Abstract
Purpose of Review
To summarize the history of titanium implants in spine fusion surgery and its evolution over time.
Recent Findings
Titanium interbody cages used in spine fusion surgery have evolved from solid metal blocks to porous structures with varying shapes and sizes in order to provide stability while minimizing adverse side effects. Advancements in technology, especially 3D printing, have allowed for the creation of highly customizable spinal implants to fit patient specific needs. Recent evidence suggests that customizing shape and density of the implants may improve patient outcomes compared to current industry standards. Future work is warranted to determine the practical feasibility and long-term clinical outcomes of patients using 3D printed spine fusion implants.
Summary
Outcomes in spine fusion surgery have improved greatly due to technological advancements. 3D printed spinal implants, in particular, may improve outcomes in patients undergoing spine fusion surgery when compared to current industry standards. Long term follow up and direct comparison between implant characteristics is required for the adoption of 3D printed implants as the standard of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal fusion procedures have been used to treat a wide range of pathologies including degenerative disc disease, spinal stenosis, spondylolisthesis, herniated discs, and trauma [1]. Over the past two decades, the incidence and prevalence of degenerative spinal disorders has increased significantly with a parallel increase in the number of spinal surgeries performed [2,3,4,5]. Surgical management of degenerative spinal disorders has been shown to reduce patient pain and disability, and improve quality of life; however, accomplishing a durable fusion with long term stability continues to be a challenge [6, 7]. The goal of spinal fusion surgery is to stabilize at least two vertebral levels. This is often accomplished by removing intervertebral disc components, placing a rigid interbody cage between the vertebrae, and fixing the structure with screws, plates, and rods to promote spine fusion. Titanium is one of the most widely used materials for interbody cages and has significantly evolved over time due to its longstanding use. Over the years, titanium cages have advanced from solid metal blocks to porous structures with varying shapes and sizes that can closely mimic properties of bone while maintaining biomechanical stability. We will discuss the evolution of titanium interbody cages and how current technology has improved their utility in spine fusion.
History
One of the earliest successful uses of interbody cages for spine fusion was implemented in 1956 by Hodgson and Stock, who used bone autografts blocks in patients with severe spine degeneration from Pott disease (Fig. 1a) [8]. In the subsequent decades, alternative constructs emerged including one by O’brien et al. which used a combination cortical femoral ring allograft packed with cancellous bone autograft and to promote spine fusion (Fig. 1b) [9]. These bone grafts showed some success in achieving fusion, but were not adequate standalone devices for stabilizing the spine.
Evolution of anterior lumbar interbody fusion cage designs. (A) Autograft block; (B) Femoral ring allograft; (C) Bagby and Kuslich (BAK) cage; (D) Polyetheretherketone (PEEK) cage; (D) SynFix implant; (F) Titanium Polyetheretherketone (Ti-PEEK) cage. Adapted from Phan et al. 2016 with permission [13]
Titanium interbody cages were introduced in the 1980s to provide more rigidity in the fusion construct and gained popularity following a clinical trial in 1992 in which Bagby and Kuslich showed the safety and efficacy of their implant in humans. This implant was a “hollow, porous, square-threaded, slightly tapered, cylindrical, titanium device” known as the BAK cage (Fig. 1c) [10]. In a multi-center, prospective clinical trial examining one- or two-level lumbar fusions, a 91% fusion rate was achieved with BAK cages after 24 months.
By the early 2000s, titanium interbody cages were commonplace and continuously undergoing modification to improve patient outcomes. Wider implants were shown to be associated with greater segment stability, leading to the implementation of the lumbar-tapered cage: a trapezoid-shaped interbody cage shown to have higher axial strength and resistance to subsidence compared to cylindrical implants (Fig. 1d) [11, 12]. The theoretical advantages were restoration of the spine to a more physiologic angle while still providing the benefits of a cylindrical metal cage (Fig. 1).
In addition to its mechanical properties, titanium has also been shown to have several bioactive properties that support its use as an implant material. Müller et al. showed that titanium alloys facilitate bone growth through osteoblast activation [14]. Navarrette et al. demonstrated that cells grown on titanium alloys stimulate an osteogenic-angiogenic microenvironment [15]. Textor et al. theorized that the safety and improved osseointegration of titanium implants is due to an oxide layer forming when the titanium alloy comes into contact with air, shielding the surrounding biologic tissue from highly reactive metal species and promoting osseointegration by mimicking the ceramic properties of hydroxyapatite [16, 17]. The stable oxide film formed with titanium alloy, especially in the form Ti-6Al-4 V, was a key finding that shifted material choices away from pure titanium to titanium alloy [18].
