Abstract
We evaluated the possibility of treatment-free remission (TFR) and durability of deep molecular response (DMR) with asciminib treatment by monitoring major BCR::ABL mRNA on the International Scale (BCR::ABL-IS) in 4 patients who needed to reduce or discontinue asciminib due to adverse event concerns, intolerance, or personal circumstances. IS increased in all 4 patients after discontinuation of asciminib, but 3 patients who resumed asciminib achieved DMR again. None of the patients achieved TFR with asciminib, but DMR could be achieved again by restarting asciminib after TFR failure. As this was a retrospective study in a small number of patients, no conclusions can be drawn regarding the possibility of TFR with asciminib. However, this study included patients with short treatment duration and DMR maintenance periods, so strict conditioning may be necessary. Safe dose reduction or TFR with asciminib may need to be considered in more cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tyrosine kinase inhibitors (TKIs) have made it possible to achieve a deep molecular response (DMR) in many patients with chronic myeloid leukemia (CML). As a result, the goal of current therapy for CML is to achieve treatment-free remission (TFR).
Although the efficacy and safety of asciminib, a STAMP inhibitor that specifically targets the myristoyl pocket of the ABL, are well known and the drug is used clinically to treat CML in chronic phase (CML-CP) patients refractory/intolerant to two or more TKIs, the possibility of achieving TFR with asciminib has not been investigated.
Here, we report the results of a follow-up study of major BCR::ABL mRNA on the International Scale (BCR::ABL-IS) in 4 patients who discontinued asciminib due to adverse event concerns, intolerance, or social issues. In this case report, we define DMR as MR4.
Case
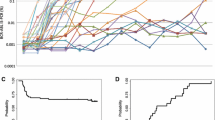
Case 1 A 71-year-old man with multiple bone metastases of prostate cancer. He was started on bosutinib but became refractory to treatment (best response BCR::ABL-IS 10.4022, molecular response (MR) not reached). Dasatinib was introduced as second-line therapy, and the patient achieved DMR (MR 4), but as he was intolerant due to anemia and rash, asciminib (20 mg/day) was introduced as third-line therapy. The patient achieved MR 4.5 during treatment with asciminib. However, he developed premature ventricular contractions during asciminib treatment and was also being treated for underlying chronic heart failure and hypertension, so the decision was made to pursue TFR due to concerns over the risk of cardiovascular disease associated with long-term TKI treatment, although he did not meet the criteria for TFR as defined by the guidelines. The total duration of TKI treatment was 2 years 2 months, and the duration of the DMR was 1 year. After 7 months, treatment with asciminib was discontinued. One month after discontinuation of asciminib, his IS increased and major molecular response (MMR) loss was observed. When asciminib was restarted, IS showed a decreasing trend, and MR 4 was achieved again.
Case 2 A 64-year-old man treated with imatinib 400 mg for CML-CP since December 2004. The patient ceased visiting the hospital in May 2012, but he visited again in June 2017 and was diagnosed with relapse and started treatment with dasatinib 100 mg. In October 2017, for financial reasons, he preferred to be treated with imatinib 400 mg, so the treatment regimen was changed. However, he did not respond to treatment (best response BCR::ABL-IS 29.2194, MR not reached) and was referred to our hospital in April 2018 and introduced to asciminib 80 mg/day a third-line treatment. The best response with asciminib was MR 5. But after 5 years of asciminb treatment, he wanted to treatment cessation for financial reasons. The total duration of TKI therapy was 6 years, and the duration of DMR was 2 years and 8 months. After stopping asciminib, IS increased and MMR loss occurred within 4 months. Thereafter, the patient self-interrupted his hospital visits, and follow-up was terminated.
Case 3 A 75-year-old man undergoing treatment for esophageal cancer, prostate cancer, and hypopharyngeal cancer was started on dasatinib. MR 4 was achieved, but continued treatment was difficult due to pleural effusion. The patient was deemed intolerant, and nilotinib was introduced. He was able to obtain a therapeutic effect of MR 5, but even with dose reduction, he was intolerant due to the appearance of liver damage and dyspnea sensation. Bosutinib was then introduced, and a therapeutic effect of MR 5 was achieved. During bosutinib therapy, the patient developed chronic heart failure due to mitral regurgitation and underwent surgery. Bosutinib was continued for a time but eventually discontinued due to elevating amylase; IS gradually increased and MMR loss also occurred. Asciminib 20 mg/day was introduced as fourth-line therapy. During the course of the disease, the patient developed lung cancer and underwent surgery. Postoperative complications included intrapulmonary hemorrhage, pneumonia, gastrointestinal bleeding, and worsening heart failure, which required prolonged intensive care management, and the patient was off treatment 4 months after starting asciminib. The best response to asciminib was MR 4.5; the total duration of TKI therapy was 6 years and 3 months, and the duration of DMR was 2 years. After stopping asciminib, the IS tended to increase, and MMR loss occurred within 2 months. When asciminib was resumed, IS showed a decreasing trend, and MR 5 was achieved again.
Case 4 A 34-year-old man treated with imatinib 400 mg for CML-CP. He showed resistance to imatinib and was referred to our hospital. Dasatinib was introduced, and after achieving MR 5 with 100 mg dasatinib and maintaining DMR for 3 years, the dose was reduced to 70 mg. The dose was tapered from 50 to 20 mg because DMR was maintained. But when the dose was reduced to 20 mg, the IS showed an increasing trend and DMR loss occurred, so the dose was increased to 50 mg again. Tapering was attempted, but when the dose was reduced to 20 mg, the IS tended to increase. Because he could not achieve TFR, had been on TKIs for 14 years, and was concerned about cardiovascular disease despite his young age, he was started on asciminib as third-line therapy. He achieved MR 5 with asciminib. Total duration of TKI treatment was 14 years and 8 months, and DMR was 5 years and 10 months. After stopping asciminib, the IS tended to increase, and MMR loss occurred 2 months after discontinuation of asciminib. When asciminib was resumed, IS showed a decreasing trend, and MR 4.5 was achieved again.
