Abstract
Introduction
The peptide-based cancer vaccine targeting Wilms’ tumor 1 (WT1) is a promising immunotherapeutic strategy for hematological malignancies. It remains unclear how long and to what extent the WT1-specific CD8 + cytotoxic T cell (CTL) persist after WT1 peptide vaccination.
Methods
The WT1 peptide vaccine was administered with written consent to a patient with CML in the chronic phase who did not respond well to imatinib, and the patient was followed for 12 years after vaccination. Immune monitoring was performed by specific amplification of WT1-specific CTLs using a mixed lymphocyte peptide culture. T-cell receptors (TCRs) of amplified WT1-specific CTLs were analyzed using next-generation sequencing. This study was approved by the Institutional Review Board of our institution.
Result
WT1-specific CTLs, which were initially detected during WT1 peptide vaccination, persisted at a frequency of less than 5 cells per 1,000,000 CD8 + T cells for more than 10 years. TCR repertoire analysis confirmed the diversity of WT1-specific CTLs 11 years after vaccination. CTLs exhibited WT1 peptide-specific cytotoxicity in vitro.
Conclusion
The WT1 peptide vaccine induced an immune response that persists for more than 10 years, even after cessation of vaccination in the CML patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances have been achieved in cancer immunotherapy in recent years [1]. Peptide-based cancer vaccines represent one of the cancer immunotherapeutic strategies under development [2]. Cancer-testis antigens (CTAs) are regarded as an ideal target because they are highly expressed in cancers, but rarely in normal tissues (except the testis) [3]. The CTA peptide vaccine involves the administration of a single or multiple 9-11mer peptides with an adjuvant for the induction of anti-tumor immune responses [3, 4]. The production of functional T cells and the persistence of T-cell memory are important factors for successful vaccine therapy [5, 6].
Wilms’ Tumor 1 (WT1) is a CTA and the WT1 gene is overexpressed in hematological malignancies and most of all solid tumors [4, 7]. Several clinical trials have been conducted on the effects of WT1 peptide vaccines on various cancer types and have demonstrated high safety [8,9,10,11,12,13]. Although the majority of patients did not achieve a better clinical response than stable disease, some showed clear clinical responses, such as decreases in blast counts or WT1 transcript levels in acute myeloid leukemia and tumor regression in recurrent malignant glioma [10,11,12]. To increase clinical efficacy, therapeutic strategies, such as dendritic cell vaccines and combinations with WT1 helper peptides, have been developed to enhance immune responses [14,15,16]. Immunological responses have been assessed using the WT1/MHC tetramer assay, intracellular cytokine response as detected by flow cytometry and interferon-gamma enzyme-linked immune-spot (ELISPOT) assay within 2 years of vaccination [9,10,11,12,13]. These assays have successfully confirmed the transient WT1-specific immune response observed in many cases early after vaccination. However, previous reports are limited to descriptions of the months during which WT1 vaccine was administered. Therefore, whether the WT1-specific immune response persists after WT1 peptide vaccine cessation remains unclear. Furthermore, the repertoire of WT1-specific CD8 + cytotoxic T lymphocytes (CTLs) after WT1 vaccination has not yet been reported.
We previously reported the case of a patient with CML who was administered the WT1 peptide vaccine and achieved substantial molecular response with the persistence of WT1-specific CTLs for 2 years [17]. In this report, we describe WT1-specific CTLs that persisted long after the cessation of the WT1 peptide vaccine using a mixed lymphocyte peptide culture (MLPC) assay. We performed functional assays and T-cell receptor (TCR) repertoire analyses of WT1-specific CTLs in this CML patient 12 years after cessation of the WT1 vaccine.
Methods
Administration of the WT1 peptide
The HLA-A*24:02-restricted modified-type WT1 peptide (WT1 peptide; 9mer peptide of CYTWNGMNL, synthesized by PolyPeptide, San Diego, USA), which exhibits anti-tumor immunogenicity, was subcutaneously administered at a dose of 1 mg every 2 weeks [17]. Since a previous study reported that some anti-tumor CD8 + CTLs lose their cytolytic activity with a strong antigenic stimulation [18], the interval for the WT1 peptide administration was changed from two weeks to four weeks from the 12th to 22nd administration [19]. Montanide ISA-51 VG (Seppic, Paris, France) was used as the adjuvant of the vaccination. The administration of the WT1 peptide was approved by the Institutional Review Board of Niigata University School of Medicine and performed after informed consent was obtained.