The drawbacks of titanium use include an elastic modulus much higher than bone (100-110Gpa vs 10-40Gpa of cortico-cancellous bone) and high resistance to mechanical loading [19]. Remodeling of bone under physiologic weightbearing is an important factor for maintaining bone health. Large differences in mechanical properties at the bone-implant interface can lead to stress shielding – a process by which bone adjacent to the implant resorbs over time because the majority of the mechanical load is on the implant, leading to subsidence and potential implant failure. In addition, traditional titanium implants are radiopaque which interferes with radiographic assessment of the bone implant surface. In the subsequent decade, advancements in additive manufacturing, also known as 3D Printing (3DP), offered some solutions to these drawbacks.
3d Printing in Spine Surgery
The first documented use of 3DP to aid in spine surgery was in 1999 [20]. At this time, it was only used to recreate physical anatomical models as a visual aid for complex cases. As technology became more advanced, a subcategory of 3D printing—selective laser sintering (SLS) — emerged as a viable method of creating implantable devices. SLS printing is a technique by which a laser solidifies and fuses powdered material in layers to form a solid structure [21, 22]. In 2004, an SLS printing machine with a high-powered laser capable of melting metals was built which allowed for the creation of 3D printed titanium parts for commercial use (Fig. 2).
Selective laser sintering (SLS) process used to fuse powdered titanium into a solid structure. A high-power laser fuses powdered titanium particles wherever it makes contact to powdered material in a layer-by-layer fashion. Adapted from Awad et al. 2020 with permission [23]
By 2015, there was a surge in clinical trials using 3DP titanium implants for spinal fusion [24, 25]. Shortly thereafter, in 2017, the FDA published validated guidelines for 3D printed medical devices with specifications of design, manufacturing and testing [26]. As a result, the demand for and use of 3D printing in medicine has increased dramatically in the past 5 years with the majority of 3D printed devices being used for orthopedic spine cases [27]. It is estimated that the production of 3D printed implantable devices will continue to grow around 29% annually through 2026 [28].
The advent of porous titanium implants, made using SLS 3D printing, helped overcome many of the drawbacks of traditional spinal implants. Porous titanium can be modified to reduce the mechanical strength mismatch between implant and bone, and its lower density results in less radiographic interference [29]. The layer-by-layer manufacturing process of SLS printing also allows the manufacture of very precise and complex internal structure geometries for titanium implants, unlike conventional machining techniques. Additionally, SLS generates less waste as it utilizes additive manufacturing—the technique of adding just enough material in a piece-wise fashion to create a part. Previous methods of creating metal parts—like machining or acid washing—use a subtractive manufacturing technique to remove excess material from a starting block, which requires more raw material and produces more waste. By using additive manufacturing techniques, raw material waste has been reported as low as 5%, compared to 15% in subtractive techniques [30].
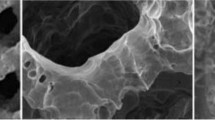
3D printed titanium also paved the way for further advancements in surface interface technology aimed at improving osseointegration and implant properties. Sheng et al. describes some of the most recent changes to functionality in titanium implants and categorized them into chemical, biologic, and physical modifications [31]. One example of a chemical modification is anodizing, whereby a current is passed through the titanium surface causing an oxidation–reduction reaction to form a surface conducive to bone healing [32, 33]. (Fig. 3a) Electrophoretic deposition (EPD) is another technique that adds a thin surface coating to titanium through an electrochemical reaction [34]. It has been used to apply inorganic coatings like hydroxyapatite, graphide oxide, and silver cations in a wide variety of orthopedic implants [34,35,36]. Physical modification includes processes that alter the internal or external structure of the implant. For example, laser surface engineering utilizes high powered lasers to melt surface material, texturizing the implant and enhancing the bone-implant interface (Fig. 3b) [37, 38]. Examples of biologic modification (Fig. 3c) include a hydrogel matrix that can absorb water and allow for controlled release of antibiotics [38], a sodium alginate gel coating containing pre-osteoblasts [39], and direct antibiotic coating. These surface modifications can be used in combination with 3D printing to enhance the efficacy and biocompatibility of spinal implants to achieve successful fusion.
