Abstract
The current therapy for high-risk myelodysplastic syndrome (MDS) involves repeated cycles of the DNA demethylating agent 5-azacitidine (5-Aza), but combination treatments have been proposed to improve patient outcomes. We performed a phase Ib study to investigate the safety and tolerability of 5-Aza (75 mg/m2) combined with the histone deacetylase inhibitor panobinostat (PAN) in adult Japanese patients with MDS or chronic myelomonocytic leukemia (CMML). Eleven patients were enrolled; five received 20 mg PAN + 5-Aza and six received 30 mg PAN + 5-Aza. All patients in the 20 mg PAN cohort had MDS, while two in the 30 mg PAN cohort had MDS and three had CMML. All patients experienced ≥1 adverse event (AE) related to the study treatment, and five discontinued the study treatment because of AEs. One patient in each group exhibited dose-limiting toxicities: lung infection (PAN 20 mg + 5-Aza) and cellulitis (PAN 30 mg + 5-Aza). PAN exposure increased with ascending doses, and combination therapy did not affect PAN plasma trough concentrations. In summary, 20 or 30 mg PAN combined with 5-Aza was safe and tolerable in adult Japanese patients with CMML or MDS.
Study registration ClinicalTrials.gov Identifier: NCT01613976.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndrome (MDS) is a term used to collectively describe a heterogeneous group of hematopoietic stem cell disorders characterized by dysmorphic bone-marrow cells and ineffective hematopoiesis leading to cytopenia. Therefore, MDS patients have a high risk of symptomatic anemia, infection, or uncontrolled bleeding. Previous studies have reported that the incidence of MDS in the US is 3.3 per 100,000 [1], although others have suggested that this might be as high as 75 (from 2000 to 2008) or 162 (in 2003) per 100,000 in those aged over 65 years [2, 3]. In Japan, the age-adjusted incidence in 2008 was 1.6 for males and 0.8 for females per 100,000 [4]. Initially, the classification of MDS used the French–American–British (FAB) system; however, the classification of myeloid neoplasms has recently been extended by the World Health Organization (WHO), and this has now supplanted the FAB system for MDS classification [5]. Chronic myelomonocytic leukemia (CMML) is, therefore, classified as part of a new group that includes myeloproliferative disease/MDS overlapping disorders. Patients with MDS have a 50% risk of developing acute myelogenous leukemia (AML), which is refractory to treatment [6, 7].
The current therapy for the treatment of high-risk MDS is multiple cycles of 5-azacitidine (5-Aza), a DNA demethylating agent that functions by reversing abnormalities in DNA methylation associated with MDS. Two-phase III clinical trials in Western patients reported that 5-Aza treatment significantly (p = 0.0001) improved the overall survival rate (median 24.5 versus 15.0 months with the conventional treatment) for MDS [8, 9]; however, all patients ultimately progressed. Therefore, there is still an unmet medical need, which might be met by combination therapies that have synergistic or additive effects.
Pan-histone deacetylases (HDACs) have regulatory roles in cell proliferation, migration, and death, and alterations in their transcriptional expression might be involved in silencing tumor-suppressing genes [10]. Previous in vitro studies have demonstrated that HDAC inhibitors such as trichostatin A in combination with 5-Aza can re-induce the expression of previously silenced genes [11, 12]. Furthermore, preclinical studies and investigations of cancer patients with lymphoid and myeloid malignancies, including MDS, indicated that HDAC inhibitors have anti-tumor activity [13,14,15]. The HDACs remove acetyl groups from histone tails in gene promoter regions; in conjunction with DNA methyltransferases that add methyl groups to CpG dinucleotides, they can suppress gene transcription. The HDAC inhibitors function by suppressing the effects of HDACs to increase histone acetylation, which removes the suppression of transcription allowing the re-expression of tumor suppressor genes [13].
