Abstract
Primary immune thrombocytopenia (ITP) is an autoimmune disease mediated by the production of auto-antibody against platelets. Rituximab, an anti-CD20 antibody, is reported to be useful for treatment of ITP. In Japan, however, robust evidence on this treatment has not been accumulated. Hence, we conducted this open-label phase III clinical trial to confirm the efficacy and safety of rituximab, administered at 375 mg/m2 once per week at weekly intervals for 4 consecutive weeks in Japanese patients with chronic ITP, who had relapsed and were refractory to conventional therapy. The primary endpoint was defined as the percentage of patients with a platelet count above 50 × 109/L at week 24 after the first dose of rituximab, which was 30.8 % of 26 patients (95 % confidence interval 14.3–51.8 %). Although the lower confidence limit of primary endpoint failed to meet the pre-specified threshold of 20 %, the clinical efficacy of rituximab is substantial in consideration of the 2 % response rate in the placebo arm in other clinical studies in patients with chronic ITP. We conclude that rituximab is clinically useful and safe in the treatment of Japanese patients with chronic ITP, achieving the goal of maintaining platelet count and reducing risk of bleeding while minimizing treatment-related toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary immune thrombocytopenia (ITP) is a thrombocytopenia-causing autoimmune disease. Approximately 20,000 patients are suffered from this disease in Japan, and about 3000 new cases occur per year [1]. The causes of decrease in the platelet count are known to be destruction of platelets, to which auto-antibody is attached, in the spleen, and defects of proliferation and maturation of megakaryocyte due to the relative shortage of thrombopoietin (TPO). The major clinical symptoms and signs of ITP are petechiae and mucosal hemorrhage. ITP is classified by duration into newly diagnosed (within 3 months of onset), persistent (3–12 months’ duration) and chronic (12 months or more in duration). Of ITP with onset in adult age, about 90 % of the patients are chronic and its male-to-female ratio is 1:2. Massive hemorrhage is relatively uncommonly seen in chronic ITP, whereas seen in the other types of ITP.
Patients who show no effects on standard therapy and have platelet count ≤30 × 109/L are diagnosed with refractory ITP, and those are about 10 % of total patients with ITP. Such patients have a 4.2-fold higher risk of death than healthy population [2]. In Japan, nearly half of patients with ITP are infected with Helicobacter pylori, and H. pylori eradication therapy is effective for restoring the platelet count in 60 % of patients [3].
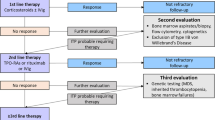
The first-line treatment of standard therapy is corticosteroid administration. Corticosteroid administration can only be discontinued in about 10–20 % of the patients. For most of the patients, the steroid therapy is continued especially in Japan. Splenectomy is chosen as a second-line treatment for patients who fail to respond or have poor tolerability to corticosteroids. A radical cure can be expected from splenectomy in about 70 % of patients, while for the remaining 30 % of patients this surgical intervention makes to be ineffective. Splenectomy has several concerns such as complications in the perioperative phase (mortality rate at 0.1 % and complication rate at 10 %), postoperative depression of immune functions, and relapses in about 20 % of patients [4]. Since it is difficult to predict the efficacy of surgical removal of the spleen in patients with ITP, both patients and physicians tend to avoid splenectomy in Japan, as well as in Europe and the United States. Non-responders to splenectomy die at about 10 % from serious hemorrhage such as cerebral hemorrhage. Therefore, the goal of ITP treatment is to increase the platelet count to ≥30 × 109/L to avoid such fatal bleeding [5, 6].
Immunosuppressants such as azathioprine and cyclosporine, and anticancer agents such as cyclophosphamide and vincristine, in off-label use, are empirically prescribed for patients who are non-responding or ineligible for splenectomy. With these drugs, response rates are as low as about 30 %, and adverse events are rather frequently observed. Recently, thrombopoietin receptor agonists (romiplostim and eltrombopag) have been approved for refractory ITP and showed efficacy in nearly 60 % of patients. However, some concerns arise from these agonists, including offset of drug effect back to baseline level in about 2 weeks after discontinuation of the medication, a high cost of drug expense as high as 2–3 million yen per year, a high incidence of thrombotic complications in some of patients with a certain background, and disease progression to myelofibrosis or acute leukemia after long-term treatment.
