Abstract
We performed a phase 1 study to evaluate the safety and feasibility of bortezomib (BOR) with melphalan and dexamethasone (BMD) in patients with light chain amyloidosis (AL) without severe cardiac failure. Patients received BOR on a twice-weekly schedule (days 1, 4, 8, and 11 of 28-day treatment cycles) at planned doses of 1.0 (dose level 1) and 1.3 (dose level 2) mg/m2 in combination with melphalan 8 mg/m2 on days 1–4 and dexamethasone 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12. Dose-limiting toxicity (DLT) was evaluated at the end of cycle one, and treatment was continued for four cycles. Six patients were enrolled at dose level 1, and one showed DLT (grade 3: herpes zoster). Further 3 patients were enrolled at dose level 2, and none experienced DLT. Thus, the maximum tolerated dose was defined as BOR doses of 1.3 mg/m2 for the twice-weekly schedule. A total of 32 cycles of BMD therapy were given, and the most common hematologic toxicity was thrombocytopenia (47 %). Peripheral neuropathy was the most common non-hematologic toxicity (16 %). We demonstrated that BMD is safe and tolerable for Japanese AL patients without severe cardiac damage.
Clinical trial registration
UMIN000006604.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Light chain amyloidosis (AL) is the most common form of amyloidosis and it is characterized by immunoglobulin light chain-derived amyloid deposits that are associated with the expansion of clonal plasma cells [1]. The median overall survival from diagnosis is approximately 3 years, but the prognosis of patients with clinically overt cardiac involvement is poor, with a median survival of less than 6 months [2]. The aim of treatment for AL is to suppress production of the insoluble amyloidogenic immunoglobulin light chain fragments, with the goal of restoring organ function [3, 4]. The depth of the hematologic response, particularly the achievement of a complete response (CR), has been shown to be associated with improved organ function [5] in AL patients, as well as improved overall survival [6, 7].
Intensive therapy with high-dose melphalan and stem cell transplant is highly effective for AL, but many patients are not eligible for this treatment modality because of their age, poor performance status, and multiple organ involvement or extensive cardiac involvement [5, 7, 8].
Oral melphalan plus dexamethasone (MD) has been the standard-of-care in a non-transplant setting, with a hematologic response rate of 67 % and a time to hematologic response of 4.5 months [7, 9–11]. Therefore, recent investigations have explored the use of novel agents, including thalidomide, lenalidomide, and bortezomib, as treatment for AL [12–19].
The proteasome inhibitor bortezomib (BOR) is highly active in multiple myeloma patients [20, 21]. The pathogenic plasma cells in AL amyloidosis produce light chains prone to misfolding and so they may be particularly sensitive to BOR-induced proteasome inhibition [22]. Indeed, a case series study suggested BOR ± dexamethasone is active in relapsed AL patients, with a 72 % hematologic response rate, including 25 % CRs, reported in a multicenter retrospective analysis of 76 relapsed and 18 untreated AL patients. The median time to hematologic response was 52, 28 days for newly diagnosed patients, and 60 days for pretreated patients [18].
Based on these observations, we performed a phase 1 study to evaluate the safety and feasibility of BOR in combination with melphalan plus dexamethasone (BMD).
Methods
Patients
Patients were enrolled in this phase 1, single-arm, open-label study (UMIN000006604) in eight centers between October 2011 and May 2014.
The present study included previously treated (less than three courses) patients with biopsy-confirmed AL aged between 20 and 65 years. Other criteria included an absolute neutrophil count ⩾ 2.0 × 109/L, a platelet count ≥75 × 109/L, hemoglobin ≥8 g/dL, an adequate liver function (aspartate aminotransferase and alanine aminotransferase ⩽ 2.5 × the upper limit of normal and total bilirubin ≤2 mg/dL), serum creatinine ≤2.5 mg/dL, no severe comorbidities including respiratory and neurologic disease, or severe diabetes mellitus, and not carriers of hepatitis, HTLV-1, or HIV virus.
