Abstract
Pediatric acute myeloid leukemia (AML) is a heterogeneous disease with various genetic abnormalities. Recent advances in genetic analysis have enabled the identification of causative genes in > 90% of pediatric AML cases. Fusion genes such as RUNX1::RUNX1T1, CBFB::MYH11, and KMT2A::MLLT3 are frequently detected in > 70% of pediatric AML cases, whereas FLT3-internal tandem duplication, CEBPA-bZip, and NPM1 mutations are detected in approximately 5–15% of cases, respectively. Conversely, mutations in DNMT3A, TET2, and IDH, which are common in adults, are extremely rare in pediatric AML. The genetic characteristics of pediatric AML are slightly different from those of adult AML. For accurate risk stratification and treatment intensity, genome analysis should be performed in a simple, fast, and inexpensive manner and the results should be returned to patients in real time. As with acute lymphoblastic leukemia, the presence or absence of minimal residual disease is an important factor in determining the success of treatment against AML, and it is important to predict prognosis and formulate treatment strategies considering the genetic abnormalities. For the development and clinical application of new molecularly targeted therapies based on identified genetic abnormalities, it is necessary to explore when and in which combinations drugs will be most effective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Annually, approximately 150 new cases of pediatric acute myeloid leukemia (AML) occur in Japan. Acute promyelocytic leukemia (APL) accounts for 10–15% of these cases with t(15;17)(q24;q21), and most cases of APL are caused by translocations forming PML::RARA chimeric genes. All-trans retinoic acid-based differentiation induction therapy has been established as a standard treatment for APL [1], while attenuated chemotherapy has been established as the standard treatment for most cases of AML associated with Down syndrome (ML-DS) [2]. Therefore, in this article, I review the necessity for future reconstruction of risk stratification and the potential of new treatment strategies in addition to focusing on genes used for the risk stratification of de novo AML, excluding APL and ML-DS, in the AML-20 phase III clinical trial currently being conducted by the JCCG in Japan.
Characteristics of the molecular basis of pediatric AML
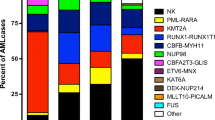
AML is a heterogeneous disease characterized by a variety of chromosomal and genetic abnormalities. Chromosomal abnormalities are more frequent in pediatric AML cases than in adult AML cases. Approximately, 40% of adult AML cases have a normal karyotype, but 70% of pediatric AML cases exhibit leukemia cell-specific translocations or structural abnormalities.
Chromosomal abnormalities and resulting fusion genes play a vital role in the development of pediatric AML. Many of these abnormalities in pediatric AML are known to correlate with treatment response and prognosis and are crucial markers for selecting treatment according to risk and for determining the indication for hematopoietic stem cell transplantation (HSCT) [3, 4]. The occurrence of genetic abnormalities varies depending on the patient’s age; KMT2A rearrangements and CBFA2T3::GLIS2 are observed in patients with AML aged < 3 years; RUNX1::RUNX1T1, CBFB::MYH11, NUP98::NSD1, and DEK::NUP214 are observed in patients with AML aged 3–14 years; RUNX1::RUNX1T1 and CBFB::MYH11 are observed in the adolescent and young adult group (15–39 years), although the incidence is lower than that in patients aged < 14 years. The frequency of fusion genes clearly decreases in patients with AML aged at least 40 years, whereas the frequency of genetic mutations increases [3, 4].
Compared with Europe and the United States, RUNX1::RUNX1T1 are highly detected in Japan, accounting for about 25–30% of all cases, and together with CBFB::MYH11, this most prevalent subgroup is known as core binding factor (CBF)-AML, accounting for one-third of all cases and exhibiting relatively low risk.