Quantification of BCR-ABL transcripts
BCR-ABL transcripts in peripheral blood samples were measured using a high-sensitivity Amp-CML assay, which is based on the transcription-mediated amplification (TMA) method [20], in the first 7 years. In our laboratory, a 3-log reduction was calculated as 280 copies in 1 µg of cellular RNA from 120 CML patients. After the seventh year following the vaccination, we measured the BCR-ABL/ABL ratio using real-time RT-PCR and the International Scale (IS) [21]. A deep molecular response (DMR) was defined as a 4.5 log reduction in the IS% BCR-ABL/ABL.
MLPC assay
The method for the MLPC assay was previously described [17]. Briefly, mononuclear cells (MNCs) were isolated from a peripheral blood sample using density gradient centrifugation with Lymphoprep™ (Cosmo Bio, Tokyo, Japan). Freshly isolated MNCs were divided into 20 wells or more on a 96-well round-bottomed plate. Each well equally contained 3 × 105 MNCs at the start of the MLPC assay. MNCs were cultured with 5% autologous serum containing RPMI1640, 10 μg/ml of the WT1 peptide, and 50 U/ml of IL-2 (Shionogi, Osaka, Japan). A two-week culture was performed, and the culture medium was changed every 1–3 days. Thereafter, MLPC cells in each well were individually analyzed by tetramer assay using WT1 peptide/HLA-A*24:02 tetramer-PE (WT1 tetramer; MBL, Nagoya, Japan) and CD8-FITC (clone SK1, BD Bioscience, New Jersey, USA) by flow cytometry. The wells containing WT1-specific CD8 + T cells were called MLPC-positive wells. The estimated frequency of WT1-specific CD8 + T cells was calculated using the following formula: number of MLPC-positive wells × 106 / [(total number of analyzed wells) × (number of divided MNCs in a well) × (percentage of CD8 + T cells in MNCs before MLPC/100)] (cells /106 CD8 + T cells).
Cytotoxicity assay
The cytotoxicity assay for MLPC cells was previously described [22]. Briefly, GFP gene-transduced T2A24 cells (T2A24-GFP) were pre-incubated with or without 10 μg/ml of the WT1 peptide overnight and then used as target cells. MLPC cells were integrated by the presence or absence of WT1-specific CD8 + T cells in each well and then used as effector cells.
Effector cells and target cells were mixed at a ratio of 15:1 and incubated for 4 h. The supernatants of these mixed cells were subjected to an IFN-γ enzyme-linked immunosorbent assay (ELISA) using the VeriKineTM Human Interferon Gamma ELISA Kit (PBL Assay Science, New Jersey, USA) according to the manufacturer’s protocol. These mixed cells were also stained by 7-AAD, and the number of viable target cells (GFP + /7-AAD −) was determined using flow cytometry for 120 s at a constant flow velocity in all samples. Percent cytotoxicity in the assay was calculated using the following formula: % Cytotoxicity = [(absolute number of viable target cells in the tube containing target cells only − absolute number of viable target cells in the sample tube) / absolute number of viable target cells in the tube containing target cells only] × 100.
Flow cytometry
Flow cytometry was used for the tetramer assay as previously described [17]. In addition, MLPC cells for the tetramer assay were stained with anti-human fluorescein-conjugated antibodies for CD45RA (PE-cyanine7, clone 2H4, Beckman Coulter, CA, USA) and CD62L (APC-cyanine7, clone DREG-56, Biolegend, Tokyo, Japan) to analyze the T-cell-differentiated phenotype [23,24,25]. MLPC cells were stained with CD39 (PE-cyanine7, clone A1, Biolegend, Tokyo, Japan). CD39 is not only an exhaustion marker but also a marker for tumor antigen-specific CD8 + T cells in tumor-infiltrating T cells [26,27,28]. Previous study showed that sustained TCR stimulation for more than a week upregulated CD39 expression in vitro [28]. Live T cells were separated by 7-AAD (Biolegend, Tokyo, Japan) and isotype controls were used for adequate gating. The gating of WT1-specific CD8 + T cells was performed after a background assessment using HLA-A*24:02-negative tetramer-PE (MBL, Nagoya, Japan). All antibody reagents were used according to the manufacturer’s protocol. Fc receptor blocking buffer was added to all samples. Flow cytometry was performed on FACSCalibur (BD Biosciences) or CytoFLEX (Beckman Coulter) and analyzed using CytExpert software (Beckman Coulter).