Rituximab is a chimeric monoclonal antibody against the CD20 antigen and prepared by recombinant DNA technology. Rituximab was approved in Japan for the treatment of B cell non-Hodgkin’s lymphoma, microscopic polyangiitis (MPA), and granulomatous polyangiitis (GPA; Wegener granulomatosis). In addition to these indications, this drug was approved for the treatment of chronic lymphoid leukemia and rheumatoid arthritis in the United States and Europe. Rituximab specifically eliminates CD20-positive B lymphocytes; therefore, its efficacy for various disorders relevant to B cell abnormalities is anticipated [7, 8]. Recent studies have demonstrated that B cells are involved in the onset and maintenance of autoimmune diseases, and the efficacy of treatment with rituximab has been reported in autoimmune disorders such as systemic lupus erythematosus (SLE), multiple sclerosis, nephrotic syndrome, and thrombotic thrombocytopenic purpura (TTP). Outside of Japan, rituximab is extensively prescribed and accepted as the second-line treatment for refractory ITP [5, 9–11]. A systematic review on the efficacy and safety of rituximab in approximately 300 patients with ITP by Arnold et al. [11] showed that the response rate was 62.5 %, and the time to therapeutic response was 5.5 weeks. A phase II clinical trial of rituximab in 60 patients with refractory ITP in France showed that the response rate was 40 % after 1 year of the treatment [12]. As seen in a number of reports outside Japan, the efficacy and safety of rituximab in patients with refractory ITP have been extensively evaluated and the effectiveness of the drug has been demonstrated.
In Japan, there are several case reports to indicate the efficacy of rituximab in the treatment of refractory ITP, but robust evidence on this treatment has not yet been accumulated such as from clinical studies. Rituximab is then prescribed off-label for rescuing patients with refractory ITP, but the medication cost of rituximab is not reimbursed under the Japanese National Health Insurance program.
Hence, we conducted this open-label phase III clinical trial to confirm the efficacy and safety of rituximab, administered at 375 mg/m2 (body surface area) once a week, at weekly intervals for 4 consecutive weeks in Japanese patients with chronic refractory ITP. This study was implemented in accordance with the International Consensus Guidelines for Diagnosis and Treatment of ITP [10], and the Japanese Guidelines for Treatment of ITP. This study was registered with the Japan Medical Association Center for Clinical Trials (JMACTR; CTR Number: JMA-IIA00070, https://dbcentre3.jmacct.med.or.jp/jmactr/default.aspx?JMACCTID=JMA-IIA00070).
Materials and methods
Patient population
Patients included in this study were: Japanese, aged ≥20 years, and diagnosed with chronic refractory ITP at least 12 months before the enrollment of this study. The definition of the term refractory in this study was as follows: platelet counts ≤30 × 109/L (measured at weeks 4 and 2 before enrollment), ineffective or intolerable for steroids, ineffective or judged as inappropriate by investigators for splenectomy, and ineffective, intolerable or judged as inappropriate by investigators for thrombopoietin receptor agonists.
Study design
This study was an open-label multicenter phase III clinical trial conducted between October 2011 and July 2013 in ten clinical institutions in Japan. The study consisted of screening (4 weeks), treatment (4 weeks), and follow-up periods (20 weeks).
Rituximab was administered at 375 mg/m2 in once a week consecutively for 4 weeks (weeks 0, 1, 2, and 3). To prevent infusion reactions associated with rituximab infusion, patients received pre-medications of oral antipyretic–analgesics, oral antihistamines, and intravenous hydrocortisone at 30 min before each administration of rituximab.
During the study period, the following concomitants or therapies were prohibited: immunoglobulin preparations, drugs which stimulate platelet production, splenectomy, H. pylori eradication therapy, hematopoietic factors, antineoplastics and platelet transfusion.
Efficacy and safety analysis
The primary efficacy endpoint was a response rate: the percentage of patient with the platelet count ≥50 × 109/L at 24 weeks after the first administration of the study drug.