Various surface modifications and resulting microstructure of a titanium implant. Microstructure is visualized on scanning electron microscopy (SEM) after a) electrophoretic deposition, b) laser peening, and c) hydrogel packing. Adapted from Sheng et al. 2022 [31]
Drawbacks associated with 3D printing include cost, which is estimated to be 2–5 times higher than conventional implants [40,41,42]. In addition, 3D printing technology is not available at many institutions which must outsource manufacturing, further increasing financial burden. Additionally, data is limited on the long-term efficacy of 3D printed implants and how they compare to implants currently being used in clinical practice. Another drawback is the possibility of hypersensitivity reactions. Chung et al. [43] reported a case of a patient with eosinophilia found incidentally after vertebral body reconstruction using a 3D printed implant [44]. The patient had no clinical symptoms but may have had a hypersensitivity response to titanium powder particles. This may warrant further investigation as 3D printed titanium devices become more common. Lastly, there is a theoretical risk of lower relative strength in 3D printed titanium implants compared to pure metal implants. Insufficient layer bonding and thermal fluctuations in the manufacturing process can result in failure under load and residual stress. However, finite element analysis and biomechanical testing have demonstrated comparable results when comparing 3D printed titanium to other methods of titanium implant manufacture [45].
Clinical studies
The two most commonly used materials for spinal implants today are titanium alloys and polyetheretherketone (PEEK), which have been compared often in clinical research. PEEK is an FDA-approved thermoplastic created for spine implantation as an alternative to titanium implants due to its bone-mimicking mechanical properties (i.e. elastic modulus of 3.8Gpa which is similar to cancellous bone), potentially reducing rates of subsidence and implant failure [46, 47]. Additionally, PEEK is radiolucent on imaging so physicians can assess bony union more easily during postoperative follow up. A major drawback was the finding that PEEK creates a biofilm in the body that inhibits osseointegration at the bone-implant interface (Fig. 4) [48, 49].
Histologic section of sagittal plane through cranial and caudal vertebral bodies in an ovine model. ROI analysis (yellow dot outline) shows most osseointegration in PTA implant compared to PEEK and PSP. Image coded as follows: bone stained, red; fibrous tissue, gray; implant, black (metal) or tan (plastic); and background, white. PEEK, polyetheretherketone; PSP, plasma sprayed porous titanium-coated PEEK; PTA, porous titanium alloy; ROI, region of interest. Adapted from Mcgilvray et al. 2018 with permission [49]
Given the promising results of porous titanium implants in animal studies, there has been increasing effort to validate the utility of 3D printed porous titanium implants in humans. Amini et al. performed one of the first cohort studies that directly compared porous 3D printed titanium to PEEK cages in standalone lateral lumbar interbody fusion (LLIF) [50]. In this retrospective study of 113 patients, radiographs were collected at 6- and 12-month follow up to assess for subsidence. Multivariate analysis showed that patients treated with 3D printed titanium cages were less likely to develop severe subsidence, defined as a loss of disc height of more than 50%, than patients receiving PEEK implants (OR = 0.05, 95% CI = 0.01, 0.3) (p = 0.001). The reason for this was postulated to be improved stability due to higher osseointegration of porous titanium implants. Makino et al. found increased bone ongrowth in porous titanium and titanium coated PEEK implants at 6 and 12 months post operation compared to PEEK only implants [51]. The same authors later published a case series comparing the two types of cages in 63 patients and found that there was significantly lower subsidence and endplate cyst formation in the porous titanium group compared to PEEK, but no difference in fusion rate or surgery effectiveness at 6 and 12 months [52].
In a systematic review in 2023, Patel et al. directly compared 3D printed porous titanium to PEEK implants in the setting of LLIF with a focus on clinical outcomes and subsidence rates [1]. Six out of the seven papers included in this review showed clinical outcomes in favor of 3D printed porous titanium over PEEK. Fusion rates in the 3D printed porous titanium implant group were superior to PEEK and resulted in equal or fewer reports of subsidence, re-operation, and graft failure.