Preclinical and clinical studies of panobinostat (PAN), a non-selective HDAC inhibitor, reported that combination therapy with 5-Aza had synergistic beneficial effects in Western MDS patients and showed favorable efficacy and tolerance [16,17,18,19]. Based on the promising data obtained in Western MDS patients, we performed a phase Ib, open-label, multi-center, dose-escalation study to characterize and confirm the safety, tolerability, pharmacokinetics (PK), and preliminary efficacy of escalating doses of oral PAN + 5-Aza in adult Japanese patients with high-risk MDS, CMML, or AML.
Materials and methods
Patients
Patients with CMML or MDS were evaluated using International Prognostic Scoring System (IPSS) factors, and placed into four risk categories based on total scores of risk factors, including cytogenetic subgroup, bone-marrow blast percentage, and cytopenia [20]. Four centers in Japan enrolled patients for this study. Key inclusion criteria were adult (≥20 years) patients, Eastern Cooperative Oncology Group performance status (PS) ≤2, ineligible for hematopoietic stem cell transplantation (HSCT), IPSS intermediate-2/high-risk MDS (therapy-related MDS eligible), and CMML. Key exclusion criteria were experience of HSCT, prior treatment with DNA methylation inhibitor or HDAC inhibitor, chemotherapy, immunotherapy, cytokines, or investigational agent for MDS <28 days prior to treatment, except hydroxyurea, and hydroxyurea (<3 days) prior to treatment.
The study protocol and all amendments were reviewed by the Independent Ethics Committee or Institutional Review Board for each study center. The study was conducted according to the ethical principles of the Declaration of Helsinki, and written informed consent was obtained from each patient before screening.
Study design
This was a phase Ib, open-label, multi-center, dose-escalation study. The study period was from 30 August 2012 (first patient and first visit) to 19 February 2014 (last patient and last visit). The study had a PK-run-in period (PAN was administered alone and PK and safety were assessed for 3 days), and a combination treatment phase with 5-Aza (PK, tolerability, safety, and efficacy was evaluated for 28 days) (Fig. 1). In some cases, the run-in period was extended up to 7 days in cases of toxicity or for social reasons. The follow-up period included 30 days after the end of the study treatment, and patients were evaluated at least once per week.
Treatment schedule. The pharmacokinetic run-in period was prolonged up to 7 days in case of toxicity or for social reasons. Cohort 1: PAN 20 mg (oral) + 5-Aza 75 mg/m2 (SC). Cohort 2: PAN 30 mg (oral) + 5-Aza 75 mg/m2 (SC). Cohort 2 started after the evaluation of cohort 1 results. Dose-limiting toxicities (DLTs) were evaluated in the PK run-in period and cycle 1. The minimum exposure criteria were 6 doses of PAN and 6 doses of 5-Aza. DLT criteria (non-hematologic) were grade 3 of 7-day duration or grade 4 toxicities. Dagger only for cycle 1 (3 days). PAN panobinostat, PK pharmacokinetic, SC subcutaneously, 5-Aza 5-azacitidine
The primary objective was to confirm the safety and tolerability of oral PAN (20 and 30 mg) in combination with 75 mg/m2 subcutaneous 5-Aza, which is the approved dose. The secondary objective was to characterize the PK of PAN administered alone and in combination with 5-Aza. The exploratory objectives were to evaluate the preliminary activity of PAN in combination with 5-Aza and to explore the genotype status of cytochrome P450 (CYP) genes CYP2D6 and CYP2C19 and the potential correlation with PK.
The starting dose was determined to be 20 mg from the previous studies in Western and Japanese patients. A clinical safety study where PAN was administered at doses up to 20 mg orally three times per week (Monday, Wednesday, and Friday) in a 28-day cycle in Japanese patients with solid tumors or cutaneous T cell lymphoma (CLBH589B1101) showed that this dose was well-tolerated [21]. The dose-escalation decision and the tolerability assessment of each dose level were performed based on dose-limiting toxicity (DLT) data and other safety signals, such as reported adverse events (AEs), laboratory measurements, and PK. An adaptive Bayesian logistic regression model (BLRM) was also used to support the decisions [22, 23]. Patients discontinued treatment if any of the following occurred: disease progression, consent withdrawal, unacceptable toxicity, start of new MDS or CMML therapy, or if the investigator considered that treatment discontinuation was in the patient’s best interest.