By contrast, mutations in FLT3-internal tandem duplication (ITD), NPM1, CEBPA, KIT, RAS, WT1, and KMT2A-partial tandem duplication (PTD) have been identified through previous genetic analysis studies, and the prognostic significance of FLT3-ITD, KIT, NPM1, and CEBPA mutations, which are frequently detected, has been examined. Numerous studies have been conducted on AML in both adult and pediatric populations (Table 1) [5, 6]. Since 2009, with the development of microarrays and next-generation sequencing, several genes including DNMT3A, TET2, and IDH1/2, as well as the gene mutations occurring in pediatric AML, have been identified in AML cases with a high prognostic value [7, 8]. However, these abnormalities are rare in pediatric AML, and the genetic background of pediatric AML development is somewhat different from that of adult AML [9].
Since it accounts for 5–10% of pediatric AML cases, acute megakaryoblastic leukemia (AMKL) has been regarded as a clinically and molecularly distinct disease subgroup. However, in ongoing international collaborative studies, CBFA2T3::GLIS2 and NUP98::KDM5A have been identified in AMKL via comprehensive analysis using next-generation sequencing [10,11,12]. CBFA2T3::GLIS2 was detected in 13–27% of pediatric AMKL cases, while NUP98::KDM5A was detected in 8–10% of cases, indicating that the former is a highly frequent abnormality. Other than AMKL, NUP98::KDM5A has been detected in various other AMLs [13]. The GATA1 mutation, which is a frequent finding in ML-DS, was detected in some non-ML-DS de novo AML cases. In addition, the molecular basis of AMKL is now becoming more obvious, and JAK2 and MPL mutations, which are frequently detected in myeloproliferative malignancies, have also been detected [14].
Recently, Yamato et al. have reported that genome-wide DNA methylation patterns are useful to predict prognosis. Four clusters linked to genetic alterations might be identified among pediatric patients with AML. Besides, combined with the gene expression status, the accuracy to predict relapse and survival rate was much improved (Fig. 1) [15]. Multiomics analysis might help to reveal the molecular basis of pediatric AML.
Unsupervised hierarchical clustering of DNA methylation profiles and associations between DNA methylation clusters and additional parameters. (A and B) Heatmap of the DNA methylation profiles of 64 AMLs based on unsupervised hierarchical clustering. Clustering was based on the 567 CpG sites with the most variable methylation values in the 64 studied cases. Four clusters were generated: 1, 2, 3, and 4. DNA methylation levels were classified into 3 groups according to their β value: hypermethylation (> 0.67), intermediate methylation (0.34–0.66), and hypomethylation (< 0.33), respectively. Light blue, orange, and dark orange indicate the presence of the specified mutation, high gene expression, and chromosomal aberration, respectively. Brown indicates KMT2A-MLLT3 fusion, and dark blue indicates FLT3-ITD with high allele ratio (> 0.7). Purple and black indicate non-complete remission (CR) and events and deaths, respectively. C Comparison of the Kaplan–Meier curves of OS among clusters 1–4. PTD partial tandem duplication
Treatment strategies for pediatric AML based on risk factors
Recent advances in treatment and supportive care have improved the overall survival of pediatric cancers. However, AML exhibits a relatively low survival rate (approximately 70%), and the prognosis of patients with relapsed/refractory AML is poor [3]. In clinical trials of pediatric AML in Japan so far (AML99 and AML-05 clinical trials), approximately 10% of patients failed to achieve complete remission (CR) and approximately 30% relapsed. These findings suggest that reconstructing risk stratification and improving survival rates are essential challenges.
Usefulness of minimal residual disease
Similar to acute lymphoblastic leukemia (ALL), initial response to chemotherapy has been reported to be prognostically important in AML. In the St. Jude AML02 study, Inaba et al. evaluated initial response to treatment by morphology, minimal residual disease using flow cytometry (FCM-MRD), and quantitative PCR targeting fusion gene products, such as RUNX1::RUNX1T1, and concluded that FCM-MRD after induction 1 or 2 was the most sensitive marker to predict prognosis [16]. In this St Jude AML02 study, patients with FCM-MRD < 0.1% after induction 1 had a 3-year event-free survival (EFS) rate of 73.6% (95% CI 68.6–78.6%), whereas patients with FCM-MRD ≥ 0.1% had a 3-year EFS rate of 43.1% (95% CI 36.2–50.0%, p < 0.0001), indicating a significantly worse prognosis for FCM-MRD-positive patients after initial induction remission therapy [17]. In addition, in the Children’s Oncology Group (COG) AAML03P1 study, patients with FCM-MRD < 0.1% had a relapse-free survival rate of 65.0% (95% CI 56.0–74.0%) following initial induction remission therapy, whereas patients with FCM-MRD ≥ 0.1% had a relapse-free survival rate of 30.0% (95% CI 15.0–45.0%, p < 0.001) [18]. Consequently, FCM-MRD may serve as a well-established marker in patients with AML, and the AML-20 clinical trial in Japan has just implemented FCM-MRD classification [19].
