Abstract
We analyzed the distribution of tumors and lymphomas of the anterior mediastinum diagnosed between 1997 and 2016 at the National Cancer Center Hospital, Japan. The median age of 283 patients with anterior mediastinal tumors was 48 (range 6–84) years, and 143 (51%) were male. The incidence of tumors was as follows: thymoma, 34%; thymic carcinoma, 16%; primary mediastinal large B-cell lymphoma (PMBL), 13%; germ cell tumors, 10%; classical Hodgkin lymphoma (CHL), 9%; thymic cyst, 7%; metastatic tumors, 3%; T lymphoblastic leukemia/lymphoma (T-LBL), 2%; other lymphomas, 3%; and others, 3%. Of the newly diagnosed lymphomas in 60 patients, PMBL (46%) was the most frequent, followed by CHL (32%), T-LBL (12%), mucosa-associated lymphoid tissue lymphoma (3%), and other lymphomas (7%). These findings suggest a recent increase in PMBL in Japan. The frequency and subtype of lymphoma differ with age and sex. In female patients ≤40 years old, 58% of the anterior mediastinal tumors were PMBL (39%) or CHL (19%). Germ cell tumors were the most frequent in male patients ≤40 years old, followed by CHL (21%), PMBL (17%), and T-LBL (10%). This distribution may serve as a reference for routine histologic diagnosis of lymphomas in the anterior mediastinum in Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thymic tumors are rare, and their histologic diagnosis is sometimes difficult and challenging. Major thymic tumors include thymic epithelial tumors (thymoma and thymic carcinoma), malignant lymphomas, and germ cell tumors (GCTs). In the section of the thymus of World Health Organization Classification of Tumours of the Lung, Pleura, Thymus and Heart published in 2015 [1], the following malignant lymphomas were listed: primary mediastinal large B-cell lymphoma (PMBL), Hodgkin lymphoma, T lymphoblastic leukemia/lymphoma (T-LBL), extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma), B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell and classical Hodgkin lymphoma (intermediate DLBCL/CHL), anaplastic large cell lymphoma and other rare mature T- and NK-cell lymphomas, and other mature B-cell lymphomas. Other rare hematolymphoid tumors were also reported such as myeloid sarcoma [2], stem cell leukemia [3], Langerhans cell histiocytosis [4], Rosai–Dorfman disease [5], amyloidoma [6], and mast cell sarcoma associated with germ cell tumor [7].
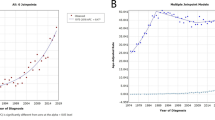
The reported incidence of PMBL between 2001 and 2006 was 0.35% of malignant lymphomas in Japan, but 0.44% in the Kantou area where our institute is located [8]. This incidence in Japan was lower than that of non-Hodgkin lymphomas (NHLs) reported in Western countries (2–4%) [9, 10]. Among Japanese children and adolescents, the reported incidence of PMBL between 1999 and 2014 was 1.0% of NHLs [11]. In Japan, the incidence of CHL has been reported as 7.03%, and that of the nodular sclerosis type as 3.14% [8] of all malignant lymphomas. Almost 80% of CHL nodular sclerosis type involves cervical lymph nodes and thymus [10]; therefore, the incidence of thymic CHL may be approximately 2–3%. The incidence of T-LBL has been reported as 0.66% [8]. In Japan, CHL is considered the most frequent subtype of thymic lymphomas, followed by T-LBL and PMBL. However, we observed through routine examination that the incidence of PMBL has recently been increasing.
The median age and sex distribution differ among malignant lymphoma subtypes. In both Japan [8] and Western countries [12], PMBL occurs mostly in young adults (median age 32 years) with a female predominance [male/female (M/F) ratio of 0.5]. CHL nodular sclerosis type also occurs predominantly in young adults (median age 37 years), but with similar sex distribution. In Japan [8], T-LBL occurs predominantly in young adults (median age 30 years) with a male predominance (M/F ratio of 1.8) [8].