The major secondary efficacy endpoints included the percentage of patients with the platelet count ≥100 × 109/L and who did not have bleeding at week 24, the percentage of patients with the platelet count ≥30 × 109/L and ≥twofold higher than the baseline value and who did not have bleeding at week 24, and the improvement rate of bleeding symptoms [World Health Organization (WHO) bleeding scale]. In addition, the changes of peripheral blood B cells (CD19 and CD20) and T cells (CD3), and changes of serum IgG, IgM, and IgA levels were evaluated as exploratory endpoints. Safety parameters (adverse events and clinical laboratory data) were also assessed.
Statistical considerations
Sample size and its rationale were pre-specified in the study protocol. Response rate in the primary endpoint was assumed to be 50 % based on results of clinical studies [11, 12]. Twenty-four patients were needed to have ≥80 % power to show that the lower limit of 95 % confidence interval (CI) for the response rate is greater than a threshold (20 %). The threshold was determined conservatively taking account of a response rate, 2 % (1/42 patients, 95 % CI 0–12.6 %) in placebo group in the phase III clinical trial of romiplostim in patients with refractory ITP [13]. All enrolled patients were included in the primary efficacy analysis population (full analysis set, FAS). Demographic factors and baseline characteristics were summarized with mean ± standard deviation (SD) or median (interquartile range, IQR) depending on distributions. Exact 95 % CIs for proportions were calculated with the Clopper–Pearson method. Paired proportions were compared with the exact McNemar’s test. For continuous valuables, values at each time point were compared with baseline values by signed rank sum test. Significance level was a two-sided 5 % for all tests. All data were analyzed with SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Ethical considerations
This clinical trial was conducted in compliance with the ethical principles of the Declaration of Helsinki, the Japanese Guidelines for Good Clinical Practice, and other relevant regulatory requirements. The investigator or co-investigator gave a full explanation of the clinical trial to patients prior to participation in the study and, upon confirming that the patients gained a good understanding of the nature of the study, obtained written informed consent for voluntary participation in the study. Prior to conduct of this clinical trial, the institutional review board (IRB) of each participating medical facility reviewed the ethical, scientific, and medical propriety of this clinical trial and approved this study.
Results
Patient characteristics
Written informed consent was obtained from 49 patients in this clinical trial. Of them, 26 patients who met the inclusion criteria were enrolled. All the 26 patients completed a total of four doses of rituximab infusion and were included in the FAS. None of the patients discontinued the study treatment. The following measured values of the platelet count were partially excluded from the FAS: the platelet counts of one patient at week 4 and week 0 when platelet aggregation was seen in the sample of the patient, and the platelet count of other patient at the time when the platelet count was increased due to emergency treatment (high-dose immunoglobulin therapy plus platelet transfusion) at week 2.
Although protocol deviations were seen in 12 patients, none were relevant to patient eligibility or discontinuation criteria. None of these patients were excluded from the efficacy and/or safety analysis, as the deviations in this study were examined at the case-conference meeting and judged not to significantly influence on the evaluation of the study.
Most of the patients with refractory ITP enrolled in this study were female (88.5 %). The mean age was 39.7 ± 13.0 years (Table 1). The median duration of ITP was 5.9 years (IQR 1.9–11.2), and Grade 0, 1, and 2 hemorrhagic symptoms in severity at baseline were 42.3, 53.8, and 3.8 % of patients, respectively. The median platelet count at baseline was 22 × 109/L (IQR 17–24). Of the enrolled patients, 15.4 % had previously received splenectomy and 34.6 % underwent H. pylori eradication. The percentages of patients who had previously received corticosteroids, high-dose immunoglobulin therapy, and thrombopoietin receptor agonists, as prior therapy for ITP, were 69.2, 38.5, and 26.9 %, respectively.
Primary efficacy endpoint
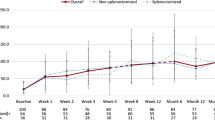
The percentage of patients who had achieved the platelet count ≥50 × 109/L at week 24 was 30.8 % (8/26 patients). The 95 % CI of the response rate was 14.3–51.8 %, and the lower limit of CI did not exceed the threshold of 20 %. However, in comparison with the response rate of 0–2 % in placebo group reported in other clinical studies with a similar target population to this study, it was suggested that the efficacy of rituximab observed in this study is substantial. The number of patients who achieved the platelet count ≥50 × 109/L at each time point for the assessment is shown in Table 2. Box plots of the trajectory of the platelet count over 24 weeks in a subgroup which consists of eight responders is shown in Fig. 1. In these eight responders, mean platelet count reached ≥50 × 109/L at week 4 and continued to increase throughout the follow-up period (Fig. 1).