Cytogenetic characteristics of and treatment strategies for low-risk groups
In the AML-20 clinical trial, patients with CBF-AML were essentially placed in the low-risk group (cases positive for FLT3-ITD or having MRD ≥ 0.1% at the end of induction remission therapy-1 are at elevated risk in the intermediate-risk group) (Table 2). In the AML-05 clinical trial, the 3-year OS was more than 90% in the CBF-AML group, showing a favorable prognosis. Although RUNX1::RUNX1T1 and CBFB::MYH11 are often analyzed together, patients with RUNX1::RUNXIT1 showed a higher relapse rate than those with CBFB::MYH11. Tokumasu et al. detected KIT mutations in 47 of 107 patients with RUNX1::RUNX1T1 and reported that patients with KIT mutations in exons 8 and 17 had considerably higher rates of relapse and cumulative events (KIT mutations in exons 10 and 11 had no impact on prognosis) [20]. Faber et al. also reported that KIT exon17 mutations were more frequently identified in RUNX1::RUNX1T1 cases and had a considerably poorer prognosis [21]. The frequency of D816V mutations in KIT exon 17 was also examined using droplet digital PCR, and it was discovered that CBF-AML had a higher frequency of low allelic mutations than non-CBF-AML. In the present study, it was discovered that the presence of this KIT D816V-positive minor clone was associated with decreasing EFS (Fig. 2). This finding was consistent with the finding that AML cells with the KIT D816V mutation are more resistant to chemotherapy than AML cells without the mutation. However, many of the relapsed patients positive for RUNX1::RUNX1T1 were rescued via subsequent hematopoietic stem cell transplantation (HSCT), and their 3-year OS rate was approximately 80% (Fig. 3A), indicating the effectiveness of HSCT. Thus, the transplantation source at the time of relapse should be considered from an early stage.
Despite the generally excellent prognosis of CBFB::MYH11, patients under the age of 3 years have a high risk of relapse. Hara et al. reported that the EFS was approximately 50% in 46 patients enrolled in the AML-05 clinical trial (Fig. 4) [22].
Cytogenetic characteristics of and treatment strategies for intermediate-risk groups
This intermediate-risk group (IR) group is composed of various genetic alterations. As a result, this group contains a mix of cases with a good prognosis and those with a poor prognosis. For example, the prognosis of patients with KMT2A rearrangements depends on partner genes and/or MECOM expression. In particular, patients with a normal karyotype exhibit different genetic abnormalities. Patients with mutations in NPM1 and CEBPA-bZip mutations showed a good prognosis, whereas patients positive for KMT2A-PTD showed a poor prognosis.
Therefore, it is necessary to consider adopting these abnormalities as risk factors in future clinical trials. Jo et al. and Matsuo et al. reported that patients with AML with KMT2A::MLLT3 who exhibited high MECOM expression frequently relapsed and had a poor prognosis, while those who exhibited low MECOM expression had a fair prognosis [23, 24]. While patients with favorable prognosis can be cured with existing chemotherapies, CR cannot be maintained in most of patients positive for KMT2A-PTD or in patients with KMT2A rearrangement with high MECOM expression using conventional chemotherapies. Since chemotherapy significantly yields the refractory clones after relapse, a new therapeutic approach may be required. As an exploratory study, AML-20 will assess the prognostic significance of high MECOM expression.