TCR repertoire analysis of WT1-specific CD8 + T-cell clones
The MLPC assay was modified as follows to harvest enough WT1-specific CT8 + T cells for the TCR repertoire analysis: cytokines for cultures were changed from IL-2 to 10 ng/ml of IL-15 and IL-21 because of their synergistic effects on CD8 + T-cell expansion [29]. Expanded WT1-specific CD8 + T-cell clones were sorted as the lymphocyte fraction with double positivity for the WT1 tetramer and CD8 per well using FACSAria (BD Biosciences). The next-generation sequencing of T-cell receptor β (TCRB) and a bioinformatics analysis of the sorted cells were performed by Repertoire Genesis Incorporation (Osaka, Japan) using the unbiased gene amplification method with Adaptor-Ligation PCR [30]. Out-of-frame sequences were excluded from the analysis.
Statistical analysis
The Student’s t-test was used to assess the significance of differences in the results of the cytotoxicity assay, which was conducted in triplicate under each condition. Two-tailed P-values < 0.05 were considered to be significant.
Result
Clinical course of a patient with CML who received the WT1 peptide vaccine
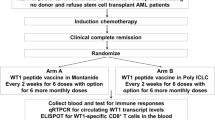
A patient with CML in the chronic phase (53 years old, male, HLA-A*24:02-positive) was administered the WT1 peptide vaccination after providing written informed consent because bcr-abl transcripts were gradually increasing during a treatment with imatinib and second-generation TKIs were not available at that time [17]. The clinical course of the patient during 13 months of the vaccination and first one year after the cessation of vaccination was previously described. Briefly, the copy number of major bcr-abl transcripts gradually decreased and became undetectable by the TMA method after the first year of the cessation [17]. The subsequent clinical course is shown in Fig. 1. The RT-PCR method using IS was introduced and DMR was identified in the sixth year of cessation. Imatinib, which had been continued before and after the WT1 peptide vaccination, was discontinued due to anemia in the eighth year of the cessation. Thereafter, the patient maintained DMR without any TKIs for more than 3 years.
Changes of bcr-abl transcripts and WT1-specific CTLs in a WT1 peptide vaccinated CML patient. The results of clinical and immune monitoring for 13 years after vaccination were shown. The level of BCR-ABL transcripts were measured using high-sensitivity Amp-CML assay, which is based on the transcription-mediated amplification method for the first 5 years after the cessation of the WT1 peptide vaccine (*) and then by BCR-ABL/ABL ratio using real-time RT-PCR method and International Scale (IS) (†). Estimated frequency of WT1-specific CD8 + T cells were shown as immune monitoring
Continuous monitoring of WT1-specific CD8 + T cells by the MLPC assay
As previously described, WT1-specific CD8 + T cells were undetectable by the MLPC assay before the WT1 peptide vaccination [17]. After vaccination, WT1-specific CD8 + T cells became detectable, and the estimated frequency of WT1-specific CD8 + T cells peaked in the second year after cessation of vaccination (27 cells per 106 CD8 + T cells) and then slowly declined [17]. Ten years after the cessation of vaccination, WT1-specific CD8 + T cells were found to persist at a frequency of less than 5 cells per 106 CD8 + T cells (0.0005%). The results of the MLPC assay in the 11th year (Fig. 2A) revealed precise populations of WT1-specific CD8 + T cells. The major phenotypes of all WT1-specific CD8 + T cells were CD62L (−) and CD45RA (−); however, one population of WT1-specific CD8 + T cells contained a fraction of CD62L (+) and CD45RA (−) as the minor phenotype (Fig. 2B).