Clinical procedures
The treatment groups were PAN 20 mg + 5-Aza and PAN 30 mg + 5-Aza. The drug treatment schedule and doses are shown in Fig. 1. During the combination treatment period, oral PAN was given on days 3 and 5 in the first week; days 8, 10, and 12 in the second week; and day 15 in the third week. Up to six doses of PAN were given per cycle. Subcutaneous 5-Aza (75 mg/m2) was given in a 7-day schedule of administration to all patients. Drug concentrations (PAN at the PK-run-in period, and PAN + 5-Aza in cycle 1) were measured in the plasma from blood samples obtained from patients at various timepoints using a validated LC–MS/MS method with a lower detection limit of 0.1 ng/mL. Drug metabolism pharmacogenetics were determined using blood samples at the time of screening to investigate genetic variation in metabolic enzymes relating to PAN metabolism (CYP2D6 and CYP2C19). Clinical laboratory tests included hematology, biochemistry, coagulation, free T4, thyroid-stimulating hormone, and urinalysis.
Efficacy assessment
The efficacy of the anti-leukemic activity of PAN in combination with 5-Aza was assessed at screening and periodically throughout the study, and was based on the standardized criteria proposed by the International Working Group for MDS and CMML: complete remission (CR), partial remission (PR), bone-marrow CR (BM-CR), stable disease (SD), relapse after CR or PR, disease progression (PD), hematologic improvement (HI), and relapse after HI [24].
Safety assessment
Safety of the drug treatment was assessed by recording all AEs, serious AEs (SAEs), and adverse drug reactions (ADRs), as well as laboratory evaluations, physical examination, vital signs, weight, PS evaluation (according to Eastern Cooperative Oncology Group scale), electrocardiography, and monitoring of thyroid function. Severity of the AEs was based on the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI CTCAE version 4.03). DLTs were defined as AEs or abnormal laboratory values that were assessed as related to the study drug that occurred after the first study cycle dose of PAN in the PK-run-in period and cycle 1. The minimum exposure criteria were six doses of PAN and six doses of 5-Aza, and the DLT criteria (non-hematologic) were grade 3 of 7-day duration or grade 4 toxicities.
Statistical analysis
The safety set was defined as all patients who received at least one dose of any component of the study treatment, including the PK-run-in period. The full analysis set (FAS) was defined as all patients to whom study treatment had been assigned and who had received at least one dose of any component of the study treatment. The pharmacokinetic analysis set (PAS) was defined as all patients who had at least one plasma sample providing evaluable PK data. The dose-determining set was defined as all patients from the safety set who met the minimum exposure criterion and had sufficient safety evaluations, or had experienced a DLT during the PK-run-in period and cycle 1 of the combination treatment period. PK parameters were calculated using the non-compartment analysis method using Phoenix WinNonlin (Version 6.2 Pharsight, Mountain View, CA, USA). Relationships of genotypes for CYP2D6 and CYP2C19 with PK parameters were investigated in an exploratory manner. For continuous data such as demographic data, summary statistics were presented including the mean, standard deviation, median, minimum, and maximum. Efficacy was determined from the FAS using frequencies for the patients having at least a PR and derived including the 95% confidence intervals (CIs) according to the Clopper–Pearson method.
Results
Patient characteristics and disposition
Patient characteristics are shown in Table 1. Overall, 11 patients (eight males and three females) in two cohorts were evaluated. The median age was 71 years (range 54–73 years), and 64% of the patients were ≥65 years. There were no statistically significant differences in any characteristics between the two treatment groups.