Segi et al. compared a tapered 3D printed porous titanium cage versus squared PEEK cage in a retrospective study of 32 patients undergoing extreme lateral interbody fusion and assessed for vertebral endplate concavity (VEC), a risk factor for subsidence [53]. Patients were followed for 3 months postoperatively and were found to have no significant difference in spinal alignment. No VEC progression was noted in the 3D printed titanium group while the PEEK group was found to have progression in 21% of the levels examined. Additionally, subsidence was observed in the PEEK group at 3 months but not in the 3D printed porous titanium group. The authors note that subsidence did not significantly alter the spinal alignment at 3 months, but the local lordotic angle was significantly affected. The clinical implications of these observations would likely be answered with longer term follow up. Finally, the authors of this study attributed the difference in VEC rates to the material properties and the geometry of the implant which may affect the friction generated when inserted in the operating room [53].
While these findings are significant, it is important to note that the literature is inconsistent on the effect of subsidence on clinical outcomes. One report found that although late cage subsidence worsened the rate of bony fusion, subsidence in the early post operative period (less than 3 months) did not significantly affect clinical outcomes [54]. In contrast, another group found that some level of intraoperative endplate injury was associated with subsidence leading to significantly less clinical improvement [55].
Khan et al. attempted to control for confounding variables in a cohort study with patients receiving a 3D printed porous titanium implant versus propensity matched patients receiving lumbar PEEK cages [56]. They tracked clinical outcomes including the numerical rating scale (NRS) for leg pain, NRS back pain, Oswestry Disability Index (ODI) scores, and Euro-Qol-5D along with radiographic evidence of subsidence and fusion success. The cohort included 228 patients assessed at 3 months and 12 months post-operation. Quality of life scores (Euro-Qol-5D) were comparable in both groups, but the 3D printed titanium group showed significantly greater improvement in ODI scores compared to PEEK cages at both 3 and 12 months. The Euro-Qol-5D score is a subjective evaluation of quality of life while the ODI score is reflective of the functional ability of the patient. Additionally, the porous titanium cohort showed higher fusion rates, lower subsidence, and lower indirect costs associated with surgical management compared to the PEEK cohort [56].
The radiographic superiority of 3D printed titanium implants was further corroborated by Alan et al. who found that porous titanium was significantly less likely to show subsidence (8% vs 27%, p = 0.001) by 12 months follow up compared to PEEK cages[57]. This study consisted of a retrospective observational cohort analysis of 192 patients undergoing LLIF, with either 3D printed porous titanium or PEEK. The study concluded that while rates of severe subsidence were lower in the porous titanium group, there were statistically similar revision rates after LLIF. Uniquely, this study performed a cost analysis of the implants by considering costs of revision as well as raw materials and found that 3D printed porous titanium could be an economically superior choice compared to PEEK if the cost was below a certain threshold ($1200) [57].
On the other hand, Kim et al. compared 3D printed porous titanium to PEEK cages in a retrospective review of 83 patients who underwent single level minimally invasive transforaminal interbody fusion and found that there was no difference in ODI scores between the 2 groups at 1 year [58]. Wang et al. also found that posterior lumbar fusions using 3D printed implants do not significantly differ in operating room time, intraoperative blood loss, post operative neurologic recovery, or final intervertebral fusion compared to PEEK [59].
A major limitation of all current comparative clinical studies is that none have reported long-term follow up beyond one year postoperatively. Additionally, the porous titanium implants used in these studies have slightly different internal organizations/structures, as 3D printing technology has allowed for finer modification of individual implant parameters such as porosity and density. Further work is warranted to examine not just material but also the implantation technique used during spine surgery. A 2019 survey of 586 spine surgeons globally found that surgeons in North America reported the lowest rate of minimally invasive spinal surgery techniques (MISST) compared to other countries [60]. In contrast, surgeons in Asia and South America reported the highest frequency of fully endoscopic MISST of all countries. Surgical technique prevalence varies by region, which can further affect clinical outcomes. Therefore, these differences should be accounted for in future work investigating implant success.
