver cancer incidence in male patient was 72 in 100,000.
Table 4 shows CT whole abdomen examinations performed with multiple-phase studies comprising of without contrast enhanced, arterial, portal, and delayed-phase scanning, had a significant contribution in patients receiving high dose, CED 100 mSv and above. The mean CED ± S.D. (range) of 6 patients was 114.5 ± 22.5(101.5–159.9) mSv while the organ dose of the lung was 74.3 ± 23.8(38.9–111.8) mGy, liver, 162.7 ± 38.1(140.5–239.5) mGy, colon, 156.9 ± 38.9(112.9–226.8) mGy, breast, 89.9 ± 67.3(16.1–147.6) mGy, uterus, 133.1 ± 32.4(101.3–166.1) mGy. The LAR of 6 subjects was influenced by the age of exposure, gender, body habitus and amount of absorbed dose of internal organs. LAR of lung, liver, colon, breast and uterus of incidence were marginally greater than mortality cancer.
Table 5 is presented in LAR for cancer incidence and mortality of male and female among young patients undergoing common CT procedures. A significant difference was observed in LAR for lung, liver, and colon cancer incidence and mortality between females and males from CT brain and angiography of the whole aorta (p < 0.05), except for LAR of brain cancer incidence and mortality. Whereas the LAR of all solid cancers from CT whole abdomen and chest was significantly different between females and males (p < 0.05).
Figure 1 illustrates the distribution of LAR for solid cancer incidence per 100,000 including lung, liver, colon, breast, and uterus from high CT dose categorized by gender across 27 patients (15 females, 12 males). The median LAR of lung in females and liver in males was higher than the other solid cancers.
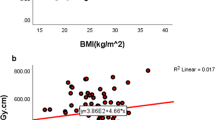
Figure 2 depicts the relationship between age at exposure and LAR of lung cancer incidence per 100,000 of patients conducted by common procedures of CT chest examinations (759 females, 448 males). The average lung dose for females and males was 18.1 ± 4.6 mGy and 18.9 ± 4.9 mGy, respectively. The mean ± S.D. of LAR for lung cancer incidence of young females and males from CT chest examinations was 5.0 ± 1.4 and 3.4 ± 1.0 per 100,000 respectively. LAR is greater in young patients, notably females with higher than males, and declined with the increasing age of exposure.
4 Discussion
In this study, the radiation induced patient cancer risk from CT examinations at high dose (≥ 100 mSv) in a single day to low dose (< 100 mSv) in the common procedures had been estimated in terms of LAR. The ERR and EAR models had been calculated and adjusted by DDREF in females and males of different cancer sites including lungs, liver, colon, breast, uterus and brain based on abridged life table and baseline incidence and mortality cancer rates of the Thai population.
Even though the percentage of patients received CED 100 mSv and above in a single day per all CT examinations, 27 from total 285,286 CT examinations, was 0.009, the highest distribution was among the young patients. 37 percent (10 patients) was less than 50 years old; 33 percent (9 patients) was 51–65 years old, and 30 percent (8 patients) was over 65 years old. Brambilla M et al. [38] reported different patterns with the highest distribution of greater than 65 years old of 229 patients (64 percent) with observation period in a month. Rehani MM et al.[10] reported high dose, 100–200 mSv frequently encountered in older age groups at greater than 60 years old. While Zewde N. et al. [15] showed a large distribution of patients receiving CED above 100 mSv were between 55 and 84 years old.
LAR was estimated by considering the frequent cancer sites, comprising liver, lung, breast, colorectum, and cervix uteri in Thai population [39]. The estimation of LAR of the organs situated outside the CT scan region based on the scattered radiation, were very low and negligible. The average LAR of brain cancer incidence and mortality were approximately 0.004 per 100,000 for female and 0.001 per 100,000 for male from the CT whole abdomen as shown in Table 5. Bosch de Basea M. et al.[3] conducted an estimation of the organ dose and LAR for organs in the scanning regions such as the stomach, colon and rectum, pancreas, liver, and kidneys from CT abdomen. Meanwhile, Khan NA et al. [24] determined the organ dose and LAR in organs exposed to scattered radiation. Our study estimated the organ dose and LAR not only within the scan area, but also in the periphery, for example from CT abdomen, 6 patients receiving high dose, CED ≥ 100 mSv, the average organ dose of the lung was 74.3 ± 23.8 (38.9–111.8) mGy while female breast was 89.9 ± 67.3(16.1–147.6) mGy. The highest LAR for breast and lung cancer incidence were 82 and 38 per 100,000, respectively as shown in Table 4. The significant factor was the scan irradiated length extended to the lower of thorax region. Consequently, it is essential to minimize the unnecessary radiation exposure with improper scan regions.