All 11 patients who received at least one dose of any component of the study treatment were included in the FAS, safety set, and PAS. Of these 11 patients, 10 were evaluable for the determination of the maximum tolerated dose, and were included in the dose-determining set. No cases of AML, as defined by the WHO classification, were evaluated. A total of four patients enrolled in this study were diagnosed with CMML; all these patients were assigned to the PAN 30 mg cohort (Table 1).
The patient disposition is shown in Table 2. The primary reasons for treatment discontinuation were AEs (46% overall), withdrawn consent by the patient (27% overall), or disease progression (27% overall) (Table 2). The median exposure to PAN in the 20 mg cohort was 13 (range 13–209) days and 164 (range 13–309) days for the 30 mg cohort. In total, 0–7 combination treatment cycles were given in the 20 mg cohort (one patient was withdrawn during the PK-run-in period before the combination treatment period) and 1–8 combination treatment cycles were given in the 30 mg cohort. The median relative dose intensity of PAN in the 20 mg cohort was 0.83 (range 0.8–1.0) and 0.53 (range 0.4–1.0) for the 30 mg cohort, which correspond 0–7 combination treatment cycles in 20 mg cohort (one patient was withdrawn during PK-run-in period before combination treatment period) and 1–8 combination treatment cycles in 30 mg cohort.
Safety evaluation
All patients had at least one AE related to the study treatment during the study. Dose escalation was based on the results observed for PAN 20 mg, and AEs were evaluated by NCI CTCAE version 4.03.
Non-hematological ADRs are shown in Table 3. Of note, grade 3/4 ADRs were rare. Hematological ADRs are shown in Table 4. Overall, grade 3/4 hematological ADRs were more common than grade 3/4 non-hematological ADRs (9% in all patients), particularly in the PAN 30 mg group. The most frequently reported ADRs were thrombocytopenia (91%), decreased appetite, neutropenia (82% each), nausea, increased blood creatinine, anemia, and leukopenia (55% each). The most frequently reported grade 3 or 4 ADRs were hematological events in both cohorts, including thrombocytopenia and neutropenia (80% each) in the PAN 20 mg cohort, and thrombocytopenia (100%), neutropenia, anemia, leukopenia (83% each), lymphopenia, and febrile neutropenia (50% each) in the PAN 30 mg cohort.
The peak of thrombocytopenia was generally experienced at the end of the study treatment, but tended to revert to baseline values until the next cycle. Furthermore, all patients in the 30 mg cohort required transfusion around the peak of thrombocytopenia. Of note, the PAN 20 mg + 5-Aza group had fewer grade 3/4 AEs compared with the PAN 30 mg + 5-Aza group. The PAN 30 mg cohort demonstrated that a higher AE incidence than did the PAN 20 mg cohort. Non-hematological AEs were generally grade 1 or 2.
One patient with DLT was observed in each treatment group: lung infection in the PAN 20 mg + 5-Aza group (grade 3 for more than 7 days) and cellulitis (grade 3 for more than 7 days) in the PAN 30 mg + 5-Aza group. Based on the accumulated DLT data and the other reported safety data, 20 or 30 mg of PAN in combination with 75 mg of 5-Aza was considered safe and tolerable. One patient was excluded from the dose-determining set because of early discontinuation as a result of AEs on day 1 of the PK-run-in period.
The AEs that caused a discontinuation of the study drug under combination treatment included pneumonia and pyrexia (n = 1); lung infection (n = 1); thrombocytopenia (n = 1); and anemia, leukopenia, lymphopenia, neutropenia, and thrombocytopenia (n = 1) (all suspected). No death was reported during the study treatment or within 30 days after discontinuation of the study treatment. Two patients in the PAN 20 mg cohort had at least one SAE, including pneumonia (suspected, n = 1), thrombocytopenia (suspected, n = 1), lung infection (suspected), and supraventricular tachycardia (not suspected) (n = 1).