Box plots of platelet counts of the eight patients who met the primary response (platelet count >50 × 109/L at week 24). Central horizontal bold line is the median; the lower and upper box limits are the 1st and 3rd quartiles, respectively; and the whiskers extended to the most extreme data points, which do not exceed the 1.5 × the interquartile of the box. Plus symbol represents the mean value
Secondary efficacy endpoints
The percentage of patients with the platelet count ≥100 × 109/L and who did not have bleeding at week 24 was 15.4 % (4/26 patients; 95 % CI 4.4, 34.9 %). The percentage of patients with the platelet count ≥30 × 109/L and ≥twofold higher than the baseline value and who did not have bleeding at week 24 was 26.9 % (7/26 patients; 95 % CI 11.6, 47.8 %).
As for the percent changes of the platelet count, the median platelet count was significantly increased compared with the baseline at every time point from week 1 to week 24 (P < 0.01, signed rank sum test; Fig. 2). The median platelet count exceeded ≥30 × 109/L at week 8 and remained stable throughout the follow-up period.
The percentage of patients with Grade ≥1 hemorrhage in the WHO bleeding scale was numerically decreased at every time point compared with the baseline. Statistically significant decrease was observed at week 8 compared with the baseline (26.9 vs 57.7 %, P = 0.0215; exact McNemar’s test), whereas no significant differences were observed at other time points.
Subgroup analysis
In Table 3, the results of subgroup analyses of the percentage of patients with the platelet count ≥50 × 109/L at week 24 were summarized. Subgroups with higher response rate were patients with duration of ITP shorter than the median duration 5.9 years (46.2 %, 6/13 patients), patients who underwent splenectomy (50.0 %, 2/4 patients), patients who did not have concomitants for ITP at baseline (60.0 %, 3/5 patients), patients who did not previously receive thrombopoietin receptor agonists (36.8 %, 7/19 patients), and patients with previous therapies for ITP less than 3 (41.2 %, 7/17 patients). While factors predictive of response to rituximab have not been consistently identified across studies, shorter duration of ITP was reported to be associated with good response from several studies [14, 15] as we found in this study.
Exploratory efficacy endpoints
Peripheral blood B cells (CD20-positive cells and CD19-positive cells) were significantly decreased at week 2 and subsequent time points compared with the baseline (P < 0.001 for both parameters: signed rank sum test). The median absolute B cell count at week 2 was <5 cells/µL and persisted in low during the study. Transient but significant decrease of peripheral blood T cells (CD3-positive cells) was observed at weeks 2, 4, and 12, compared with the baseline (P < 0.05, signed rank sum test); however, the median value of absolute cell count of CD3-positive T cells remain >790 cells/µL throughout the study.
Serum IgG levels were significantly increased at week 4 compared with the baseline (P = 0.023, signed rank sum test), whereas IgM levels were significantly decreased at weeks 12 and 24, compared with the baseline (P < 0.001, signed rank sum test). These changes of serum IgG and IgM, however, were within the normal range. Serum IgA levels were not significantly changed from the baseline over 24-week study period.
Safety
Three serious adverse events required inpatient hospitalization were reported in three patients: one patient with grade 3 viral infection, one with grade 2 viral infection and one with grade 2 hypermenorrhea. All these three events recovered by supportive treatment and the patients discharged from the hospital in a week. The causal relationship of all the serious adverse events with rituximab was not completely ruled out.
The other adverse drug reactions (ADRs) that occurred in two or more patients were upper respiratory tract infection and headache in three patients each, and diarrhea, abdominal pain, malaise, and cough in two patients each. All these ADRs were grade 1 or 2 in severity.
Infusion related reactions were observed in eight patients and those that occured in two or more patients were fever, oropharyngeal pain, headache, pruritus, urticaria, and hypersensitivity, all of which were grade 1 or 2 in severity. Infusion related reactions were most frequently observed at the initial administration of rituximab (at week 0) among the injection-time points in the 4-dose study drug regimen. None of patients had adverse events led to discontinuation of the study drug, and no deaths were reported in this study.