Patients were excluded if they had received prior treatment with BOR, New York Heart Association (NYHA) classification III or IV, ejection fraction <40 %, continuous pleural effusion, supine systolic blood pressure less than 90 mmHg, N-terminal pro-brain natriuretic peptide (NT-proBNP) >332 pg/mL (BNP >50 pg/mL), saturation of oxygen level <95 %, symptomatic orthostatic hypotension, grade 3 or higher diarrhea not controllable with medication, grade 2 or higher neuropathy or painful peripheral neuropathy, pulmonary complications such as interstitial pneumonitis, pulmonary fibrosis, pulmonary amyloidosis, and computed tomography abnormality, KL-6 >500 U/mL, SP-D >110 ng/mL, SP-A >43.8 ng/mL, or were pregnant.
All patients participating in the study provided written informed consent. The study was approved by the institutional review board of participating sites and was conducted in accordance with the Declaration of Helsinki, International Conference on Harmonization, and Good Clinical Practice Guideline.
Study design
Eligible patients received BOR intravenously on a twice-weekly schedule (days 1, 4, 8, and 11 of 28-day treatment cycles) at planned doses of 1.0 (dose level 1) and 1.3 (dose level 2) mg/m2 in combination with melphalan 8 mg/m2 on days 1–4 and dexamethasone 20 mg on days 1, 2, 4, 5, 8, 9, 11, and 12 every 28 days. Treatment was continued for 4 cycles.
The primary objective of the study was the determination of the maximum tolerated dose (MTD) of BMD, and the secondary objective was to evaluate the efficacy of this combination.
Dose-limiting toxicity
The MTD was evaluated based on the dose-limiting toxicity (DLT) observed through the end of cycle 1 (day 28).
A standard 3 + 3 design was followed. If no DLT was encountered in the first 3 patients at dose level 1, 3 patients were enrolled at dose level 2. If >1 of the 3 patients experienced DLT, then MTD was considered to have been exceeded and the study was discontinued. If 1 of the 3 patients experienced DLT, 3 more patients were enrolled at dose level 1 (total: 6 patients). If no more patients experienced DLT (1 of 6), 3 patients were enrolled at dose level 2. In case of ⩾ 2 of 6 patients experiencing DLT, MTD was considered to have been exceeded.
The severity of adverse events (AE) was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events Version 3.0. DLT was defined as Grade 4 hematologic toxicity, or Grade 3 or higher non-hematologic toxicity.
Efficacy assessments
The serum-free light chain (FLC) levels were assessed before and after 4 cycles of BMD therapy and at 6 months after BMD therapy. Hematologic and organ responses were determined at 6 months of BMD therapy by assessment according to established consensus criteria [23]. Hematologic responses were based on serum and urine M-protein electrophoresis, immunoelectrophoresis (IEP), immunofixation electrophoresis (IFE), FLC analysis, and bone marrow aspirate. Organ responses were based on the multiple procedures used at screening to determine end-organ involvement.
Results
Patients’ characteristics
A total of nine patients with relapsed or refractory AL were enrolled in this phase 1 study. Patients’ characteristics are shown in Table 1. They were 6 males and 3 females, with a median age of 55 years (range, 44–65 years). Seven patients (78 %) showed involvement of 2 or more organs, and the most involved organs were the kidney (78 %) and gastrointestinal tract (78 %) followed by the liver (33 %) and heart (11 %). Seven (78 %) had lambda light chain and the other 2 had kappa light chain. Overall, 6 (67 %) patients had received prior melphalan, and 6 (67 %) had previously undergone intensive therapy with high-dose therapy and stem cell transplantation. Five of these 6 patients responded to SCT with response duration of 31 (3–60) months. At the time of enrollment, 5 patients were refractory to previous therapies, and a median time from previous therapy to BMD therapy was 3 (1–107) months.
DLT and determination of MTD
The first 6 patients received BOR 1.0 mg/m2 (dose level 1) and the remaining 3 received BOR 1.3 mg/m2 (dose level 2). One of the first 3 patients enrolled at dose level 1 experienced DLT (Grade 3 herpes zoster) during cycle 1 (Table 2). The AE was considered BOR-related and led to treatment discontinuation. Herpes zoster was reported to occur in 13 % of patients during BOR therapy if no prophylactic antiviral therapy was conducted [24, 25]; therefore, the protocol was amended to do prophylactic antiviral therapy for subsequently enrolled patients. Consequently, a further 3 patients were enrolled in this cohort (patients 4–6). In patient 6, BOR was given subcutaneously instead of intravenously. Recently, BOR has been routinely given subcutaneously, because a randomized phase 3 study of multiple myeloma demonstrated that rates of adverse events such as peripheral neuropathy were lower with subcutaneous administration as compared with intravenous administration, while the efficacy was comparable between these two administration routes [26]. The Efficacy and Safety Assessment Committee advised us to include this patient in study cohort because the subcutaneous administration of BOR is safer and widely used in daily clinical practice. Thus, the protocol was amended so that BOR was given subcutaneously on further enrollment. None experienced DLT. Then, a further 3 patients were enrolled at dose level 2 (BOR 1.3 mg/m2), and none experienced DLT.