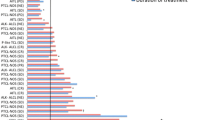
PK evaluation
Drug plasma concentrations up to 48 h after dosing during the PK run-in are shown in Fig. 2. The PAN plasma concentration rapidly reached a peak with T max (median) of 2.0 and 1.5 h in the PAN 20 and 30 mg cohorts, respectively, and then decreased with a T 1/2 (geometric mean) of 12.1 and 13.2 h at each dose. Higher plasma PAN levels were observed in the PAN dose-escalation group (30 mg) compared with the PAN 20 mg group (Table 5).
Plasma concentrations (geometric mean and range) for PAN alone and in combination with 5-Aza after 48 h of dosing were 0.26 (0.10–0.62) and 0.61 (0.39–1.35) in the PAN 20 and 30 mg cohorts, respectively; for PAN + 5-Aza, at the same timepoint, plasma concentrations were 0.39 (0.20–0.74) and 0.72 (0.43–1.05), respectively (Table 5). There was no clear difference between PAN alone and PAN + 5-Aza, suggesting that the combination with 5-Aza did not affect the pharmacokinetics of PAN.
Genotype status and PK
The PK parameters for each patient and their relationships with CYP2D6 and CYP2C19 genotypes were investigated in an exploratory manner. One patient in the PAN 20 mg group who was homozygous wild-type (WT) for CYP2D6 and homozygous *3 mutation for CYP2C19 had the highest C max (33.2 ng/mL) and the longest half-life (17 h); however, the second largest AUC0–48h was found in the 20 mg cohort, compared with another patient (heterozygous *2/WT for CYP2D6 and homozygous WT for CYP2C19) who had C max 17.5 ng/mL and T 1/2 of 13 h. The other patients had homozygous WT or heterozygous genotype with mutations in CYP2D6 (WT/WT, *2/WT, *5/WT) and CYP2C19 (WT/WT, *2/WT, *3/*3) with no clear impact on PK parameters. Thus, there was no clear relationship between the PK parameters of the PAN 20 mg + 5-Aza and PAN 30 mg + 5-Aza groups and the CYP2D6 and CYP2C19 genotypes (Table 6).
Clinical efficacy of PAN + 5-Aza
The overall response (OR) of MDS patients to PAN 20 mg + 5-Aza and PAN 30 mg + 5-Aza groups is shown in Table 7. In the PAN 30 mg cohort (n = 2), one patient with therapy-related MDS achieved CR as the best OR. Another patient with MDS achieved SD as the best OR. In the PAN 20 mg cohort (n = 5), three MDS patients achieved SD, of whom one achieved erythroid and platelet improvements. Regarding CMML patients, all four patients in the PAN 30 mg cohort achieved SD as their best OR. Associations between treatment efficacy and patient background factors such as age and sex could not be investigated because of the small sample size.
Discussion
The objective of this phase Ib, open-label, multi-center, dose-escalation study was to confirm the safety and tolerability of escalating doses of oral PAN (20 and 30 mg) in combination with 5-Aza in 11 Japanese patients with MDS or CMML. A previous clinical trial (ClinicalTrials.gov Identifier: NCT00946647) of Western patients diagnosed with MDS, CMML, or AML indicated that PAN 30 mg/day was the recommended phase II dose when using the BLRM method. The main finding of the current study was that a dose level of 20 or 30 mg of PAN combined with 5-Aza is considered safe and tolerable in Japanese patients with MDS or CMML who are candidates for treatment with 5-Aza. These findings further confirm those of overseas studies in similar populations as reported by Ottmann et al. [16] and Tan et al. [25].
PAN exposure increased with ascending doses as previously reported [26], and combination therapy with 5-Aza did not affect PAN plasma trough concentrations. Alterations in CYP gene polymorphisms have been shown to have potential effects on the PK of drugs in clinical trials [27]. However, CYP2D6 and CYP2C19 have only minor contributions to PAN metabolism as oral clearance (<13%); CYP3A4 is primarily responsible for oxidative metabolism of PAN in the liver. Then, we did not observe any impact of CYP2D6 and CYP2C19 genotypes on PAN PK parameters. Thus, there was no clear relationship between PAN PK parameters and CYP2D6 and CYP2C19 genotypes.