Discussion
The response rate of the primary efficacy endpoint in this study, the percentage of patients with the platelet count ≥50 × 109/L at week 24 after the first administration of rituximab, was 30.8 % (95 % CI 14.3–51.8 %), and failed to meet the pre-determined statistical criteria of the lower confidence limit of 20 %.
However, the efficacy of rituximab in patients with chronic refractory ITP in this study is substantial when compared with the modest response rate of 2 % (1/42 patients; 95 % CI 0, 12.6 %) in placebo group reported in other clinical studies in patients with refractory ITP [13]. Also, as seen in the subgroup analysis, even heavily treated patients with chronic refractory ITP in this study exhibited moderate efficacy, with the platelet count ≥50 × 109/L at week 24, to rituximab as shown below: 50.0 % (2/4 patients) of patients who underwent splenectomy and 14.3 % (1/7 patients) of patients who previously received thrombopoietin receptor agonists. This trend becomes much clearer in this study when considering clinical benefit to patients who are at risk of fatal bleeding (i.e., the platelet count ≤30 × 109/L). As additional analysis, the percentages of patients with the platelet count ≥30 × 109/L at week 24 after administration of the study drug were evaluated, and rituximab then showed considerably high effectiveness in a total of patients (57.7 %, 15/26 patients) as well as patients previously heavily treated, who underwent splenectomy (75.0 %, 3/4 patients) and who received thrombopoietin receptor agonists (71.4 %, 5/7 patients). These lines of evidence suggest that rituximab can clinically useful for the treatment of Japanese patients with chronic refractory ITP.
The goal of treatment in ITP is to maintain the platelet count which reduces the risk of bleeding while minimizing treatment-related toxicity. To accomplish this goal, thrombopoietin receptor agonists are recently used. However, thrombocytopenia usually recurring shortly after the drug withdrawal is known as one of the drawbacks of these agonists. Thus, these agents are indefinitely used to maintain the platelet count to minimize bleeding [16]. In the sense, this study showed that rituximab’s effect lasted longer after completion of treatment; the platelet counts at all the time points exceeded 30 × 109/L until week 24 after the last dose of the study drug at week 3.
Clinical significance of rituximab in patients with ITP is still being investigated extensively outside Japan to position the therapy at an alternative treatment for ITP prior to splenectomy [15–18]. Although the details of study design was varied from study to study in terms of target population (e.g., newly diagnosed or relapsed ITP), concomitant therapy (e.g., with or without steroids), dosage and administration of rituximab (e.g., 4-weekly 375 mg/m2 or 2-times 1000 mg 2 weeks apart), and endpoints of efficacy analysis, rituximab commonly showed a clinically substantial efficacy and well tolerability in patients with ITP. Especially, several studies showed a clinically meaningful sustained response to have a chance for sparing splenectomy [12, 18–23], supporting our results in this study. Regarding the safety of rituximab, we observed severe adverse events in three patients. Two had viral infection of unknown etiology and one had hypermenorrhea. All three events were resolved by supportive treatment and all patients were discharged from hospital within a week of admission.
We, thus, conclude from the above-mentioned results that rituximab is clinically useful and involves no particular safety concerns in the treatment of Japanese patients with chronic refractory ITP.
References
Kurata Y, Fujimura K, Kuwana M, Tomiyama Y, Murata M. Epidemiology of primary immune thrombocytopenia in children and adults in Japan: a population-based study and literature review. Int J Hematol. 2011;93:329–35.
Portielje JE, Westendorp RG, Kluin-Nelemans HC, Brand A. Morbidity and mortality in adults with idiopathic thrombocytopenic purpura. Blood. 2001;97:2549–54.
Fujimura K, Kuwana M, Kurata Y, Imamura M, Harada H, Ikeda Y, et al. Is eradication therapy useful as the first line of treatment in Helicobacter pylori-positive idiopathic thrombocytopenic purpura? Analysis of 207 eradicate chronic ITP cases in Japan. Int J Hematol. 2005;81:162–8.
Kojouri K, Vesely SK, Terrell DR, George JN. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: a systematic review to assess long-term platelet count responses, prediction of response, and surgical complications. Blood. 2004;104:2623–34.
Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, Crowther MA, American Society of Hematology. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117:4190–207.
Kashiwagi H, Tomiyama Y. Pathophysiology and management of primary immune thrombocytopenia. Int J Hematol. 2013;98:24–33.