Thus, the MTD was defined as maximum doses of 1.3 mg/m2 for the twice-weekly schedule.
Adverse events
All patients except 2 experienced at least 1 AE during cycle 1 (Table 2). Hematologic toxicities, including grade 3 leukopenia, neutropenia, lymphopenia, or thrombocytopenia, were reported in 7 of 9 patients. The non-hematological toxicities reported were grade 1 peripheral neuropathy and grade 2 eruptions.
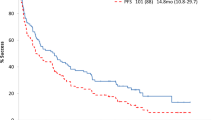
A total of 32 cycles of BMD therapy were given in this phase 1 study (Table 3). The median number of cycles was 4, and 7 of 9 patients received 4 cycles. Treatment was discontinued due to AE in cycle 1 in patient 3 (herpes zoster) and cycle 3 in patient 7 (peripheral neuropathy). The most common hematologic toxicities included thrombocytopenia, leukopenia, lymphopenia, and anemia. Peripheral neuropathy was observed in 5 events (16 %), including grade 3 in one event, and was the most common non-hematologic toxicity.
No death was reported during the study period.
Efficacy assessments
The changes of free light chains, and hematologic and organ responses were secondary endpoints, shown in Table 4. Before BMD therapy, involved FLC was increased in 7 of 9 patients and the κ/λ ratio was abnormal in 3 patients. After BMD therapy, involved FLC was high in only 3 patients and the κ/λ ratio was abnormal in 2 patients. Unfortunately, IFE was performed in only 3 of 9 patients (patients 5, 6 and 7); therefore, a hematologic response was defined as CR in 2 with a partial response (PR) in 5 patients, with a response rate of 78 %. Three of 4 patients defined as showing PR were negative for IEP, but IFE was not done.
An organ response was observed after 6 months of BMD therapy in 2 patients: one showed a liver response and the other showed a renal response.
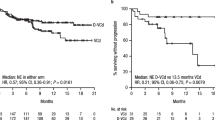
All patients were alive at a median follow-up period of 27 months (14–43).
Discussion
In this phase 1 study, we demonstrated that BMD therapy is safe and tolerable for Japanese AL patients without severe cardiac damage.
MD has been considered the standard-of-care for the treatment of AL, with a median survival of about 60 months [10]. However, the median time to response by MD is 4.5 months, and MD cannot overcome the poor prognosis of patients with severe cardiac involvement [9, 27].
BOR is a reversible proteasome inhibitor, which has significant activity in patients with multiple myeloma [20, 21]. Plasma cells that produce amyloidogenic light chains accumulate unfolded toxic light chains that lead to unprecedented increases in endoplasmic stress and a strive-to survive response, which are largely dependent on the proteasome function [22]. Thus, clonal plasma cells in AL are considered to be more sensitive to proteasome inhibition than clonal plasma cells in myeloma [22]. Several studies have shown hematological response rates in excess of 80 % with BOR in patients with relapsed or refractory disease [16, 17]. Hematologic responses were markedly rapid in some patients, although one-third developed grade 3 toxicity or needed to discontinue BOR treatment [16, 17]. A collaborative European study from 33 centers involving 94 patients (81 % of whom had received prior therapy) showed a hematologic response rate of 71 %, a CR rate of 25 %, and a cardiac response in 29 % [18]. A prospective trial showed that single-agent BOR is highly and rapidly effective [28–30]. In addition, recent reports demonstrated that a triplet regimen containing BOR with cyclophosphamide and dexamethasone is highly effective for AL [31–34]. Based on these results, we evaluated the safety and efficacy of BMD in Japanese patients with AL amyloidosis.