Future Designs
Patient bone density tends to decrease over time, especially in the setting of aging, chronic medication use, and degenerative disease. Therefore, there is utility in considering patient specific factors like age, bone quality, and anatomic variations in creating a patient-specific implant using 3D printing. Titanium implants can now be customized with varying densities, porosities, and stiffness characteristics. Commercially available 3D printed titanium implants are generally separated into two categories: patient-specific (PS) and off-the-shelf (OTS) [44, 49]. PS implants are shaped based on pre-operative computed tomography (CT) or magnetic resonance imaging (MRI) and are manufactured according to patient-specific anatomy [40] while OTS implants are available in a range of porosity and stiffnesses but are not fully individualized (Fig. 5) [61]. There is evidence to suggest that PS implants are associated with less intraoperative blood loss and greater satisfaction compared to OTS [62], but more investigation is needed to confirm this finding. While PS implants are costly to produce, further advancements in manufacturing technology may reduce financial burden on healthcare institutions and patients.
A standard OTS implant (left) compared to a PS implant (right) shaped to the patient’s anatomy. Adapted from DeFrancesco 2023 with permission by article writer [63]
In addition to changing the physical geometry of an implant through 3D printing, surface modification is a promising new avenue for improved spine fusion success. Bioactive implants are now possible with advancements in 3D printing technology, as the porous microstructure of 3D printed implants offers an ideal environment for their use as a drug delivery vehicle [64] while maintaining biomechanical stability. Additionally, surface treatment with growth factors [65], functional molecules [66], and peptides [67] could enhance the material characteristics of an implant to reduce complication rates and hasten healing.
With the high customizability made possible by 3D printing, it can be challenging to test every permutation of implant characteristic in a traditional trial-and-error fashion. For example, implant porosity is a characteristic that can be modified in almost endless ways through size, shape, and orientation (Fig. 6). Artificial intelligence (AI) algorithms, which have advanced greatly in the past few years, can be used to build predictive analytical tools to optimize 3D printing parameters. AI has already been used in conjunction with finite element analysis tools to simulate and predict the mechanical behavior of medical implants but further work on orthopedic specific implants is warranted [68, 69].
Examples of porous 3D printed implants with varying vertical porosity parameters (a, c, e) and diagonal parameters (b, d, f) to create different microstructures. Adapted from Wu et al. 2023 with permission [45]
Conclusion
Advancements in 3D printing technology allowing for the creation of highly customizable implants have shown significant benefit in spine surgery. Titanium interbody cages for spine fusion have evolved greatly over the years, from solid metal implants to changes in external geometry and texture, and most recently customized internal structure to mimic native bone. Available literature shows evidence that 3D printed porous titanium interbody cages may reduce subsidence rates, improve clinical outcomes, and demonstrate stronger bioactivity and biocompatibility when compared to conventional titanium implants and other materials such as PEEK. With patient-specific implants becoming easier and cheaper to produce through 3D printing, future work should further distinguish between patient-specific versus off-the-shelf spinal implants and compare their clinical and practical applications.
Data Availability
No datasets were generated or analysed during the current study.
References
Patel NA, et al. Three-Dimensional-Printed Titanium Versus Polyetheretherketone Cages for Lumbar Interbody Fusion: A Systematic Review of Comparative In Vitro, Animal, and Human Studies. Neurospine. 2023;20(2):451–63.
Kobayashi K, et al. Epidemiological trends in spine surgery over 10 years in a multicenter database. Eur Spine J. 2018;27(8):1698–703.
Ragab A, Deshazo RD. Management of back pain in patients with previous back surgery. Am J Med. 2008;121(4):272–8.
Martin BI, et al. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976). 2007;32(3):382–7.
Weiner DK, et al. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med. 2006;7(2):143–50.
McGirt MJ, et al. Lumbar Surgery in the Elderly Provides Significant Health Benefit in the US Health Care System: Patient-Reported Outcomes in 4370 Patients From the N2QOD Registry. Neurosurgery. 2015;77(Suppl 4):S125–35.
Parker SL, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg. 2014;82(1–2):230–8.
Hodgson AR, Stock FE. Anterior Spine Fusion for the Treatment of Tuberculosis of the Spine: The Operative Findings and Results of Treatment in the First One Hundred Cases. JBJS. 1960;42(2):295–310.
O’Brien JP, et al. Simultaneous combined anterior and posterior fusion. A surgical solution for failed spinal surgery with a brief review of the first 150 patients. Clin Orthop Relat Res. 1986;203:191–5.