Results of the MLPC assay were performed 11 years after cessation of the WT1 peptide vaccine. A MLPC cells in 20 wells (Nos. 1–20) were cultured using the MLPC method. Wells 3, 5, 14, and 19 contained WT1-specific CD8 + T cells and were MLPC-positive. No clear WT1 tetramer-binding CD8 + T cells were detected prior to MLPC. B Differences in the properties of WT1-specific CD8 + T cells among MLPC cells. WT1-specific CD8 + T cells in well 14 expressed CD45RA (−) and CD62L (−) as the effector memory phenotype, whereas WT1-specific CD8 + T cells in well 5 partially expressed CD45RA (−) and CD62L (+) as the central memory phenotype. WT1 tetramer-unbound CD8 + T cells in well no. 14 were used as positive controls. C, D Cytotoxicity assay of WT1-specific CD8 + T cells obtained by MLPC assay. The target cells were T2A24-GFP cells pulsed with or without the WT1 peptide, and the effector cells were MLPC cells containing WT1-specific CD8 + T cells (+) or not (−). The percent cytotoxicity was calculated using the counts of viable target cells [GFP (+) and 7-AAD (−)] and analyzed by flow cytometry. C The concentration of IFN-γ released during the cytotoxicity assay was measured using ELISA (D). All experiments were performed in triplicates. Student’s t-test was used to assess the significance of differences
Cytotoxic functionality of WT1-specific CD8 + T cells that persisted after the vaccine cessation
The cytotoxic functionality of the detected WT1-specific CD8 + T cells was evaluated using an MLPC assay 11 years after the cessation of WT1 vaccination. The cells in the positive wells were harvested into one tube (MLPC-positive cells containing 5.3% WT1 tetramer + CD8 + T cells) and used as effector cells, whereas the MLPC-negative cells were used as controls. When using target cells (T2A24-GFP cells) pulsed with the WT1 peptide, the cytotoxicity rate in MLPC-positive cells was 37% (1% in control), and the concentration of IFN-γ in the supernatant was 327 ng/mL (24 ng/mL in control). In contrast, when using target cells without the WT1 peptide pulse, the rate of cytotoxicity and the concentration of IFN-γ in the supernatant were low and comparable to those in the control (Fig. 2C, D). In summary, WT1-specific CD8 + T cells detected in the MLPC assay were CTLs that retained WT1-specific cytotoxicity.
The diversity of TCRs in decade-long WT1-specific CTLs
WT1-specific CD8 + T cells detected by the MLPC assay occasionally showed different fluorescence intensities for the WT1/MHC tetramer in each well (Fig. 2A). Therefore, we hypothesized that WT1-specific CD8 + T cells with TCRs that exhibit different affinities for the WT1/MHC complex might be simultaneously present in the patient. CD39 is one of the markers expressed by CTLs chronically exposed to intense TCR stimulation [26, 28]. In support of our hypothesis, WT1-specific CD8 + T cells showed different CD39 expressions in diverse wells, despite receiving the same stimulation with the WT1 peptide (Fig. 3A). To determine whether a specific TCR has been used in WT1-specific CD8 + T cells, sequencing analysis of TCRβ was performed on wells in which enough WT1 tetramer + CD8 + T cells were sorted by flow cytometry. We conducted these analyses on three occasions in the period from the 11th to 12th year after vaccine cessation. These results demonstrated the presence of diverse TCRs in WT1-specific CD8 + T cells (Fig. 3B). However, no TCRs were continuously detected in multiple analyses. Thus, no predominant WT1-specific CD8 + T-cell clones were identified in the patient with CML.
Results of sequencing analysis on TCRβ of WT1-specific CTLs detected by MLPC assays. A Three of the WT1-specific CTLs for analyses were obtained using the MLPC assay in the 11th year after WT1 vaccine cessation. Each of the three CTLs differed in the fluorescence intensity of the WT1/MHC tetramer and the expression of CD39. B Sequencing analyses were performed three times between the 11th and 12th year after the WT1 vaccine cessation. Although various TCRs were detected, any recurrently detected TCRs were not found
Discussion
The present study demonstrated that HLA-A*24:02-restricted modified-type WT1 peptide vaccine therapy induced WT1-specific immune effects for a long period of time (more than 10 years) based on the continuous detection of WT1-specific CTLs in the CML patient using the MLPC assay.