The aim of this study was to delineate the recent distribution of thymic malignant lymphomas at the National Cancer Center Hospital in Japan. We presented the incidences of each histologic subtype of malignant lymphoma in the thymus, separately analyzed by age and sex.
Materials and methods
Patient selection and histopathologic diagnosis
This study included 283 consecutive patients with anterior mediastinal tumors who were histologically diagnosed at the National Cancer Center Hospital in Tokyo, Japan, between 1997 and 2016. All anterior mediastinal tumors, which were benign or malignant, primary or metastatic, histologically diagnosed at a local hospital and reviewed in our hospital, or not diagnosed histologically at the local hospital but newly diagnosed in our hospital, were included in this study. Histopathologic diagnoses were listed and separately analyzed by age and sex. Clinical information was obtained from the patients’ medical records. The study was approved by the Institutional Review Board of the National Cancer Center. All malignant lymphoma cases were diagnosed by two hematopathologists (AMM and HT) according to the World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues published in 2008 [12] and revised in 2016 [13]. The distribution of histologically diagnosed anterior mediastinal tumors was analyzed among all cases, only malignant lymphoma cases, or anterior mediastinal tumor cases separated by age and sex.
Results
Distribution of tumors in the anterior mediastinum
The distribution of all 283 anterior mediastinal tumors that were biopsied or resected is summarized in Fig. 1 and Table 1. The median age of the patients was 48 (range 6–84) years, with 143 (51%) males.
a Distribution of thymic tumors in all 283 patients. b Distribution of thymic malignant lymphomas in 76 patients. c Distribution of thymic malignant lymphomas in 60 patients who were newly diagnosed in our hospital. “Other malignant lymphomas” included MALT lymphoma (n = 2), adult T-cell leukemia/lymphoma (n = 1), anaplastic large cell lymphoma, ALK positive (n = 1), intermediate DLBCL/CHL (n = 1), myeloid sarcoma (n = 1, previously reported2), myeloid/NK precursor cell leukemia (n = 1), and stem cell leukemia/lymphoma (n = 1). “Others” included thymic hyperplasia (n = 3), atypical carcinoid tumor (n = 3), typical carcinoid tumor (n = 1), thymolipoma (n = 1), synovial sarcoma (n = 1), and leiomyoma (n = 1)
The distribution of 76 (27%) patients with malignant lymphoma is summarized in Fig. 1. The median age was 29 (range 6–68) years, and 40 (52%) patients were female. The distribution of malignant lymphoma in 60 patients, who did not achieve a histologic diagnosis at the local hospital and were newly diagnosed in our hospital, is summarized in Fig. 1. Because patients with rare tumors tend to attend to our hospital, we should demonstrate the real incidence of each malignant lymphoma subtype of the anterior mediastinum with the exception of patients referred from local hospitals who have already been diagnosed histologically as having thymic malignant lymphoma.
Distribution of tumors in the anterior mediastinum by age and sex
The distribution of tumors in the anterior mediastinum by age and sex is summarized in Fig. 2. In 51 (18%) female patients ≤40 years old (Fig. 2a), PMBL and CHL were the top two histologic subtypes. In the 60 (21%) male patients ≤40 years old (Fig. 2b), GCT (yolk sac tumor, 9 cases; mixed GCTs, 3 cases; mature cystic teratoma, 3 cases; seminoma, 2 cases; and choriocarcinoma, 1 case) was the most frequently diagnosed, followed by CHL, PMBL, and T-LBL. Notably, T-LBL occurred at a relatively high frequency (10%) only in this group. In 89 (32%) female patients >40 years old (Fig. 2c), thymic epithelial tumors were the most frequent. PMBL and CHL were seen only in 6 and 1% of the cases, respectively. In the 83 (29%) male patients >40 years old (Fig. 2d), thymic epithelial tumor, GCTs, and metastasis were frequent, but PMBL, CHL, and T-LBL occurred at a frequency of 1% each.