The combination treatment showed no apparent new or unexpected safety signals compared with monotherapy [27] and had an acceptable safety profile. In fact, the most frequent AEs observed with PAN monotherapy were similar [thrombocytopenia (41.5%), fatigue (21%), and neutropenia (21%)] [27] to those observed in the present study [thrombocytopenia (91%), neutropenia (82%), decreased appetite (82%)]. Our findings in Japanese patients are also consistent with data obtained in other countries [25].
The peak of thrombocytopenia, a frequently reported grade 3/4 AE, was generally experienced at the end of the study treatment. However, thrombocytopenia tended to revert to baseline values after ending treatment. In addition, a patient discontinued early during the PAN PK run-in phase because of AEs. Altogether, these findings emphasize the importance of close clinical monitoring early on and during the entire treatment cycles of patients receiving such a treatment combination to properly identify and manage AEs.
Treatment options are limited for elderly patients with MDS, CMML, or AML [25]. Alternative therapies for these patients are currently being studied, mainly in the form of combinations with 5-Aza, and show various levels of activity for these conditions [28,29,30,31]. However, a recent study concluded that combining 5-Aza with the HDAC inhibitor entinostat resulted in excessive treatment toxicity without adding any supplemental benefits or yielding improved outcomes; thus, such a treatment combination is not recommended [32]. Furthermore, a National Institute for Health and Care Excellence Single Technology Appraisal did not recommend 5-Aza alone as treatment for AML [33]. In light of such recent findings, our study results, in terms of safety, tolerability, and efficacy of the combination of oral PAN (20 and 30 mg) with 5-Aza, are promising and should be explored further.
In summary, we conclude that 20 or 30 mg PAN combined with 5-Aza is safe and tolerable in adult Japanese patients with CMML or MDS, and report no new AEs for the combination. The 30 mg PAN cohort reported higher grade AEs, which were more commonly associated with hematological events, than did the 20 mg cohort, although this difference was not statistically significant. The combination treatment of PAN with 5-Aza did not alter PAN plasma levels, but showed some preliminary anti-leukemic activities in two Japanese patients of the targeted patient population. The small number of patients in our cohort is the main limitation of this study; therefore, findings should be validated in a larger group of patients.
References
Catenacci DV, Schiller GJ. Myelodysplasic syndromes: a comprehensive review. Blood Rev. 2005;19:301–19.
Cogle CR, Craig BM, Rollison DE, List AF. Incidence of the myelodysplastic syndromes using a novel claims-based algorithm: high number of uncaptured cases by cancer registries. Blood. 2011;117:7121–5.
Goldberg SL, Chen E, Corral M, Guo A, Mody-Patel N, Pecora AL, et al. Incidence and clinical complications of myelodysplastic syndromes among United States Medicare beneficiaries. J Clin Oncol. 2010;28:2847–52.
Chihara D, Ito H, Katanoda K, Shibata A, Matsuda T, Sobue T, et al. Incidence of myelodysplastic syndrome in Japan. J Epidemiol. 2014;24:469–73.
Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia. 2008;22:14–22.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:937–51.
Walter MJ, Shen D, Ding L, Shao J, Koboldt DC, Chen K, et al. Clonal architecture of secondary acute myeloid leukemia. N Engl J Med. 2012;366:1090–8.
Silverman LR, McKenzie DR, Peterson BL, Holland JF, Backstrom JT, Beach CL, et al. Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol. 2006;24:3895–903.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10:223–32.
Moe-Behrens GH, Pandolfi PP. Targeting aberrant transcriptional repression in acute myeloid leukemia. Rev Clin Exp Hematol. 2003;7:139–59.