WT1-specific CTLs, which were amplified from the same WT1 peptide, possessed a diversity of TCRs. A previous study reported that each T cell has cross-reactivity and also that numerous possible TCRs may bind to the same antigen [31]. WT1-specific CTL lines have been successfully established from healthy donors using the same modified WT1 peptide employed in the present study, and the sequences of TCR-BVs in each clone differed [32, 33]. However, in these studies, the diversity of the TCRs of WT1-specific CTLs in a single donor was not clearly demonstrated because WT1-specific CTL lines were established from more than one patient. Furthermore, there is currently no information on the diversity of the TCRs of WT1-specific CTLs in patients after WT1 peptide vaccinations. In the present study, we showed for the first time that WT1-specific CTLs were induced with diversity in a single patient who received the WT1 peptide vaccine. We did not identify any dominant TCRs that were repeatedly detected in the sequential analysis at least 10 years after the WT1 peptide vaccine. The WT1-specific cytotoxicity of WT1-specific CTLs obtained by the MLPC assay has been maintained in the absence of a specific predominant TCR. It should be noted that the MLPC assay is not a comprehensive method to analyze all WT1-specific CTLs present in a patient, because only CTL clones which adapted to MLPC conditions had been amplified and analyzed. Although the TCRs we analyzed may be only a small part, however, the present results suggest that the WT1 peptide vaccination induces functional WT1-specific CTLs with different TCRs in the long term.
A previous study reported differences in affinity to the WT1 peptide/MHC complex and cytotoxicity among WT1-specific CTL clones with different TCRs [32]. Although we did not directly compare the functionalities of each CTL in the present study, the following two results suggested that the affinity for the WT1 peptide/MHC complex and functionality may differ in each CTL. CTLs with different phenotypes related to their function were amplified regardless of the same culture procedure. Furthermore, the WT1 tetramer assay showed that the fluorescence intensity of the WT1 tetramer differed for each WT1-specific CTL. In previous studies that compared the properties of clones with the different fluorescence intensities of the WT1 tetramer, CTL clones with stronger WT1 tetramer fluorescence intensity (WT1-tetramerhigh CTL) had higher levels of CD5, a marker of resistance to activation-induced cell death, and were more cytotoxic than CTL clones with weaker fluorescence intensity (WT1-tetramerlow CTL) [34, 35]. Similar to these findings, CTLs with different fluorescence intensities of WT1 tetramers in the present study may have had different functionalities.
The major phenotype of all WT1-specific CTLs amplified by MLPC was CD62L (−) CD45RA (−), which is described as a phenotype of effector memory CD8 + T cells [25]; however, one of the WT1-specific CTLs contained a fraction of CD62L (+) CD45RA (−), which is described as a phenotype of central memory CD8 + T cells [25]. Central memory T cells have a higher amplification capacity and mainly produce IL-2, while effector memory T cells have a lower amplification capacity and mainly produce IFN-γ [36]. The present results also showed that WT1-specific CTLs expressing and not expressing CD39 were amplified by the MLPC assay. Previous studies demonstrated that CD39-expressing CD8 + T cells were exhausted cells that had been chronically activated by a TCR stimulation, showed the decreased production of TNF and IL-2, and had high expression levels of co-inhibitory factors [26, 37]. Also, another study showed that the expression of CD39 has been reported to be progressively upregulated by long-term TCR stimulation, while it was limited by short-term TCR stimulation [28]. This suggests that the reason for the different expression of CD39 in each WT1-specific CTL clone could involve differences in the affinity of the TCR for the HLA/WT1 peptide complex. This study clarified the existence of functionally heterogeneous CTLs that show different responsiveness to the WT1 peptide stimulation in the CML patient. However, there was several limitations regarding the analysis to the cellular phenotype and functionality of WT1-specific CTLs in this study. First, this study did not examine exhaustion markers other than CD39 or any activation markers. Second, since most of the amplified WT1-specific CTLs had insufficient cell numbers to perform cytotoxicity assays, it was difficult to investigate the direct relationship between cellular phenotype and functionality for each CTL. Finally, the phenotype of WT1-specific CTLs in vivo remained unclear in the present study due to the limitations of phenotypic changes caused by in vitro expansion. Further studies are needed in the future.