Cytogenetic characteristics of and treatment strategies for high-risk groups
In the ongoing AML-20 clinical trial, CBFA2T3::GLIS2, NUP98::KDM5A, and other recently identified genetic abnormalities were added as high-risk factors in addition to monosomy 7, FUS::ERG, KMT2A::AFDN (AF6), and NUP98::NSD1, which have already been adopted in the AML-12 clinical trial. Besides, AML-20 clinical trial also attempted to reduce the risk of CBF-AML to intermediate risk even in patients positive for FLT3-ITD (Table 2) [19].
In this review, a comprehensive gene expression analysis was performed on samples obtained from patients enrolled in the AML99 clinical trial using microarray. The results of this analysis revealed a characteristic gene expression pattern shared by patients with NUP98::NSD1. The characteristics of this signature were highly associated with high PRDM16 expression, which is a homologous gene of MECOM and plays an important role in the activation of the HOX pathway. Many of these patients were refractory to treatment, did not experience remission, had a high rate of relapse, and did not fully recover even after HSCT. In case of non-CR, the protocol is discontinued, and second-line treatment is provided at each institution. Intriguingly, in approximately 20% of all pediatric AML cases, NUP98::NSD1-negative cases displayed the same gene expression pattern as NUP98::NSD1-positive cases, and the prognosis for these cases was poor [25]. In particular, the prognosis of patients with high PRDM16 expression and FLT3-ITD positivity is extremely poor (Fig. 5). Recently, UBTF-ITD has been identified, and patients with this mutation have been reported to show poor prognosis and elevated PRDM16 expression [26]. This significance will be assessed retrospectively in the AML-20 clinical trial.
Treatment strategies for patients with relapsed/refractory disease and non-complete remission for induction therapy
The standard chemotherapy regimen for relapsed/refractory pediatric AML has not been established, and the combination of daunorubicin (DNR), cytarabine (Ara-C), and etoposide (VP-16) used in the initial remission induction therapy should be often repeated. In particular, fludarabine, Ara-C, and granulocyte colony-stimulating factor (G-CSF) (FLAG) or FLAG with idarubicin (FALG-IDA) therapy are often used. Of the 369 AML-05 patients for whom genetic information was available, 232 were non-CBF-AML cases. Among them, the 3-year OS of 101 patients who did not receive HSCT was 80% and that of 131 patients who received HSCT was 30% (Fig. 3B). These findings suggested that conventional HSCT could not treat non-CBF-AML patients who experienced non-CR or relapse.
Exome analysis of four patients with relapsed disease showed that the clones that were initially minor and resistant to therapy were selected from multiple clones found at the time of initial relapse and that the clones with specific genetic mutations at the time of relapse proliferated. Leukemia cells exhibit a various type of clonal evolution. This suggests that leukemia cells are not a single population, but rather these cells develop resistance to anticancer drugs through a series of cytogenetic events that occur when these cells undergo repeated proliferation under the exposure of anticancer drugs. This may lead to treatment resistance, such as relapsed/refractory leukemia. These findings demonstrated the significance of initial treatment using drugs that cause total remission without the development of any refractory clones following initial induction therapy [9].
In the St. Jude AML02 study performed in the United States, patients with FCM-MRD ≥ 25% after the first course of induction therapy were treated with ADE (small dose Ara-C + DNR + VP-16) + gemtuzumab ozogamicin (GO, 3 mg/m2). Furthermore, patients with FCM-MRD ≥ 0.1% following the second course of induction therapy (Induction-2) were treated with GO alone (6 mg/m2). After confirming the safety of ADE + GO, ADE + GO was administered to patients with MRD ≥ 1.0% after completion of Induction-1, and GO alone (6 mg/m2) was discontinued. Among 29 patients with MRD ≥ 1.0% after Induction-1, 28 patients showed a decrease in MRD level and 13 patients turned negative for MRD, while 14 of 17 patients who received GO alone (6 mg/m2) showed a decrease in MRD level [27]. In the COG-AAML0531 study, a subgroup analysis of IR and HR patients who had undergone HSCT revealed a trend toward improved disease-free survival and OS in the GO combination group compared with patients who received only chemotherapy [28]. GO administration before transplantation has been reported to improve prognosis in patients who relapsed [29]. The AML-20 clinical trial compared the poor prognosis of the IR and HR groups in each course of consolidation chemotherapy with or without GO to determine whether the addition of GO improved survival rates in the IR and HR groups (Fig. 6). Clinical trials using methylation inhibitors, BCL2 inhibitors, DOT1L inhibitors, HDAC inhibitors, JAK inhibitors, MENIN inhibitors, and other agents are mostly being conducted in the United States for pediatric AML [30]. Clinical trials of CAR-T cell therapy targeting CD123 are being conducted, and other targets are also being tested in clinical trials [30]. Various therapies are currently under development. Until a new standard strategy is established, these new molecularly targeted therapies should be tailored according to the cytogenetic characteristics of each patient, and it is necessary to investigate new treatment modalities in Japan.