BOR has been reported to have adverse cardiac effects, and there are a few cardiovascular events associated with BOR use in patients with multiple myeloma [35–37]. Therefore, we excluded patients with congestive heart failure including NYHA classification III or IV, ejection fraction <40 %, and NT-proBNP ≥332 pg/mL (BNP ≥50 pg/mL). The threshold value of NT-proBNP 332 pg/mL provides a hazard ratio of 2.05 for mortality in patients with AL amyloidosis and was used as a prognostic factor in combination with cardiac troponin T for staging system for patients with AL amyloidosis [38]. Recently, a retrospective analysis of 73 consecutive AL patients treated with BOR-based regimens demonstrated severe adverse events (grade 3 or higher) in 45 % of patients, of which the most commonly observed was cardiac [19]. Another retrospective analysis of 19 patients treated with BOR, melphalan, and prednisolone also demonstrated 2 patients with decompensated heart failure with fluid overload [39].
At dose level 1, only one of 6 patients demonstrated Grade 3 herpes zoster. However, this adverse event was reported to often be observed during the administration of BOR in patients with multiple myeloma and could be protective using the prophylactic administration of antiviral agent acyclovir or valacyclovir [24, 25]. Thus, we amended the protocol to administer prophylactic valacyclovir 500 mg daily during BOR treatment.
During this study, the subcutaneous administration of BOR was reported to be less neurotoxic compared with intravenous administration but with equal clinical efficacy in multiple myeloma [26]. Therefore, the protocol was amended to administer BOR subcutaneously instead of intravenously. At dose level 2, no DLT was observed. These observations suggested that the subcutaneous administration of BOR twice weekly in combination of MD is safe and tolerable in Japanese AL patients.
Efficacy assessment of BMD therapy was not a goal of this study because this was a small phase 1 study, but a hematologic response of 78 % including a CR rate of 22 % is promising. Unfortunately, IFE was not done in 5 PR patients, but all of these had a normal FLC κ/λ ratio and 3 of these were IEP-negative. Strict evaluation is necessary regarding whether or not these patients achieved CR. In this study, high-risk patients such as those with severe cardiac damage were excluded; therefore, the response rate is considered to be high.
Recently, a matched case–control study of 87 patients treated with BMD compared with that of 87 controls treated with MD demonstrated a higher CR rate observed with BMD (42 vs. 19 %, respectively), but this was not associated with improved overall survival [40]. However, a significant survival advantage for BMD was observed in patients without severe (NYHA class III or IV) heart failure and with NT-proBNP <8500 pg/mL. Patients treated with full-dose dexamethasone had similar response rates and survival regardless of whether they received BOR or not. Intermediate-risk patients who are not fit enough to receive high-dose dexamethasone are likely to gain the greatest advantage from the addition of BOR to MD.
There are still questions regarding the added value of incorporating BOR into first-line therapy among patients with AL [41]. The ongoing phase III randomized and stratified clinical trial comparing BMD with MD (NCT01277016) will clarify the optimal setting for employing the combination of BMD in AL amyloidosis. BOR-containing regimens appear to be an attractive option, and starting with lower doses and a weekly subcutaneous administration may promote better tolerance in many AL patients.
References
Falk RH, Comenzo RL, Skinner M. The systemic amyloidosis. N Engl J Med. 1997;337:898–909.
Dispenzieri A, Gertz MA, Kyle RA, Lacy MQ, Burritt MF, Therneau TM, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22:3751–7.
Guidelines Working Group of UK Myeloma Forum, British Commitee for Standards in Haematology, British Society for Haematology. Guidelines on the diagnosis and management of AL amyloidosis. Br J Haematol. 2004;125:681–700.
Merlini G, Seldin DC, Gertz MA. Amyloidosis: pathogenesis and new therapeutic options. J Clin Oncol. 2012;29:1924–33.
Skinner M, Sanchorawala V, Seldin DC, Dember LM, Falk RH, Berk JL, et al. High-dose melphalan and autologous stem-cell transplantation in patients with AL amyloidosis: an 8-year study. Ann Intern Med. 2004;140:85–93.
Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Leung N, et al. Effect of hematologic response on outcome of patients undergoing transplantation for primary amyloidosis: importance of achieving a complete response. Haematologica. 2007;92:1415–8.
Jaccard A, Moreau P, Leblond V, Leleu X, Benboubker L, Hermine O, et al. High-dose melphalan versus melphalan plus dexamethasone for AL amyloidosis. N Engl J Med. 2007;357:1083–93.