Looney RJ. B-cell targeted therapy in diseases other than rheumatoid arthritis. J Rheumatol. 2005;32(Suppl 73):25–8.
Reddy V, Jayne D, Close D, Isenberg D. B-cell depletion in SLE: clinical and trial experience with rituximab and ocrelizumab and implications for study design. Arthritis Res Ther. 2013;15(Suppl 1):S2.
British Committee for Standards in Haematology General Haematology. Task force. Guidelines for the investigation and management of idiopathic thrombocytopenic purpura in adults, children and in pregnancy. Br J Haematol. 2003;120:574–96.
Provan D, Stasi R, Newland AC, Blanchette VS, Bolton-Maggs P, Bussel JB, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010;115:168–86.
Arnold DM, Dentali F, Crowther MA, Meyer RM, Cook RJ, Sigouin C, et al. Systematic review: efficacy and safety of rituximab for adults with idiopathic thrombocytopenic purpura. Ann Intern Med. 2007;146:25–33.
Godeau B, Porcher R, Fain O, Lefrère F, Fenaux P, Cheze S, et al. Rituximab efficacy and safety in adult splenectomy candidates with chronic immune thrombocytopenic purpura: results of a prospective multicenter phase 2 study. Blood. 2008;112:999–1004.
Kuter DJ, Bussel JB, Lyons RM, Pullarkat V, Gernsheimer TB, Senecal FM, et al. Efficacy of romiplostim in patients with chronic immune thrombocytopenic purpura: a double-blind randomised controlled trial. Lancet. 2008;371:395–403.
Cooper N, Stasi R, Cunningham-Rundles S, Feuerstein MA, Leonard JP, Amadori S, et al. The efficacy and safety of B-cell depletion with anti-CD20 monoclonal antibody in adults with chronic immune thrombocytopenic purpura. Br J Haematol. 2004;125:232–9.
Zaja F, Vianelli N, Battista M, Sperotto A, Patriarca F, Tomadini V, et al. Earlier administration of rituximab allows higher rate of long-lasting response in adult patients with autoimmune thrombocytopenia. Exp Hematol. 2006;34:571–2.
Siegal D, Crowther M, Cuker A. Thrombopoietin receptor agonists in primary ITP. Semin Hematol. 2013;50:S18–21.
Khellaf M, Charles-Nelson A, Fain O, Terriou L, Viallard JF, Cheze S, et al. Safety and efficacy of rituximab in adult immune thrombocytopenia: results from a prospective registry including 248 patients. Blood. 2014;124:3228–36.
Zaja F, Baccarani M, Mazza P, Bocchia M, Gugliotta L, Zaccaria A, et al. Dexamethasone plus rituximab yields higher sustained response rates than dexamethasone monotherapy in adults with primary immune thrombocytopenia. Blood. 2010;115:2755–62.
Li Z, Mou W, Lu G, Cao J, He X, Pan X, et al. Low-dose rituximab combined with short-term glucocorticoids up-regulates Treg cell levels in patients with immune thrombocytopenia. Int J Hematol. 2011;93:91–8.
Arnold DM, Heddle NM, Carruthers J, Cook DJ, Crowther MA, Meyer RM, et al. A pilot randomized trial of adjuvant rituximab or placebo for nonsplenectomized patients with immune thrombocytopenia. Blood. 2012;119:1356–62.
Gudbrandsdottir S, Birgens HS, Frederiksen H, Jensen BA, Jensen MK, Kjeldsen L, et al. Rituximab and dexamethasone vs dexamethasone monotherapy in newly diagnosed patients with primary immune thrombocytopenia. Blood. 2013;121:1976–81.
Tran H, Brighton T, Grigg A, McRae S, Dixon J, Thurley D, et al. A multi-centre, single-arm, open-label study evaluating the safety and efficacy of fixed dose rituximab in patients with refractory, relapsed or chronic idiopathic thrombocytopenic purpura (R-ITP1000 study). Br J Haematol. 2014;167:243–51.
Ghanima W, Khelif A, Waage A, Michel M, Tjønnfjord GE, Romdhan NB, et al. Rituximab as second-line treatment for adult immune thrombocytopenia (the RITP trial): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2015;385:1653–61.