Treatment scheme of the AML-20 clinical trial. ALAL acute leukemia of ambiguous lineage, AML acute myeloid leukemia, APL acute promyelocytic leukemia, BMA bone marrow aspiration, CBF core binding factor, CR complete remission, HSCT hematopoietic stem cell transplantation, ML-DS myeloid leukemia associated with Down syndrome, MRD minimal residual disease, TP timepoint
Conclusion
Recent advances in molecular biology have been remarkable, and with the introduction of microarrays and next-generation sequencers, diagnostic methods for AML have evolved significantly and the cytogenetic background of AML has been clarified. Genetic analyses, as well as domestic and international analyses, have provided a better perspective on the molecular basis of AML (Fig. 7). The genomic profile of each clone at initial diagnosis should be evaluated to increase the cure rate of pediatric AML. Combination of various conventional or novel targetable drugs, cellular immunity, and conventional anticancer drugs with few side effects enable the reduction of relapse and therapy-related mortality.
References
Takahashi H, Watanabe T, Kinoshita A, Yuza Y, Moritake H, Terui K, et al. High event-free survival rate with minimum-dose-anthracycline treatment in childhood acute promyelocytic leukaemia: a nationwide prospective study by the Japanese paediatric leukaemia/lymphoma study group. Br J Haematol. 2016;174(3):437–43. https://doi.org/10.1111/bjh.14068.
Taga T, Watanabe T, Tomizawa D, Kudo K, Terui K, Moritake H, et al. Preserved high probability of overall survival with significant reduction of chemotherapy for myeloid leukemia in down syndrome: a nationwide prospective study in Japan. Pediatr Blood Cancer. 2016;63(2):248–54. https://doi.org/10.1002/pbc.25789.
Fröhling S, Scholl C, Gilliland DG, Levine RL. Genetics of myeloid malignancies: pathogenetic and clinical implications. J Clin Oncol. 2005;23(26):6285–95. https://doi.org/10.1200/JCO.2005.05.010.
Marcucci G, Haferlach T, Döhner H. Molecular genetics of adult acute myeloid leukemia: prognostic and therapeutic implications. J Clin Oncol. 2011;29(5):475–86. https://doi.org/10.1200/JCO.2010.30.2554.
Fröhling S, Schlenk RF, Stolze I, Bihlmayr J, Benner A, Kreitmeier S, et al. CEBPA mutations in younger adults with acute myeloid leukemia and normal cytogenetics: prognostic relevance and analysis of cooperating mutations. J Clin Oncol. 2004;22(4):624–33. https://doi.org/10.1200/JCO.2004.06.060.
Shimada A, Taki T, Tabuchi K, Tawa A, Horibe K, Tsuchida M, et al. KIT mutations, and not FLT3 internal tandem duplication, are strongly associated with a poor prognosis in pediatric acute myeloid leukemia with t(8;21): a study of the Japanese childhood AML cooperative study group. Blood. 2006;107(5):1806–9. https://doi.org/10.1182/blood-2005-08-3408.
Abbas S, Lugthart S, Kavelaars FG, Schelen A, Koenders JE, Zeilemaker A, et al. Acquired mutations in the genes encoding IDH1 and IDH2 both are recurrent aberrations in acute myeloid leukemia: prevalence and prognostic value. Blood. 2010;116(12):2122–6. https://doi.org/10.1182/blood-2009-11-250878.