Discussion
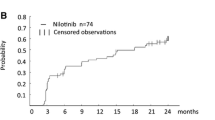
Approximately one-half of patients diagnosed with CML-CP and whose DMR is maintained for a certain period of time with first-line imatinib, nilotinib, or dasatinib are reportedly able to maintain TFR without molecular genetic relapse after discontinuation of the TKI [1]. Additionally, approximately one-half of patients who were resistant or intolerant to the previous TKI but maintained DMR for a certain period of time with second-line nilotinib or dasatinib are reportedly able to maintain TFR after discontinuation of the TKI [2, 3].
Although the efficacy and safety of asciminib, a STAMP inhibitor that specifically targets the myristoyl pocket of the ABL, are well known and the drug is used clinically to treat CML-CP patients refractory/intolerant to two or more TKIs [4], the possibility of achieving TFR with asciminib has not been investigated.
We followed the evolution of IS in 4 patients who required dose reduction or discontinuation of asciminib due to adverse event concerns, intolerance, or social issues. To the best of our knowledge, this is the first report to examine the possibility of TFR with asciminib alone. In all 4 cases, the best response to prior therapy was DMR, and the total duration of TKI treatment was more than 2 years (2 years 2 months to 14 years 8 months) (Table 1). In all 4 patients, DMR could be maintained even at reduced doses of asciminib. All 4 patients also showed a rapid increase in IS immediately after discontinuation of asciminib. Three of four patients showed a rapid decline in IS after resumption of asciminib and achieved DMR again. One of four patients ceased visiting the hospital and was lost to follow-up; therefore, follow-up was terminated.
The results of this study indicate that asciminib may be used at reduced doses to induce and maintain DMR. Dose adjustment may be necessary, depending on the patient's underlying disease and frailty. Although induction of TFR with asciminib is thought to be difficult, it is possible to achieve DMR again with the resumption of asciminib, and considering the high safety profile of asciminib as shown in the ASCEMBLE study, it is possible that patients who receive asciminib for CML-CP that is resistant/intolerant to ≥ 2 TKIs may be able to achieve DMR with asciminib. The results of our study suggest that it may be desirable to continue asciminib, even at low doses, in patients who have been introduced to asciminib for CML-CP resistant/intolerant to ≥ 2 TKIs.
This was a retrospective study of a small number of patients, and there were cases of short DMR duration leading to asciminib discontinuation. The short DMR duration may have been a disadvantage for discontinuation of asciminib. In addition, previous studies have shown that the TFR rate is low in patients whose TKI was changed due to previous TKI resistance [5], and 4 of the 4 patients in this study were resistant to the previous TKI. This may have also worked against asciminib discontinuation.
So far, it is difficult to define the potential and mechamisms of asciminib treatment on the TFR. Safe dose reduction or withdrawal of asciminib needs to be studied in a larger number of patients in the appropriate clinical study.
New findings
The results of this study indicate that induction of treatment-free remission (TFR) with asciminib is thought to be difficult. Considering the high safety profile of asciminib, it is possible that patients who receive asciminib for CML in the chronic phase (CML-CP) that is resistant/intolerant to ≥ 2 Tyrosine kinase inhibitors (TKIs) may be able to achieve deep molecular response (DMR) with asciminib. The results of our study suggest that it may be desirable to continue asciminib, even at low doses, in patients who have been introduced to asciminib for CML-CP resistant/intolerant to ≥ 2 TKIs.
References
Mahon FX, Réa D, Guilhot J, Guilhot F, Huguet F, Nicolini F, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11(11):1029–35.
Hughes TP, Clementino NCD, Fominykh M, Lipton JH, Turkina AG, Moiraghi EB, et al. Long-term treatment-free remission in patients with chronic myeloid leukemia after second-line nilotinib: ENESTop 5-year update. Leukemia. 2021;35(6):1631–42.
Imagawa J, Tanaka H, Okada M, Nakamae H, Hino M, Murai K, et al. Discontinuation of dasatinib in patients with chronic myeloid leukaemia who have maintained deep molecular response for longer than 1 year (DADI trial): a multicentre phase 2 trial. Lancet Haematol. 2015;2(12):e528–35.
Réa D, Mauro MJ, Boquimpani C, Minami Y, Lomaia E, Voloshin S, et al. A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood. 2021;138(21):2031–41.
Okada M, Imagawa J, Tanaka H, Nakamae H, Hino M, Murai K, et al. Final 3-year results of the dasatinib discontinuation trial in patients with chronic myeloid leukemia who received dasatinib as a second-line treatment. Clin Lymphoma Myeloma Leuk. 2018;18(5):353-60.e1.
Acknowledgements
This work was supported by the National Cancer Center Research and Development Fund (2021-A-11) from the Ministry of Health, Labour and Welfare.
Disclosures
Y.M.: Bristol-Myers Squibb, Novartis Pharma KK, Pfizer Japan, Inc., and Takeda (honoraria).
Author information
Authors and Affiliations
Contributions
RY performed experiments, collected and analyzed the data, interpreted the data, and co-wrote the manuscript. YM planned and performed experiments, collected and analyzed the data, interpreted the data, and co-wrote the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yoshimaru, R., Minami, Y. Achievement of deep molecular response and treatment-free remission with asciminib treatment in CML. Int J Hematol 120, 512–514 (2024). https://doi.org/10.1007/s12185-024-03816-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-024-03816-x