The frequency of WT1-specific CTLs estimated by the MLPC assay was less than 5 out of 1 million CD8 + T cells 8 years after the vaccination. Even with this rare existence, the clinical course of CML was favorable after the vaccination, which suggests that WT1-specific CTLs continued to exert their effects in vivo. Although the expression level of the WT1 gene transcript was not monitored, the expression level of the BCR-ABL transcript gradually decreased, confirming that this patient eventually reached DMR. An oscillation in the BCR-ABL/ABL ratio near the sensitivity threshold was observed in the patient even in the absence of TKIs, which indicated that CML stem cells were still present. However, anti-tumor immunity that suppresses the relapse of CML may also have been present [38, 39]. Although long-term analysis of immunocompetent cells other than CTL such as NK cells have not been performed in this study, it was suggested that the WT1-specific CTLs may have played a part in long-term anti-tumor immunity against CML.
In summary, we have demonstrated that the WT1 peptide vaccine induces an immune response that persists for more than 10 years, even after the cessation of vaccination in CML patients. Diverse TCRs in WT1-specific CTLs were observed in the patient.
Data availability
The data that support the findings of this study are available from the corresponding author, M.M., upon reasonable request.
References
Yang Y. Cancer immunotherapy: harnessing the immune system to battle cancer. J Clin Invest. 2015;125(9):3335–7.
Butterfield LH. Cancer vaccines. BMJ. 2015;350: h988.
Wei X, Chen F, Xin K, Wang Q, Yu L, Liu B, et al. Cancer-testis antigen peptide vaccine for cancer immunotherapy: progress and prospects. Transl Oncol. 2019;12(5):733–8.
Di Stasi A, Jimenez AM, Minagawa K, Al-Obaidi M, Rezvani K. Review of the results of WT1 peptide vaccination strategies for myelodysplastic syndromes and acute myeloid leukemia from nine different studies. Front Immunol. 2015;6:36.
Ahlers JD, Belyakov IM. Memories that last forever: strategies for optimizing vaccine T-cell memory. Blood. 2010;115(9):1678–89.
Klebanoff CA, Gattinoni L, Restifo NP. CD8+ T-cell memory in tumor immunology and immunotherapy. Immunol Rev. 2006;211:214–24.
Oka Y, Tsuboi A, Kawakami M, Elisseeva OA, Nakajima H, Udaka K, et al. Development of WT1 peptide cancer vaccine against hematopoietic malignancies and solid cancers. Curr Med Chem. 2006;13(20):2345–52.
Oji Y, Inoue M, Takeda Y, Hosen N, Shintani Y, Kawakami M, et al. WT1 peptide-based immunotherapy for advanced thymic epithelial malignancies. Int J Cancer. 2018;142(11):2375–82.
Keilholz U, Letsch A, Busse A, Asemissen AM, Bauer S, Blau IW, et al. A clinical and immunologic phase 2 trial of Wilms tumor gene product 1 (WT1) peptide vaccination in patients with AML and MDS. Blood. 2009;113(26):6541–8.
Oka Y, Tsuboi A, Taguchi T, Osaki T, Kyo T, Nakajima H, et al. Induction of WT1 (Wilms’ tumor gene)-specific cytotoxic T lymphocytes by WT1 peptide vaccine and the resultant cancer regression. Proc Natl Acad Sci U S A. 2004;101(38):13885–90.
Rezvani K, Yong AS, Mielke S, Savani BN, Musse L, Superata J, et al. Leukemia-associated antigen-specific T-cell responses following combined PR1 and WT1 peptide vaccination in patients with myeloid malignancies. Blood. 2008;111(1):236–42.