Kuslich SD, et al. The Bagby and Kuslich Method of Lumbar Interbody Fusion: History, Techniques, and 2-Year Follow-up Results of a United States Prospective. Multicenter Trial Spine. 1998;23(11):1267–78.
Steffen T, Tsantrizos A, Aebi M. Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs. Spine (Phila Pa 1976). 2000;25(9):1077–84.
Spruit M, et al. Posterior reduction and anterior lumbar interbody fusion in symptomatic low-grade adult isthmic spondylolisthesis: short-term radiological and functional outcome. Eur Spine J. 2002;11(5):428–33.
Phan K, Mobbs RJ. Evolution of Design of Interbody Cages for Anterior Lumbar Interbody Fusion. Orthop Surg. 2016;8(3):270–7.
Müller U, et al. Do human osteoblasts grow into open-porous titanium? Eur Cell Mater. 2006;11:8–15.
Olivares-Navarrete R, et al. Rough titanium alloys regulate osteoblast production of angiogenic factors. Spine J. 2013;13(11):1563–70.
Sul YT, et al. Optimum surface properties of oxidized implants for reinforcement of osseointegration: surface chemistry, oxide thickness, porosity, roughness, and crystal structure. Int J Oral Maxillofac Implants. 2005;20(3):349–59.
Textor M, et al. Properties and Biological Significance of Natural Oxide Films on Titanium and Its Alloys. Berlin Heidelberg: Springer; 2001. p. 171–230.
Litak J, Szymoniuk M, Czyżewski W, Hoffman Z, Litak J, Sakwa L, Kamieniak P. Metallic Implants Used in Lumbar Interbody Fusion. Materials (Basel). 2022;15(10):3650. https://doi.org/10.3390/ma15103650.
Zhu Y, et al. “Effect of Elastic Modulus on Biomechanical Properties of Lumbar Interbody Fusion Cage.” J Mater Sci Technol. 2009;25:325–8.
D’Urso PS, et al. Spinal biomodeling. Spine (Phila Pa 1976). 1999;24(12):1247–51.
Popov VV Jr, et al. Design and 3D-printing of titanium bone implants: brief review of approach and clinical cases. Biomed Eng Lett. 2018;8(4):337–44.
Zhang L, et al. Three-dimensional (3D) printed scaffold and material selection for bone repair. Acta Biomater. 2019;84:16–33.
Awad A, et al. 3D printing: Principles and pharmaceutical applications of selective laser sintering. Int J Pharm. 2020;586:119594.
Witowski J, et al. From ideas to long-term studies: 3D printing clinical trials review. Int J Comput Assist Radiol Surg. 2018;13(9):1473–8.
Van Norman GA. Expanded Patient Access to Investigational New Devices: Review of Emergency and Nonemergency Expanded Use, Custom, and 3D-Printed Devices. JACC Basic Transl Sci. 2018;3(4):533–44.
FDA, Technical Considerations for Additive Manufactured Medical Devices; Guidance for Industry and Food and Drug Administration Staff. Federal Information & News Dispatch, 2017: 57462.
Kermavnar T, et al. Three-Dimensional Printing of Medical Devices Used Directly to Treat Patients: A Systematic Review. 3D Print Addit Manuf. 2021;8(6):366–408.
Yang, L., S. Bhaduri, and T.J. Webster, Biomaterials in translational medicine. 2018: Academic Press.
Cheng BC, et al. A comparative study of three biomaterials in an ovine bone defect model. Spine J. 2020;20(3):457–64.
Wixted CM, et al. Three-dimensional Printing in Orthopaedic Surgery: Current Applications and Future Developments. J Am Acad Orthop Surg Glob Res Rev. 2021;5(4):e20.00230-11.
Sheng X, Wang A, Wang Z, Liu H, Wang J, Li C. Advanced Surface Modification for 3D-Printed Titanium Alloy Implant Interface Functionalization. Front Bioeng Biotechnol. 2022;10:850110. https://doi.org/10.3389/fbioe.2022.850110.
Park S, Han U, Choi D, et al. Layer-by-layer assembled polymeric thin films as prospective drug delivery carriers: design and applications. Biomater Res 2018;22(1):29. https://doi.org/10.1186/s40824-018-0139-5.