In this study, the commercial software had been used to determine the organ dose modeled utilizing the stylized computational phantoms and represented by mathematical equations for estimating LAR. While Maxwell S et al. [40] used the software based on voxelized phantoms provided organ dose to determine cancer incidence. Thus, the software type and size of the phantom may affect the value of the organ dose employed to determine cancer risk.
According to epidemiological data from the Life Span Study (LSS) cohort, radiation-induced breast cancer rates were high, especially in young adult [18]. In our study, at the high dose, the LAR for breast cancer incidence in young female patients who underwent CT whole abdomen was 82 in 100,000 (Table 3). At the low dose, the average LAR for breasts cancer incidence of patients performed CT angiography of the whole aorta was 23 in 100,000 (Table 5). In the Fig. 2, LAR of lung cancer incidence in younger females was higher than males and decreased with increasing exposure age. The average lung dose was slightly different for females, 18.1 ± 4.6 mGy and males, 18.9 ± 4.9 mGy whereas the parameter of ERR and EAR model derived from BEIR VII report of females was greater than males. The mean ± S.D. of LAR for lung cancer incidence of young females and males from CT chest examinations was 5.0 ± 1.4 and 3.4 ± 1.0 per 100,000 respectively. Although the amount of LAR per 100,000 is relatively low, it is necessary to consider the potential cancer risk resulting from radiation. Specifically, in young adults who may receive recurrent CT scans from follow-up or diagnose their diseases, the risk of cancer may increase significantly.
It is interesting to compare the LAR from this study to others. The LAR for lung cancer incidence was 5.1 per 100,000 and the median organ dose of the lung was 16.9 mGy of Thai subjects, while the LAR for lung cancer of Spanish subjects [3] at the same age range was 96.84 per 100,000 and the median organ dose of the lungs was 15.5 mGy. The discrepancy among both LARs was according to the maximum age at 80 years in Thai subjects and 110 years in Spanish subjects. Bosch de Basea M. et al. [3] determined the lifetime cancer risk for young patients from CT scans, providing useful data to promote radiation protection, particularly in the young cohorts. It is beneficial to categorize the levels of cancer risk associated with radiation exposure according to the procedures, age group, and gender in order to justify the health risks, benefits and optimized parameter settings.
There are two limitations in this study. First, the BEIR VII method is implemented to estimate the risk of cancer based on the linear dose-risk relationship. The risk coefficients and risk-transfer weights were adopted to calculate LAR for each cancer site, while these factors were obtained from the cohort of Japanese and U.S. populations. Consequently, the uncertainty of this issue should be considered and mentioned. Second, LAR has been calculated using the maximum age of 80 years in this study, based on the average typical life expectancy for both genders of Thai subjects [39]. Due to Thailand's demographic life table, the probability of surviving longer than 80 years in Thai population is limited.
5 Conclusion
Recurrent CT scans and CT whole abdomen contribute high radiation dose to the patients. LAR for breast cancer incidence of young female underwent CT whole abdomen was 82 in 100,000 with breast dose of 148 mGy. LAR for liver cancer in male patients underwent multiple CT scans was 72 in 100,000 with a liver dose of 133 mGy. Both LARs were higher than other cancer sites. LAR for lung cancer incidence from CT chest examinations was 5.0 and 3.4 per 100,000 in young female and male, respectively and declined with the increasing age of exposure. The range of LAR for cancer incidence and mortality in the common CT procedures of brain, whole abdomen, and angiography of whole aorta in young adult patients were 0.0003–13.2, 0.001–18.2, and 0.7–23.2 per 100,000, respectively. Therefore, the cumulative effective dose (CED) from CT examinations at 100 mSv and above should be monitored and recorded individually to reduce the incidence and mortality risk of cancer at later life, particularly in young adult patients.
References
National Research Council. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2. Washington, DC: National Academy of Sciences; 2006.
International Commission on Radiological Protection. The 2007 recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37:1–332.