Methods of histologic diagnosis
Materials for histologic diagnosis were obtained by needle biopsy, open biopsy, operation after intraoperable diagnosis, only operation, or fine needle aspiration for cytology (Fig. 3a). Needle biopsies (55%) were the most frequent method for histologic diagnosis of anterior mediastinal tumors, followed by operation after intraoperable diagnosis (29%), operation (10%), open biopsy (5%), and cytology (0.4%). In 76 patients with malignant lymphomas, needle biopsy was the most frequently (81%) performed procedure, followed by open biopsy (12%). Operation (4%) and operation after intraoperable diagnosis (3%) were rarely performed (Fig. 3b). Among them, operation was performed for two cases of CHL with multicystic lesions (3%).
Discussion
We analyzed the distribution of 283 anterior mediastinal tumors histologically diagnosed between 1997 and 2016 in the National Cancer Center Hospital in Japan. Malignant lymphomas of the anterior mediastinum were diagnosed at a frequency of 27% (n = 76). These included PMBL (13%), CHL (9%), and T-LBL (2%). Among newly diagnosed malignant lymphomas of the anterior mediastinum in 60 patients at our hospital, PMBL (46%) and CHL (32%) were the most frequent, followed by T-LBL (12%) and MALT lymphoma (3%). In the present study, PMBL was the most frequently diagnosed, although reported incidences of CHL, T-LBL, and PMBL were 2–3, 0.66, and 0.35%, respectively, of all malignant lymphomas between 2001 and 2006 in Japan [8]. The present data suggested that the incidence of PMBL might be increasing in Japan, which might relate with westernization of life in Japan, or with increasing accurate diagnosis of PMBL.
The distribution of malignant lymphoma subtypes differed by age and sex. In female patients ≤40 years old, 58% of the cases were PMBL or CHL. In female patients >40 years old, malignant lymphomas were rarely seen, but 6% of the cases were PMBL. In male patients ≤40 years old, GCTs were the most frequent (30%), followed by CHL (21%), PMBL (17%), and T-LBL (10%). Notably, T-LBLs were concentrated in this group. In male patients >40 years old, malignant lymphomas were rarely seen. We should recognize this distribution and refer to it as a guide for routine histologic diagnosis of anterior mediastinal tumors in Japan.
PMBL has large nuclei and often shows wide clear cytoplasm and CD30-positivity. Although these features somewhat mimic CHL, the presence of large proliferating CD20-positive cells with dense and diffuse appearance enable diagnosis of PMBL. In male patients, differential diagnosis of large cell tumors with clear cytoplasm includes seminoma and yolk sac tumor. They can be diagnosed using immunohistochemistry, but a recent report indicated that some DLBCL cases [2/11 (18%) of testicular DLBCLs, 6/134 (5%) of non-testicular DLBCLs, and 2/6 (33%) of primary central nervous system lymphoma] were positive for OCT4, a well-known germ cell marker [14]. Therefore, the differential diagnosis should be performed using other germ cell markers such as SALL4 in combination. We should also pay attention to the presence of rare hematolymphoid malignancies such as myeloid sarcoma [2] or stem cell leukemia [3] in the thymus. In addition, recent advances in interventional radiology have led to an increase in needle biopsy materials, which make pathologic diagnosis difficult. We think that 2 or more needle biopsy materials should be obtained for accurate diagnosis. If histologic diagnosis could not be completed because of small sample size, open biopsy should be considered for the next step.
T-LBL occurs mainly in young adults, but at a low frequency; however, it is a highly aggressive leukemia/lymphoma that requires prompt diagnosis. Immunophenotypes of T cells in both thymoma and T-LBL were similar. If there is obvious nuclear atypia in T cells, a diagnosis of T-LBL can be made. However, in cases of mild nuclear atypia in T cells, a differential diagnosis is needed to determine if thymoma or T-LBL is present. Diffuse distribution of keratin-positive thymic epithelial cells suggests thymoma, whereas sparsely distributed keratin-positive thymic epithelial cell islands suggest T-LBL.