Comenzo RL, Gertz MA. Autologous stem cell transplantation for primary systemic amyloidosis. Blood. 2002;99:4276–82.
Palladini G, Perfetti V, Obici L, Caccialanza R, Semino A, Adami F, et al. Association of melphalan and high-dose dexamethasone is effective and well tolerated in patients with AL (primary) amyloidosis who are ineligible for stem cell transplantation. Blood. 2004;103:2936–8.
Palladini G, Russo P, Nuvolone M, Lavatelli F, Perfetti V, Obici L, et al. Treatment with oral melphalan plus dexamethasone produces long-term remissions in AL amyloidosis. Blood. 2007;110:787–8.
Palladini G, Milani P, Foli A, Obici L, Lavatelli F, Nuvolone M, et al. Oral melphalan and dexamethasone grants extended survival with minimal toxicity in AL amyloidosis: long-term results of a risk-adapted approach. Haematologica. 2014;99:743–50.
Palladini G, Perfetti V, Perlini S, Obici L, Lavatelli F, Caccialanza R, et al. The combination of thalidomide and intermediate-dose dexamethasone is an effective but toxic treatment for patients with primary amyloidosis (AL). Blood. 2005;105:2949–51.
Wechalekar AD, Goodman HJ, Lachmann HJ, Offer M, Hawkins PN, Gillmore JD. Safety and efficacy of risk adapted cyclophosphamide, thalidomide, and dexamethasone in systemic AL amyloidosis. Blood. 2007;109:457–64.
Dispenzieri A, Lacy MQ, Zeldenrust SR, Hayman SR, Kumar SK, Geyer SM, et al. The activity of lenalidomide with or without dexamethasone in patients with primary systemic amyloidosis. Blood. 2007;109:465–70.
Palladini G, Russo P, Foli A, Milani P, Lavatelli F, Obici L, et al. Salvage therapy with lenalidomide and dexamethasone in patients with advanced AL amyloidosis refractory to melphalan, bortezomib, and thalidomide. Ann Hematol. 2012;91:89–92.
Kastritis E, Anagnostopoulos A, Roussou M, Toumanidis S, Pamboukas C, Migkou M, et al. Treatment of light chain (AL) amyloidosis with the combination of bortezomib and dexamethasone. Haematologica. 2007;92:1351–8.
Wechalekar AD, Lachmann HJ, Offer M, Hawkins PN, Gillmore JD. Efficacy of bortezomib in systemic AL amyloidosis with relapsed/refractory clonal disease. Haematologica. 2008;93:295–8.
Kastritis E, Wechalekar A, Dimopoulos M, Merlini G, Hawkins P, Perfetti V, et al. Bortezomib with or without dexamethasone in primary systemic (light chain) amyloidosis. J Clin Oncol. 2010;28:1031–7.
Gatt ME, Hardan I, Chubar E, Suriu C, Tadmor T, Shevetz O, et al. Israeli MM study group. Outcomes of light-chain amyloidosis patients treated with first-line bortezomib: a collaborative retrospective multicenter assessment. Eur J Haematol. 2015 Mar 31, doi.1111/ejh.12558.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352:2487–98.
San Miguel J, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M, et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med. 2008;359:906–17.
Sita R, Palladini G, Merlini G. Bortezomib in the treatment of AL amyloidosis: targeted therapy? Haematologica. 2007;92:1302–7.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18–22 April 2004. Am J Hematol. 2005;79:319–28.
Chanan-Khan A, Sonneveld P, Schuster MW, Stadtmauer EA, Facon T, Harousseau JL, et al. Analysis of herpes zoster events among bortezomib-treated patients in the phase III APEX study. J Clin Oncol. 2008;26:4784–90.
Vickrey E, Allen S, Mehta J, Singhal S. Acyclovir to prevent reactivation of varicella zoster virus (herpes zoster) in multiple myeloma patients receiving bortezomib therapy. Cancer. 2009;115:229–32.
Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M, et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol. 2011;12:431–40.
Dietrich S, Schönland S, Benner A, Bochtler T, Kristen A, Beimler J, et al. Treatment with intravenous melphalan and dexamethasone is not able to overcome the poor prognosis of patients with newly diagnosed systemic light chain amyloidosis and severe cardiac involvement. Blood. 2010;116:522–8.