Minagar S, et al. Cell response of anodized nanotubes on titanium and titanium alloys. J Biomed Mater Res A. 2013;101(9):2726–39.
Boccaccini AR, et al. Electrophoretic deposition of biomaterials. J R Soc Interface. 2010;7(Suppl 5(Suppl 5)):S581-613.
Shalom H, Feldman Y, Rosentsveig R, Pinkas I, Kaplan-Ashiri I, Moshkovich A, Perfilyev V, Rapoport L, Tenne R. Electrophoretic Deposition of Hydroxyapatite Film Containing Re-Doped MoS₂ Nanoparticles. Int J Mol Sci. 2018;19(3):657. https://doi.org/10.3390/ijms19030657.
Dulski M, Balcerzak J, Simka W, Dudek K. Innovative Bioactive Ag-SiO2/TiO2 Coating on a NiTi Shape Memory Alloy: Structure and Mechanism of Its Formation. Mater. 2021;14(1):99. https://doi.org/10.3390/ma14010099.
Kurella A, Dahotre NB. Review paper: surface modification for bioimplants: the role of laser surface engineering. J Biomater Appl. 2005;20(1):5–50.
Shin T, et al. A laser-aided direct metal tooling technology for artificial joint surface coating. Int J Precis Eng Manuf. 2017;18(2):233–8.
Kumar N, et al. Design and 3D printing of novel titanium spine rods with lower flexural modulus and stiffness profile with optimised imaging compatibility. Eur Spine J. 2023;32(6):1953–65.
Amelot A, Colman M, Loret J-E. Vertebral body replacement using patient-specific three–dimensional-printed polymer implants in cervical spondylotic myelopathy: an encouraging preliminary report. The Spine Journal. 2018;18(5):892–9.
De Beer N, Bloem N. An economic cost model for patient-specific intervertebral disc implants. Presented at the ISEM 2011 Proceedings, September 21-23, Stellenbosch University, Stellenbosch, South Africa; 2011. http://hdl.handle.net/10019.1/39628.
Spetzger U, Frasca M, König SA. Surgical planning, manufacturing and implantation of an individualized cervical fusion titanium cage using patient-specific data. Eur Spine J. 2016;25(7):2239–46.
Chung KS, et al. Vertebral Reconstruction with Customized 3-Dimensional-Printed Spine Implant Replacing Large Vertebral Defect with 3-Year Follow-up. World Neurosurg. 2019;126:90–5.
Burnard JL, et al. 3D-printed spine surgery implants: a systematic review of the efficacy and clinical safety profile of patient-specific and off-the-shelf devices. Eur Spine J. 2020;29(6):1248–60.
Wu Y, et al. An overview of 3D printed metal implants in orthopedic applications: Present and future perspectives. Heliyon. 2023;9(7):e17718.
Brooke NS, et al. Preliminary experience of carbon fibre cage prostheses for treatment of cervical spine disorders. Br J Neurosurg. 1997;11(3):221–7.
Heary RF, et al. Elastic modulus in the selection of interbody implants. J Spine Surg. 2017;3(2):163–7.
Yoon BJV, et al. Optimizing surface characteristics for cell adhesion and proliferation on titanium plasma spray coatings on polyetheretherketone. Spine J. 2016;16(10):1238–43.
McGilvray KC, et al. Bony ingrowth potential of 3D-printed porous titanium alloy: a direct comparison of interbody cage materials in an in vivo ovine lumbar fusion model. Spine J. 2018;18(7):1250–60.
Adl Amini D, et al. Evaluation of cage subsidence in standalone lateral lumbar interbody fusion: novel 3D-printed titanium versus polyetheretherketone (PEEK) cage. Eur Spine J. 2021;30(8):2377–84.
Makino T, et al. Impact of mechanical stability on the progress of bone ongrowth on the frame surfaces of a titanium-coated PEEK cage and a 3D porous titanium alloy cage: in vivo analysis using CT color mapping. Eur Spine J. 2021;30(5):1303–13.
Makino T, et al. Comparison of Short-Term Radiographical and Clinical Outcomes After Posterior Lumbar Interbody Fusion With a 3D Porous Titanium Alloy Cage and a Titanium-Coated PEEK Cage. Global Spine J. 2022;12(5):931–9.