Bosch de Basea M, Morina D, Figuerola J, Barber I, Muchart J, Lee C, et al. Subtle excess in lifetime cancer risk related to CT scanning in Spanish young people. Environ Int. 2018;120:1–10.
United Nations Scientific Committee on the Effects of Atomic Radiation. Sources, effects, and risks of ionizing radiation. Evaluation of medical exposure to ionizing radiation. Vol 1, Scientific Annex A. 2020/2021 Report to the General Assembly with annexes. New York: United Nations; 2022.
National Council on Radiation Protection and Measurements. Medical radiation exposure of patients in the United States. NCRP Report No.184. Bethesda, Md: National Council on Radiation Protection and Measurements; 2019.
Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–84.
Nuntue C, Krisanachinda A, Khamwan K. Optimization of a low-dose 320-slice multi-detector computed tomography chest protocol using a phantom. Asian Biomedicine. 2016;10:269–76.
Tongkum S, Suwanpradit P, Vidhyarkorn S, Siripongsakun S, Oonsiri S, Rakvongthai Y, et al. Determination of radiation dose and low-dose protocol for digital chest tomosynthesis using radiophotoluminescent (RPL) glass dosimeters. Phys Med. 2020;73:13–21.
Kwee TC, Dijkstra H, Knapen DG, de Vries EGE, Yakar D. Which patients are prone to undergo disproportionate recurrent CT imaging and should we worry? Eur J Radiol. 2020. https://doi.org/10.1016/j.ejrad.2020.108898.
Rehani MM, Heil J, Baliyan V. Multicentric study of patients receiving 50 or 100 mSv in a single day through CT imaging-frequency determination and imaging protocols involved. Eur Radiol. 2021. https://doi.org/10.1007/s00330-021-07734-y.
Tamam N, Sulieman A, Omer H, Toufig H, Alsaadi M, Salah H, et al. Assessment of breast dose and cancer risk for young females during CT chest and abdomen examinations. Appl Radiat Isot. 2022. https://doi.org/10.1016/j.apradiso.2022.110452.
Wall B, Haylock R, Jansen J, Hillier M, Hart D, Shrimpton P. Radiation risks from medical x-ray examinations as a function of the age and sex of the patient. Report HPA-CRCE-028. Chilton: Health Protection Agency; 2011.
Mahmoodi M, Chaparian A. Organ doses, effective dose, and cancer risk from coronary CT angiography examinations. AJR Am J Roentgenol. 2020;214:1131–6.
Karimizarchi H, Chaparian A. Estimating risk of exposure induced cancer death in patients undergoing computed tomography pulmonary angiography. Radioprotection. 2017. https://doi.org/10.1051/radiopro/2016087.
Zewde N, Ria F, Rehani MM. Organ doses and cancer risk assessment in patients exposed to high doses from recurrent CT exams. Eur J Radiol. 2022. https://doi.org/10.1016/j.ejrad.2022.110224.
Lee S, Kim J, Han S. A comparative review of radiation-induced cancer risk models. J Radiat Prot Res. 2017;42:130–40.
EPA. Radiogenic cancer risk models and projections for the U.S. population. Report EPA 402-R-11–001. Washington, DC: U.S. Environmental Protection Agency; 2011.
World Health Organization. Health risk assessment from the nuclear accident after the 2011 Great East Japan earthquake and tsunami, based on a preliminary dose estimation. Geneva: WHO; 2013.
Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA. 2003. https://doi.org/10.1073/pnas.2235592100.
Hendee WR, O’Connor MK. Radiation risks of medical imaging: separating fact from fantasy. Radiology. 2012;264:312–21.
de Souza Ribeiro JC, de Mendes JDS, de Sá LV. Attributable patient risk in nuclear medicine procedures and establishment of diagnostic reference levels. J Appl Clin Med Phys. 2023. https://doi.org/10.1002/acm2.13658.
Suksancharoen W, Lowong T, Krisanachinda A. Assessment of patient radiation dose from recurrent ct examinations. Medical Physics International. 2021;9:93–6.
Brower C, Rehani MM. Radiation risk issues in recurrent imaging. Br J Radiol. 2021. https://doi.org/10.1259/bjr.20210389.
Khan AN, Khosa F, Nikolic B, Shuaib W, Lin PJ, Khan MK. Cancerogenesis risks between 64 and 320 row detector CT for coronary CTA screening. J Clin Imaging Sci. 2014. https://doi.org/10.4103/2156-7514.131640.