Tsuboi A, Hashimoto N, Fujiki F, Morimoto S, Kagawa N, Nakajima H, et al. A phase I clinical study of a cocktail vaccine of Wilms’ tumor 1 (WT1) HLA class I and II peptides for recurrent malignant glioma. Cancer Immunol Immunother. 2019;68(2):331–40.
Ueda Y, Ogura M, Miyakoshi S, Suzuki T, Heike Y, Tagashira S, et al. Phase 1/2 study of the WT1 peptide cancer vaccine WT4869 in patients with myelodysplastic syndrome. Cancer Sci. 2017;108(12):2445–53.
Anguille S, Van de Velde AL, Smits EL, Van Tendeloo VF, Juliusson G, Cools N, et al. Dendritic cell vaccination as postremission treatment to prevent or delay relapse in acute myeloid leukemia. Blood. 2017;130(15):1713–21.
Kan S, Bito T, Shimabuku M, Taguchi J, Ohkusa T, Shimodaira S, et al. Impact of mature dendritic cells pulsed with a novel WT1 helper peptide on the induction of HLAA2restricted WT1reactive CD8+ T cells. Int J Oncol. 2020;57(4):1047–56.
Fujiki F, Oka Y, Tsuboi A, Kawakami M, Kawakatsu M, Nakajima H, et al. Identification and characterization of a WT1 (Wilms Tumor Gene) protein-derived HLA-DRB1*0405-restricted 16-mer helper peptide that promotes the induction and activation of WT1-specific cytotoxic T lymphocytes. J Immunother. 2007;30(3):282–93.
Narita M, Masuko M, Kurasaki T, Kitajima T, Takenouchi S, Saitoh A, et al. WT1 peptide vaccination in combination with imatinib therapy for a patient with CML in the chronic phase. Int J Med Sci. 2010;7(2):72–81.
Demotte N, Stroobant V, Courtoy PJ, Van Der Smissen P, Colau D, Luescher IF, et al. Restoring the association of the T cell receptor with CD8 reverses anergy in human tumor-infiltrating lymphocytes. Immunity. 2008;28(3):414–24.
Saitoh A, Narita M, Watanabe N, Tochiki N, Yamahira A, Nakamura T, et al. WT1 peptide vaccination in a CML patient: induction of effective cytotoxic T lymphocytes and significance of peptide administration interval. Med Oncol. 2011;28(1):219–30.
Nakamae H, Yoshida C, Miyata Y, Hidaka M, Uike N, Koga D, et al. A new diagnostic kit, ODK-1201, for the quantitation of low major BCR-ABL mRNA level in chronic myeloid leukemia: correlation of quantitation with major BCR-ABL mRNA kits. Int J Hematol. 2015;102(3):304–11.
Hughes T, Deininger M, Hochhaus A, Branford S, Radich J, Kaeda J, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108(1):28–37.
Iwabuchi M, Narita M, Uchiyama T, Iwaya S, Oiwa E, Nishizawa Y, et al. Enhancement of the antigen-specific cytotoxic T lymphocyte-inducing ability in the PMDC11 leukemic plasmacytoid dendritic cell line via lentiviral vector-mediated transduction of the caTLR4 gene. Mol Med Rep. 2015;12(2):2443–50.
Tanaka-Harada Y, Kawakami M, Oka Y, Tsuboi A, Katagiri T, Elisseeva OA, et al. Biased usage of BV gene families of T-cell receptors of WT1 (Wilms’ tumor gene)-specific CD8+ T cells in patients with myeloid malignancies. Cancer Sci. 2010;101(3):594–600.
Nakata J, Nakajima H, Hayashibara H, Imafuku K, Morimoto S, Fujiki F, et al. Extremely strong infiltration of WT1-specific CTLs into mouse tumor by the combination vaccine with WT1-specific CTL and helper peptides. Oncotarget. 2018;9(89):36029–38.
Golubovskaya V, Wu L. Different subsets of T cells, memory, effector functions, and CAR-T immunotherapy. Cancers (Basel). 2016;8(3):36.