This study has several limitations. First, the present study is a single-institution study and the number of patients is not large. Second, patients whose tumors were not diagnosed histologically at a local hospital, that is, patients whose tumors were difficult to pathologic diagnosis, or patients with bulky thymic mass and symptoms who needed immediate treatment, often attended to our institution.
In conclusion, the present study suggests that the incidence of PMBL might recently be increasing in Japan. The frequency and subtype of malignant lymphomas differ by age and sex. We hope this data might contribute to accurate histologic diagnosis of thymic malignant lymphomas.
References
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. World Health Organization Classification of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2015.
Ueda R, Maruyama D, Nomoto J, Maeshima AM, Fukuhara S, Kitahara H, et al. FUS-ERG gene fusion in isolated myeloid sarcoma showing uncommon clinical features. Oxf Med Case Rep. 2016;2016:4–8.
Nagata T, Higashigawa M, Nagai M, Zhang XL, Azuma E, Komada Y, et al. A child case of CD34+, CD33+, HLA-DR−, CD7+, CD56+ stem cell leukemia with thymic involvement. Leuk Res. 1996;20:983–5.
Yagci B, Varan A, Uner A, Akyuz C, Buyukpamukcu M. Thymic langerhans cell histiocytosis mimicking lymphoma. Pediatr Blood Cancer. 2008;51:833–5.
Wu W, Cao L, Li Y, Yu X, Huang H, He J. Primary splenic diffuse large B-cell lymphoma in a patient with thymus Rosai–Dorfman disease. Am J Med Sci. 2012;344:155–9.
Takamori S, Yano H, Hayashi A, Fukunaga M, Miwa K, Maeshiro K, et al. Amyloid tumor in the anterior mediastinum: report of a case. Surg Today. 2004;34:518–20.
Yamashita A, Saito T, Akaike K, Arakawa A, Yoshida A, Kikuchi K, et al. Mast cell sarcoma of the sternum, clonally related to an antecedent germ cell tumor with a novel D579del KIT mutation. Virchows Arch. 2017;470:583–8.
Aoki R, Karube K, Sugita Y, Nomura Y, Shimizu K, Kimura Y, et al. Distribution of malignant lymphoma in Japan: analysis of 2260 cases, 2001–2006. Pathol Int. 2008;58:174–82.
Barth TF, Leihauser F, Joos S, Bentz M, Moller P. Mediastinal (thymic) large B-cell lymphoma: where do we stand? Lancer Oncol. 2002;3:229–34.
Cazals-Hatem D, Lepage E, Brice P, Ferrant A, d’Agay MF, Baumelou E, et al. Primary mediastinal large B-cell lymphoma. A clinicopathologic study of 141 cases compared with 916 non-mediastinal large B-cell lymphomas, a GELA (“Groupe d’Etude des lymphomes de l’Adulte”) study. Am J Surg Pathol. 1996;20:877–88.
Osumi T, Tanaka F, Mori T, Fukano R, Tsurusawa M, Oshima K, et al. Primary mediastinal large B-cell lymphoma in Japanese children and adolescents. Int J Hematol. 2017;105:440–4.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. World Health Organization classification of tumors of haematopoietic and lymphoid tissues. Lyon: IARC Press; 2008.
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Williams AS, Shawwa A, Merrimen J, Dakin Haché K. Expression of OCT4 and SALL4 in diffuse large B-cell lymphoma: an analysis of 145 consecutive cases and testicular lymphomas. Am J Surg Pathol. 2016;40:950–7.
Acknowledgements
This work was supported in part by the National Cancer Centre Research and Development Fund (26-A-4 and 26-A-24), JSPS Grants-in-Aid for Scientific Research Fund (C-25461442), and Japan Agency for Medical Research and Development Fund (17ck0106349h001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Maeshima, A.M., Taniguchi, H., Suzuki, T. et al. Distribution of malignant lymphomas in the anterior mediastinum: a single-institution study of 76 cases in Japan, 1997–2016. Int J Hematol 106, 675–680 (2017). https://doi.org/10.1007/s12185-017-2331-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-017-2331-0