Ley TJ, Miller C, Ding L, Raphael BJ, Mungall AJ, Robertson A, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368(22):2059–74. https://doi.org/10.1056/NEJMoa1301689.
Shiba N, Yoshida K, Shiraishi Y, Okuno Y, Yamato G, Hara Y, et al. Whole-exome sequencing reveals the spectrum of gene mutations and the clonal evolution patterns in paediatric acute myeloid leukaemia. Br J Haematol. 2016;175(3):476–89. https://doi.org/10.1111/bjh.14247.
Gruber TA, Larson Gedman A, Zhang J, Koss CS, Marada S, Ta HQ, et al. An Inv(16)(p13.3q24.3)-encoded CBFA2T3-GLIS2 fusion protein defines an aggressive subtype of pediatric acute megakaryoblastic leukemia. Cancer Cell. 2012;22(5):683–97. https://doi.org/10.1016/j.ccr.2012.10.007.
Thiollier C, Lopez CK, Gerby B, Ignacimouttou C, Poglio S, Duffourd Y, et al. Characterization of novel genomic alterations and therapeutic approaches using acute megakaryoblastic leukemia xenograft models. J Exp Med. 2012;209(11):2017–31. https://doi.org/10.1084/jem.20121343.
de Rooij JD, Hollink IH, Arentsen-Peters ST, van Galen JF, Berna Beverloo H, Baruchel A, et al. NUP98/JARID1A is a novel recurrent abnormality in pediatric acute megakaryoblastic leukemia with a distinct HOX gene expression pattern. Leukemia. 2013;27(12):2280–8. https://doi.org/10.1038/leu.2013.87.
Hara Y, Shiba N, Ohki K, Tabuchi K, Yamato G, Park MJ, et al. Prognostic impact of specific molecular profiles in pediatric acute megakaryoblastic leukemia in non-Down syndrome. Genes Chromosomes Cancer. 2017;56(5):394–404. https://doi.org/10.1002/gcc.22444.
de Rooij JD, Branstetter C, Ma J, Li Y, Walsh MP, Cheng J, Gruber TA, et al. Pediatric non-Down syndrome acute megakaryoblastic leukemia is characterized by distinct genomic subsets with varying outcomes. Nat Genet. 2017;49(3):451–6. https://doi.org/10.1038/ng.3772.
Yamato G, Kawai T, Shiba N, Ikeda J, Hara Y, Ohki KT, et al. Genome-wide DNA methylation analysis in pediatric acute myeloid leukemia. Blood Adv. 2022;6(11):3207–19. https://doi.org/10.1182/bloodadvances.2021005381.
Inaba H, Coustan-Smith E, Cao X, Pounds SB, Shurtleff SA, Wang KY, et al. Comparative analysis of different approaches to measure treatment response in acute myeloid leukemia. J Clin Oncol. 2012;30(29):3625–32. https://doi.org/10.1200/JCO.2011.41.5323.
Rubnitz JE, Inaba H, Dahl G, Ribeiro RC, Bowman WP, Taub J, et al. Minimal residual disease-directed therapy for childhood acute myeloid leukaemia: results of the AML02 multicentre trial. Lancet Oncol. 2010;11(6):543–52. https://doi.org/10.1016/S1470-2045(10)70090-5.
Loken MR, Alonzo TA, Pardo L, Gerbing RB, Raimondi SC, Hirsch BA, et al. Residual disease detected by multidimensional flow cytometry signifies high relapse risk in patients with de novo acute myeloid leukemia: a report from children’s oncology group. Blood. 2012;120(8):1581–8. https://doi.org/10.1182/blood-2012-02-408336.
Tomizawa D, Tsujimoto S, Tanaka S, Matsubayashi J, Aoki T, Iwamoto S, et al. A phase III clinical trial evaluating efficacy and safety of minimal residual disease-based risk stratification for children with acute myeloid leukemia, incorporating a randomized study of gemtuzumab ozogamicin in combination with post-induction chemotherapy for non-low-risk patients (JPLSG-AML-20). Jpn J Clin Oncol. 2022;52(10):1225–31. https://doi.org/10.1093/jjco/hyac105.