Canale FP, Ramello MC, Nunez N, Araujo Furlan CL, Bossio SN, Gorosito Serran M, et al. CD39 expression defines cell exhaustion in tumor-infiltrating CD8(+) T cells. Cancer Res. 2018;78(1):115–28.
Simoni Y, Becht E, Fehlings M, Loh CY, Koo SL, Teng KWW, et al. Bystander CD8+ T cells are abundant and phenotypically distinct in human tumour infiltrates. Nature. 2018;557(7706):575–9.
Duhen T, Duhen R, Montler R, Moses J, Moudgil T, de Miranda NF, et al. Co-expression of CD39 and CD103 identifies tumor-reactive CD8 T cells in human solid tumors. Nat Commun. 2018;9(1):2724.
Zeng R, Spolski R, Finkelstein SE, Oh S, Kovanen PE, Hinrichs CS, et al. Synergy of IL-21 and IL-15 in regulating CD8+ T cell expansion and function. J Exp Med. 2005;201(1):139–48.
Kitaura K, Yamashita H, Ayabe H, Shini T, Matsutani T, Suzuki R. Different somatic hypermutation levels among antibody subclasses disclosed by a new next-generation sequencing-based antibody repertoire analysis. Front Immunol. 2017;8:389.
Sewell AK. Why must T cells be cross-reactive? Nat Rev Immunol. 2012;12(9):669–77.
Morimoto S, Fujiki F, Kondo K, Nakajima H, Kobayashi Y, Inatome M, et al. Establishment of a novel platform cell line for efficient and precise evaluation of T cell receptor functional avidity. Oncotarget. 2018;9(75):34132–41.
Watanabe K, Toji S, Ohtake J, Nakano K, Satoh T, Kitamura H, et al. Establishment of a stable T lymphoma cell line transduced with HLA-A*24:02-restricted WT1-specific TCR genes and its application to antigen-specific immunomonitoring. Biomed Res. 2013;34(1):41–50.
Kondo K, Fujiki F, Nakajima H, Yatsukawa E, Morimoto S, Tatsumi N, et al. An essential role of the avidity of T-cell receptor in differentiation of self-antigen-reactive CD8+ T cells. J Immunother. 2016;39(3):127–39.
Fujiki F, Tsuboi A, Morimoto S, Hashimoto N, Inatome M, Nakajima H, et al. Identification of two distinct populations of WT1-specific cytotoxic T lymphocytes in co-vaccination of WT1 killer and helper peptides. Cancer Immunol Immunother. 2021;70(1):253–63.
Sallusto F, Geginat J, Lanzavecchia A. Central memory and effector memory T cell subsets: function, generation, and maintenance. Annu Rev Immunol. 2004;22:745–63.
Yost KE, Satpathy AT, Wells DK, Qi Y, Wang C, Kageyama R, et al. Clonal replacement of tumor-specific T cells following PD-1 blockade. Nat Med. 2019;25(8):1251–9.
Arpinati M, Tolomelli G, Bochicchio MT, Castagnetti F, Amabile M, Bandini G, et al. Molecular monitoring of BCR-ABL transcripts after allogeneic stem cell transplantation for chronic myeloid leukemia. Biol Blood Marrow Transplant. 2013;19(5):735–40.
Clapp GD, Lepoutre T, Nicolini FE, Levy D. BCR-ABL transcript variations in chronic phase chronic myelogenous leukemia patients on imatinib first-line: possible role of the autologous immune system. Oncoimmunology. 2016;5(5): e1122159.
Acknowledgements
The present study was supported in part by JSPS KAKENHI Grant Number JP17K09006 to Y.S., JP18K07410 to M.N., and JP16K09868 to M.M. and a Japanese Society of Hematology Research Grant (2019–2020) to M.M.
Author information
Authors and Affiliations
Contributions
TS, MN, and MM designed the present study, conducted all experiments, analyzed the data obtained, and wrote the manuscript. TS and MN performed the MLPC assay. HS supervised this work. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Suwabe, T., Shibasaki, Y., Tamura, S. et al. Decade-long WT1-specific CTLs induced by WT1 peptide vaccination. Int J Hematol 119, 399–406 (2024). https://doi.org/10.1007/s12185-024-03723-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-024-03723-1