Cameron EE, Bachman KE, Myohanen S, Herman JG, Baylin SB. Synergy of demethylation and histone deacetylase inhibition in the re-expression of genes silenced in cancer. Nat Genet. 1999;21:103–7.
Zhu WG, Otterson GA. The interaction of histone deacetylase inhibitors and DNA methyltransferase inhibitors in the treatment of human cancer cells. Curr Med Chem Anticancer Agents. 2003;3:187–99.
Griffiths EA, Gore SD. DNA methyltransferase and histone deacetylase inhibitors in the treatment of myelodysplastic syndromes. Semin Hematol. 2008;45:23–30.
Khot A, Dickinson M, Prince HM. Panobinostat in lymphoid and myeloid malignancies. Expert Opin Investig Drugs. 2013;22:1211–23.
Dimicoli S, Jabbour E, Borthakur G, Kadia T, Estrov Z, Yang H, et al. Phase II study of the histone deacetylase inhibitor panobinostat (LBH589) in patients with low or intermediate-1 risk myelodysplastic syndrome. Am J Hematol. 2012;87:127–9.
Ottmann OG, DeAngelo DJ, Garcia-Manero G, Lübbert M, Jillella A, Sekeres MA et al. Determination of a phase II dose of panobinostat in combination with 5-azacitidine in patients with myelodysplastic syndromes, chronic myelomonocytic leukemia, or acute myeloid leukemia. American Society of Hematology (ASH)—annual meeting 2011, Abs # 459. https://ash.confex.com/ash/2011/webprogram/Paper37915.html. Accessed 19 Jan 2016.
Platzbecker U, Al-Ali HK, Gattermann N, Haase D, Janzen V, Krauter J, et al. Phase 2 study of oral panobinostat (LBH589) with or without erythropoietin in heavily transfusion-dependent IPSS low or int-1 MDS patients. Leukemia. 2014;28:696–8.
Luszczek W, Cheriyath V, Mekhail TM, Borden EC. Combinations of DNA methyltransferase and histone deacetylase inhibitors induce DNA damage in small cell lung cancer cells: correlation of resistance with IFN-stimulated gene expression. Mol Cancer Ther. 2010;9:2309–21.
Govindaraj C, Tan P, Walker P, Wei A, Spencer A, Plebanski M. Reducing TNF receptor 2+ regulatory T cells via the combined action of azacitidine and the HDAC inhibitor, panobinostat for clinical benefit in acute myeloid leukemia patients. Clin Cancer Res. 2014;20:724–35.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Fukutomi A, Hatake K, Matsui K, Sakajiri S, Hirashima T, Tanii H, et al. A phase I study of oral panobinostat (LBH589) in Japanese patients with advanced solid tumors. Invest New Drugs. 2012;30:1096–106.
Babb J, Rogatko A, Zacks S. Cancer phase I clinical trials: efficient dose escalation with overdose control. Stat Med. 1998;17:1103–20.
Neuenschwander B, Branson M, Gsponer T. Critical aspects of the Bayesian approach to phase I cancer trials. Stat Med. 2008;27:2420–39.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108:419–25.
Tan P, Wei A, Mithraprabhu S, Cummings N, Liu HB, Perugini M, et al. Dual epigenetic targeting with panobinostat and azacitidine in acute myeloid leukemia and high-risk myelodysplastic syndrome. Blood Cancer J. 2014;4:e170.
Ingelman-Sundberg M, Sim SC, Gomez A, Rodriguez-Antona C. Influence of cytochrome P450 polymorphisms on drug therapies: pharmacogenetic, pharmacoepigenetic and clinical aspects. Pharmacol Ther. 2007;116:496–526.
DeAngelo DJ, Spencer A, Bhalla KN, Prince HM, Fischer T, Kindler T, et al. Phase Ia/II, two-arm, open-label, dose-escalation study of oral panobinostat administered via two dosing schedules in patients with advanced hematologic malignancies. Leukemia. 2013;27:1628–36.