Acknowledgments
This study is a research project of the Ministry of Health, Labour, and Welfare (MHLW) Scientific Research Project. The authors are gratefully indebted to Zenyaku Kogyo Co., Ltd. for the supply of the investigational product and support for preparation of the manuscript, and to Quintiles Transnational Japan Inc. for support in conducting the clinical trial and in preparation of the manuscript, and Center for Clinical Trials, Japan Medical Association (JMACCT) for financial support. We also appreciated CTD Inc. for providing professional advises to our study group.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Miyakawa reports non-financial support from Zenyaku Kogyo, grants from Japan Medical Association Center for Clinical Trials (JMACCT), during the conduct of the study; grants and personal fees from Alexion pharmaceutical, personal fees from Daiichi Sankyo, personal fees from Fuji film, personal fees from GlaxoSmithKline, personal fees from Kyowa-Hakko Kirin, personal fees from Ono pharmaceuticals, outside the submitted work; Dr. Kanakura reports grants from Chugai Pharmaceutical Co. Ltd., personal fees from Zenyaku-Kogyo, during the conduct of the study; grants and personal fees from Kyowa-Hakkyo Kirin Co. Ltd., grants and personal fees from Otsuka Pharmaceutical Co. Ltd., grants from Takeda Pharmaceutical Co. Ltd., grants from Teijin Pharma, grants from Janssen Pharmaceutical Co. Ltd., grants and personal fees from Alexion Pharmaceutical Co. Ltd., personal fees from Shire Co. Ltd., grants from Bristol-Myers Squibb Co. Ltd., outside the submitted work; Dr. Yano has nothing to disclose. Dr. Shirasugi reports personal fees from Kyowa-Hakko Kirin, personal fees from Pfizer, personal fees from Ono pharmaceutical, personal fees from Bristol-Myers Squibb, personal fees from Celgene, personal fees from GlaxoSmithKline, outside the submitted work; Dr. Higashihara reports grants and personal fees from Chugai pharmaceutical, during the conduct of the study; grants and personal fees from Kyowa-Hakko Kirin, grants from MSD, grants from Jannsen pharmaceutical, grants from Takeda, personal fees from Sumitomo Dainippon pharma, grants from Teijin, grants from Astellas pharma, personal fees from GlaxoSmithKline, outside the submitted work; Dr. Nishiwaki reports grants from Zenyaku Kogyo Company, Limited, grants from Chugai Pharmaceutical, grants from Novartis Pharma K.K., outside the submitted work; Dr. Okamoto reports grants from Chugai pharmaceuticals, during the conduct of the study; personal fees from KyowaHakkoKirin, personal fees from Takeda, personal fees from Bristol-Myers Squibb, personal fees from Janssen pharmaceutical, personal fees from Celgene, personal fees from Alexion, personal fees from Eisai, grants from GlaxoSmithKline, outside the submitted work; Dr. Katsutani has nothing to disclose. Dr. Nomura has nothing to disclose. Dr. Kikuchi has nothing to disclose. Dr. Abe has nothing to disclose. Dr. Nishikawa has nothing to disclose. Dr. Ozaki reports grants from Japan Medical Association Center for Clinical Trials, during the conduct of the study; personal fees from Nippon Shinyaku, personal fees from Janssen pharmaceutical companies, personal fees from Chugai pharmaceutical, personal fees from Celgene, personal fees from Kyowa-Hakko Kirin pharmaceutical, outside the submitted work; Dr. Ikeda reports personal fees from Chugai pharmaceuticals, during the conduct of the study; personal fees from Novartis, personal fees from Sanofi, personal fees from Daichi Sankyo, outside the submitted work; Dr. Tomiyama reports grants from JMACCT, during the conduct of the study; personal fees from GSK, personal fees from Novartis, personal fees from Kyowa-Hokko Kirin, personal fees from Eisai, personal fees from Sysmex, outside the submitted work; Dr. Fujimura reports non-financial support from Kyowa-Hakko Kirin, during the conduct of the study; non-financial support from Medical support, outside the submitted work.
About this article
Cite this article
Miyakawa, Y., Katsutani, S., Yano, T. et al. Efficacy and safety of rituximab in Japanese patients with relapsed chronic immune thrombocytopenia refractory to conventional therapy. Int J Hematol 102, 654–661 (2015). https://doi.org/10.1007/s12185-015-1887-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-015-1887-9