Reece D, Sanchorawala V, Hegenbart U, Merlini G, Palladini G, Fermand J, et al. Weekly and twice-weekly bortezomib in patients with systemic AL amyloidosis: results of a phase 1 dose-escalation study. Blood. 2009;114:1489–97.
Reece DE, Hegenbart U, Sanchorawala V, Merlini G, Palladini G, Bladé J, et al. Efficacy and safety of once-weekly and twice-weekly bortezomib in patients with relapsed systemic AL amyloidosis: results of a phase 1/2 study. Blood. 2011;118:865–73.
Dubrey SW, Reece DE, Sanchorawala V, Hegenbart U, Merlini G, Palladini G, et al. Bortezomib in a phase 1 trial for patients with relapsed AL amyloidosis: cardiac responses and overall effects. QJM. 2011;104:957–70.
Mikhael JR, Schuster SR, Jimenez-Zepeda VH, Bello N, Spong J, Reeder CB, et al. Cyclophosphamide-bortezomib-dexamethasone (CyBorD) produces rapid and complete hematologic response in patients with AL amyloidosis. Blood. 2012;119:4391–4.
Venner CP, Lane T, Foard D, Rannigan L, Gibbs SD, Pinney JH, et al. Cyclophosphamide, bortezomib, and dexamethasone therapy in AL amyloidosis is associated with high clonal response rates and prolonged progression-free survival. Blood. 2012;119:4387–90.
Venner CP, Gillmore JD, Sachchithanantham S, Mahmood S, Lane T, Foard D, et al. A matched comparison of cyclophosphamide, bortezomib and dexamethasone (CVD) versus risk-adapted cyclophosphamide, thalidomide and dexamethasone (CTD) in AL amyloidosis. Leukemia. 2014;28:2304–10.
Kikukawa Y, Yuki H, Hirata S, Ide K, Nakata H, Miyakawa T, et al. Combined use of bortezomib, cyclophosphamide, and dexamethasone induces favorable hematological and organ responses in Japanese patients with amyloid light-chain amyloidosis: A single-institution retrospective study. Int J Hematol. 2015;101:133–9.
Enrico O, Gabriele B, Nadia C, Sara G, Daniele V, Giulia C, et al. Unexpected cardiotoxicity in haematological bortezomib treated patients. Br J Haematol. 2007;138:396–7.
Hacihanefioglu A, Tarkun P, Gonullu E. Acute severe cardiac failure in a myeloma patient due to proteasome inhibitor bortezomib. Int J Hematol. 2008;88:219–22.
Bockorny M, Chakravarty S, Schulman P, Bockorny B, Bona R. Severe heart failure after bortezomib treatment in a patient with multiple myeloma: a case report and review of the literature. Acta Haematol. 2012;128:244–7.
Dispenzieri A, Gertz MA, Kyle RA, Lacy MQ, Burritt MF, Therneau TM, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22:3751–7.
Lee JY, Lim SH, Kim SJ, Lee GY, Lee JE, Choi JO, et al. Bortezomib, melphalan, and prednisolone combination chemotherapy for newly diagnosed light chain (AL) amyloidosis. Amyloid. 2014;21:261–6.
Palladini G, Milani P, Foli A, Vidus Rosin M, Basset M, Lavatelli F, et al. Melphalan and dexamethasone with or without bortezomib in newly diagnosed AL amyloidosis: a matched case–control study on 174 patients. Leukemia. 2014;28:2311–6.
Dispenzieri A. Still no certainty about the role of upfront bortezomib among patients with AL amyloidosis. Leukemia. 2014;28:2273–5.
Acknowledgments
This study was supported by Grants-in-Aid for Intractable Diseases from the Ministry of Health, Labour and Welfare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors would like to thank Janssen Pharmaceutical KK, Japan, for providing bortezomib for this study. The authors have no conflict of interest to declare.
About this article
Cite this article
Shimazaki, C., Fuchida, Si., Suzuki, K. et al. Phase 1 study of bortezomib in combination with melphalan and dexamethasone in Japanese patients with relapsed AL amyloidosis. Int J Hematol 103, 79–85 (2016). https://doi.org/10.1007/s12185-015-1901-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1901-2