Almeida A, Fenaux P, List AF, Raza A, Platzbecker U, Santini V. Recent advances in the treatment of lower-risk non-del(5q) myelodysplastic syndromes (MDS). Leuk Res. 2017;52:50–7.
Prebet T, Sun Z, Ketterling RP, Zeidan A, Greenberg P, Herman J, et al. Azacitidine with or without Entinostat for the treatment of therapy-related myeloid neoplasm: further results of the E1905 North American Leukemia Intergroup study. Br J Haematol. 2016;172:384–91.
Tan P, Soo Tiong I, Fleming S, Pomilio G, Cummings N, Droogleever M, et al. The mTOR inhibitor everolimus in combination with azacitidine in patients with relapsed/refractory acute myeloid leukemia: a phase Ib/II study. Oncotarget. 2016;. doi:10.18632/oncotarget.13699.
Schneider BJ, Shah MA, Klute K, Ocean A, Popa E, Altorki NK, et al. Phase I study of epigenetic priming with azacitidine prior to standard neoadjuvant chemotherapy for patients with resectable gastric and esophageal adenocarcinoma. Clin Cancer Res. 2017;23:2673–80.
Morita S, Oizumi S, Minami H, Kitagawa K, Komatsu Y, Fujiwara Y, et al. Phase I dose-escalating study of panobinostat (LBH589) administered intravenously to Japanese patients with advanced solid tumors. Investig New Drugs. 2012;30:1950–7.
Tikhonova IA, Hoyle MW, Snowsill TM, Cooper C, Varley-Campbell JL, Rudin CE, et al. Azacitidine for treating acute myeloid leukaemia with more than 30% bone marrow blasts: an evidence review group perspective of a National Institute for Health and Care Excellence single technology appraisal. Pharmacoeconomics. 2017;35:363–73.
Acknowledgements
This study was supported by an independent data monitoring committee comprising three physicians: Dr. Yasushi Miyazaki of Nagasaki University, Dr. Keiya Ozawa of Jichi Medical University (currently of the Institute of Medical Science, The University of Tokyo), and Dr. Tomoki Naoe of Nagoya Medical Center. A medical expert consultancy agreement was made with Dr. Masamitsu Yanada of Fujita Health University. The authors thank J. Ludovic Croxford, Ph.D., of Edanz Medical Writing, on behalf of Springer Healthcare Communications, for providing medical writing support. This assistance was funded by Novartis Pharmaceuticals Japan.
Conflict of interest
YK received research funding from Novartis during the conduct of the study. FS, MY, FM, and TT are employees of Novartis. HM reports grants from Novartis during the conduct of the study; as well as grants from Fuji Film RI Pharma, AstraZeneca, Yakult Honsha, Berhringer Ingelheim, Astellas, Merck Serono, Sanofi, MSD, Nihon Shinyaku, Teijin Pharma, and Dainippon Sumitomo; grants and personal fees from Taisho Toyama Pharmaceutical, Novartis, Eisai, Kyowa Hakko Kirin, Chugai, Bristol Myers Squibb, Taiho, Daiichi-Sankyo, Ono, Pfizer, Eli Lilly, Takeda Pharmaceutical, and Asahi Kasei Pharma, and personal fees from Bayer, Kowa, Nippon Chemiphar, and Mochida Pharmaceutical, outside the submitted work. MO reports grants from SymBio and Celltrion and personal fees from Meiji Seika Pharma, Mundipharma, Celltrion, AstraZeneca, Takeda, Jansen Pharma, and Celgene, outside the submitted work. The remaining authors declare that they have no conflicts of interest. This industry-led study was sponsored by Novartis, who also supplied the study drugs.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kobayashi, Y., Munakata, W., Ogura, M. et al. Phase I study of panobinostat and 5-azacitidine in Japanese patients with myelodysplastic syndrome or chronic myelomonocytic leukemia. Int J Hematol 107, 83–91 (2018). https://doi.org/10.1007/s12185-017-2327-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-017-2327-9