Segi N, Nakashima H, Shinjo R, Kagami Y, Machino M, Ito S, Ouchida J, Morishita K, Oishi R, Yamauchi I, Imagama S. Vertebral Endplate Concavity in Lateral Lumbar Interbody Fusion: Tapered 3D-Printed Porous Titanium Cage versus Squared PEEK Cage. Medicina (Kaunas). 2023;59(2):372. https://doi.org/10.3390/medicina59020372.
Satake K, et al. Cage subsidence in lateral interbody fusion with transpsoas approach: intraoperative endplate injury or late-onset settling. Spine Surg Relat Res. 2017;1(4):203–10.
Tohmeh AG, et al. Radiographical and clinical evaluation of extreme lateral interbody fusion: effects of cage size and instrumentation type with a minimum of 1-year follow-up. Spine (Phila Pa 1976). 2014;39(26):E1582-91.
Khan I, et al. Clinical and Cost-Effectiveness of Lumbar Interbody Fusion Using Tritanium Posterolateral Cage (vs. Propensity-Matched Cohort of PEEK Cage). Spine Surg Relat Res. 2022;6(6):671–80.
Alan N, et al. Graft subsidence and reoperation after lateral lumbar interbody fusion: a propensity score-matched and cost analysis of polyetheretherketone versus 3D-printed porous titanium interbodies. J Neurosurg Spine. 2023;39(2):187–95.
Kim DY, Kwon OH, Park JY. Comparison Between 3-Dimensional-Printed Titanium and Polyetheretherketone Cages: 1-Year Outcome After Minimally Invasive Transforaminal Interbody Fusion. Neurospine. 2022;19(3):524–32.
Wang Y, et al. Application of three-dimensional printed porous titanium alloy cage and poly-ether-ether-ketone cage in posterior lumbar interbody fusion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36(9):1126–31.
Lewandrowski KU, et al. Regional variations in acceptance, and utilization of minimally invasive spinal surgery techniques among spine surgeons: results of a global survey. J Spine Surg. 2020;6(Suppl 1):S260-s274.
Mokawem M, et al. Lumbar interbody fusion rates with 3D-printed lamellar titanium cages using a silicate-substituted calcium phosphate bone graft. J Clin Neurosci. 2019;68:134–9.
Culler SD, Martin GM, Swearingen A. Comparison of adverse events rates and hospital cost between customized individually made implants and standard off-the-shelf implants for total knee arthroplasty. Arthroplast Today. 2017;3(4):257–63.
DeFrancesco C. A 3D-Printed Solution for the Spine. UConn Health Today. 2023. https://today.uconn.edu/2023/09/a-3d-printed-solution-for-the-spine/#. Accessed March 2024.
Wu W, et al. A therapeutic delivery system for chronic osteomyelitis via a multi-drug implant based on three-dimensional printing technology. J Biomater Appl. 2016;31(2):250–60.
Park JY, et al. 3D printing technology to control BMP-2 and VEGF delivery spatially and temporally to promote large-volume bone regeneration. J Mater Chem B. 2015;3(27):5415–25.
Zhang W, et al. 3D printed composite scaffolds with dual small molecule delivery for mandibular bone regeneration. Biofabrication. 2020;12(3):035020.
Chen L, et al. Enhancement in sustained release of antimicrobial peptide and BMP-2 from degradable three dimensional-printed PLGA scaffold for bone regeneration. RSC Adv. 2019;9(19):10494–507.
Yan L, et al. Finite element analysis of bone and implant stresses for customized 3D-printed orthopaedic implants in fracture fixation. Med Biol Eng Comput. 2020;58(5):921–31.
Roach DJ, et al. Utilizing computer vision and artificial intelligence algorithms to predict and design the mechanical compression response of direct ink write 3D printed foam replacement structures. Addit Manuf. 2021;41:101950.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JL – Idea generation, manuscript research, writing, and preparation.
FJ, DH, MP – Manuscript research and writing.
WH – Idea generation, manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, J.J., Jacome, F.P., Hiltzik, D.M. et al. Evolution of Titanium Interbody Cages and Current Uses of 3D Printed Titanium in Spine Fusion Surgery. Curr Rev Musculoskelet Med (2024). https://doi.org/10.1007/s12178-024-09912-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s12178-024-09912-z