Tokumasu M, Murata C, Shimada A, Ohki K, Hayashi Y, Saito AM, et al. Adverse prognostic impact of KIT mutations in childhood CBF-AML: the results of the Japanese pediatric leukemia/lymphoma study group AML-05 trial. Leukemia. 2015;29(12):2438–41. https://doi.org/10.1038/leu.2015.121.
Faber ZJ, Chen X, Gedman AL, Boggs K, Cheng J, Ma J, et al. The genomic landscape of core-binding factor acute myeloid leukemias. Nat Genet. 2016;48(12):1551–6. https://doi.org/10.1038/ng.3709.
Hara Y, Shiba N, Yamato G, Ohki K, Tabuchi K, Sotomatsu M, et al. Patients aged less than 3 years with acute myeloid leukaemia characterize a molecularly and clinically distinct subgroup. Br J Haematol. 2020;188(4):528–39. https://doi.org/10.1111/bjh.16203.
Jo A, Mitani S, Shiba N, Hayashi Y, Hara Y, Takahashi H, et al. High expression of EVI1 and MEL1 is a compelling poor prognostic marker of pediatric AML. Leukemia. 2015;29(5):1076–83. https://doi.org/10.1038/leu.2015.5.
Matsuo H, Kajihara M, Tomizawa D, Watanabe T, Saito AM, Fujimoto J, et al. EVI1 overexpression is a poor prognostic factor in pediatric patients with mixed lineage leukemia-AF9 rearranged acute myeloid leukemia. Haematologica. 2014;99(11):e225–7. https://doi.org/10.3324/haematol.2014.107128.
Shiba N, Ichikawa H, Taki T, Park MJ, Jo A, Mitani S, et al. NUP98-NSD1 gene fusion and its related gene expression signature are strongly associated with a poor prognosis in pediatric acute myeloid leukemia. Genes Chromosom Cancer. 2013;52(7):683–93. https://doi.org/10.1002/gcc.22064.
Umeda M, Ma J, Huang BJ, Hagiwara K, Westover T, Abdelhamed S, et al. Integrated genomic analysis identifies UBTF tandem duplications as a recurrent lesion in pediatric acute myeloid leukemia. Blood Cancer Discov. 2022;3(3):194–207. https://doi.org/10.1158/2643-3230.BCD-21-0160.
O’Hear C, Inaba H, Pounds S, Shi L, Dahl G, Bowman WP, et al. Gemtuzumab ozogamicin can reduce minimal residual disease in patients with childhood acute myeloid leukemia. Cancer. 2013;119(22):4036–43. https://doi.org/10.1002/cncr.28334.
Gamis AS, Alonzo TA, Meshinchi S, Sung L, Gerbing RB, Raimondi SC, et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: results from the randomized phase III children’s oncology group trial AAML0531. J Clin Oncol. 2014;32(27):3021–32. https://doi.org/10.1200/JCO.2014.55.3628.
Niktoreh N, Lerius B, Zimmermann M, Gruhn B, Escherich G, Bourquin JP, et al. Gemtuzumab ozogamicin in children with relapsed or refractory acute myeloid leukemia: a report by Berlin-Frankfurt-Münster study group. Haematologica. 2019;104(1):120–7. https://doi.org/10.3324/haematol.2018.191841.
Rubnitz JE, Kaspers GJL. How i treat pediatric acute myeloid leukemia. Blood. 2021;138(12):1009–18. https://doi.org/10.1182/blood.2021011694.
Acknowledgements
I am grateful to Drs. Yasuhide Hayashi and Seishi Ogawa for their passionate guidance. I also gratefully acknowledge the work of past and present colleagues of the laboratory. The author would like to thank Enago (www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has nothing to declare in relation to the content of this paper’s presentation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shiba, N. Comprehensive molecular understanding of pediatric acute myeloid leukemia. Int J Hematol 117, 173–181 (2023). https://doi.org/10.1007/s12185-023-03533-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-023-03533-x