Dance DR, Christofides S, Maidment ADA, McLean ID, Ng KH. Diagnostic radiology physics: a handbook for teachers and students. Vienna: International Atomic Energy Agency; 2014.
Bushberg JT, Seibert JA, Leidholt EM Jr, Boone JM. The essential physics of medical imaging. 4th ed. Philadelphia: Lippincott William and Wilkins; 2020.
Harbron RW, Chapple CL, O'Sullivan JJ, Best KE, Berrington de González A, Pearce MS. Survival adjusted cancer risks attributable to radiation exposure from cardiac catheterisations in children. Heart. 2017;103:341–6.
Majer M, Knežević Z, Saveta M. Current trends in estimating risk of cancer from exposure to low doses of ionising radiation. Arh Hig Rada Toksikol. 2014;65:251–7.
Kiani M, Chaparian A. Evaluation of image quality, organ doses, effective dose, and cancer risk from pediatric brain CT scans. Eur J Radiol. 2023. https://doi.org/10.1016/j.ejrad.2022.110657.
Kiani M, Bagheri J, Chaparian A. Evaluation of image quality, organ dose, effective dose and cancer risk in pediatric chest CT procedure. Journal of Isfahan Medical School. 2023;40:1029–36.
Adeleye B, Chetty N. Radiation dose and cancer risk estimates in helical CT for pulmonary tuberculosis infections. Open Physics. 2017;15:769–76.
Lim H, Choi J, Kim JH, Cheong HK, Ha M. Estimation of cancer incidence and mortality risks attributed to diagnostic medical radiation exposure in Korea, 2013. J Korean Med Sci. 2018. https://doi.org/10.3346/jkms.2018.33.e211.
Huang B, Li J, Law MW, Zhang J, Shen Y, Khong PL. Radiation dose and cancer risk in retrospectively and prospectively ECG-gated coronary angiography using 64-slice multidetector CT. Br J Radiol. 2010;83:152–8.
Bayer HealthCare Medical Care. CT organ dose calculations in Radimetrics™ Enterprise Platform by Bayer. Indianola: Bayer Pharma AG; 2016.
National Statistical Office Thailand. Abridged life table for population in Thailand, 2005–2006. 2006. http://www.nso.go.th. Accessed 30 March 2022
World Health Organization (WHO). Global Cancer Observatory: Cancer Today, Thailand: International Agency for Research on Cancer. 2020. https://gco.iarc.fr/today. Accessed 1 April 2022
International Atomic Energy Agency. Quality assurance programme for computed tomography: diagnostic and therapy applications. IAEA Human Health Series No.19. Vienna: IAEA; 2012
Brambilla M, Cannillo B, D’Alessio A, Matheoud R, Agliata MF, Carriero A. Patients undergoing multiphase CT scans and receiving a cumulative effective dose of ≥ 100 mSv in a single episode of care. Eur Radiol. 2021;31:4452–8.
World Health Organization (WHO). Global Cancer Observatory: Globocan 2020 Thailand. Summary statistic 2020. https://gco.iarc.fr/today/data/factsheets/populations/764-thailand-fact-sheets.pdf. Accessed 1 April 2022
Maxwell S, Fox R, McRobbie D, Bulsara M, Doust J, O’Leary P, et al. How have advances in CT dosimetry software impacted estimates of CT radiation dose and cancer incidence? A comparison of CT dosimetry software: Implications for past and future research. PLoS ONE. 2019. https://doi.org/10.1371/journal.pone.0217816.
Acknowledgements
The authors would like to thank Miss Jirawan Jayuphan, Department of Epidemiology, Faculty of Medicine, Prince of Songkla University, Thailand for her guidance and contribution to the statistical analysis.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Retrospective ethics approval
This research involves the determination of patient dose in Computed Tomography. The patient data had been collected during the period of 5 years from January 2018 to December 2022 in adult patients who underwent CT examinations. The research was approved by the Ethical Committee of the Faculty of Medicine, Chulalongkorn University, and Faculty of Medicine, Prince of Songkla University, Thailand.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Poosiri, S., Krisanachinda, A. & Khamwan, K. Evaluation of patient radiation dose and risk of cancer from CT examinations. Radiol Phys Technol 17, 176–185 (2024). https://doi.org/10.1007/s12194-023-00763-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-023-00763-w