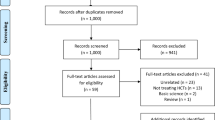
Abstract
Purpose of Review
The lateral meniscus oblique radial tear (LMORT) of the posterior horn is a relatively new term for one of the more common types of lateral meniscal tears found in patients with acute anterior cruciate ligament (ACL) injuries. Given the importance of anatomical reduction and preservation of the lateral meniscus to maintain normal knee stability and slow the progression of early-onset osteoarthritis, LMORT classification and treatment guidelines have been formulated. This article provides a review of the prevalence, classification, biomechanics, surgical repair techniques, and outcomes related to LMORT injuries.
Recent Findings
Current research demonstrates favorable clinical results when LMORTs are surgically treated based on recent evidence. Biomechanically, repair of the higher grade 3 and 4 LMORT lesions have led to comparable results when compared to an intact lateral meniscus, and superior results when compared to partial meniscectomy and untreated tears. Ongoing research is aimed to determine the difference between LMORT repairs compared to intact lateral menisci at the time of ACL surgery regarding comparable patient outcomes.
Summary
LMORT lesions are common tears of the lateral meniscus that should be treated surgically based on tear type at the time of ACL surgery. The benefit of doing so has already been demonstrated biomechanically.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal injuries are one of the most common concomitant pathologies found with ACL injuries [1,2,3], with medial meniscal injuries more commonly found in chronic ACL-deficient patients and lateral meniscal injuries typically occurring more in the acute setting [1, 4, 5]. Specifically, out of the various types of meniscal lesions, the posterior horn appears to be the most affected [6, 7]. Wilson et al. [8] found that in the adolescent and pediatric population, posterior horn tears of the lateral meniscus composed 15% of all observed meniscal pathology, with 85% involving the root directly or in close proximity.
The lateral meniscus oblique radial tear (LMORT) was first classified into four types with types 3 and 4 lesions found to be most common. Overall, the presence of LMORT tears with an acute ACL injury was noted to be 12% [9••]. Despite LMORT tears being one of the more prevalent lateral meniscal pathologies found in the setting of ACL ruptures, there is a paucity of data describing appropriate treatment guidelines for these tears [9••]. In contrast to more commonly studied meniscal lesions such as ramp and root tears, both of which having widely accepted classifications and treatment considerations [10, 11], the classification of the LMORT is much more recent despite these lesions being equally as common [9••]. Since the publication of this classification, there have only been a few additional studies to our knowledge examining these types of meniscal lesions [12•, 13•, 14•, 15].
It is important to consider the type of LMORT present as the treatment varies based on the severity of the tear. Given the important roles of the meniscus as a cartilage protectant and secondary knee stabilizer, restoring proper intra-articular anatomy with the reduction and repair of the lateral meniscus is crucial [15,16,17]. Being able to accurately identify, classify, and treat these lesions may result in improved patient outcomes and may slow the progression of lateral compartment osteoarthritis.
Epidemiology
In the recent study examining 600 consecutive patients who underwent anterior cruciate ligament reconstruction (ACLR) from three high-volume orthopaedic surgeons, Krych et al. [9••] found that LMORTs occurred in 72 (12%) of the patients and accounted for 23% of all lateral meniscal tears. Jeon et al. [14•] found that out of 635 consecutive ACLRs, 97 (15.3%) of the patients had a concomitant LMORT and accounted for approximately 51% of the lateral meniscal tears in their patient population. In both studies, type 4 LMORTs were the most encountered tears with Krych et al. recording 34 (47.9%) and Jeon et al. recording 62 (32.6%).
Lmort Tear Classification
Type 1
These are partial-thickness radial oblique tears that originate < 10 mm from the posterior root attachment (Fig. 1) [9••]. These are the least common of the LMORTs accounting for 1.1–9.9% of the tears [9••, 14•].
Type 1 LMORT [9••]
Type 2
These are full-thickness radial oblique tears that originate < 10 mm from the posterior root attachment, but do not directly involve the root itself (Fig. 2) [9••]. These make up 12.7–14.7% of the LMORTs [9••, 14•].
Type 2 LMORT [9••]
Type 3
The LMORT type 3 lesions are incomplete, radial oblique tears that originate ≥ 10 mm from the root and propagate towards the posterior root attachment but do not extend through the posterior rim to the meniscofemoral ligament (Fig. 3) [9••]. The biggest discrepancy between Krych’s and Jeon’s studies was found here as the latter reported this tear in only 2.6% of patients whereas the former reported this to be the second most prevalent tear at 29.6% [9••, 14•].
Type 3 LMORT [9••]
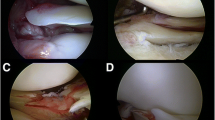
Type 4
These are complete, radial oblique tears that originate ≥ 10 mm from the posterior root attachment and extend through the posterior rim, reaching the meniscofemoral ligament (Fig. 4) [9••]. As stated previously, Krych et al. and Jeon et al. reported the LMORT 4 to be the most common type [9••, 14•].
Type 4 LMORT [9••]
Jeon et al. [14•] further sub-classified this type into two subtypes, a LMORT 4a which is reminiscent of the classic LMORT 4 described by Krych et al. [9••], and a LMORT 4b (Fig. 5) which is described as containing a longitudinal tear at the meniscocapsular junction of the remnant flap.
Type 3 vs. Type 4
Out of the four types of LMORTs, types 3 and 4 are the most difficult to distinguish between, made evident in the two LMORT studies examining lesion identification and classification [9••, 14•]; however, despite the high interobserver variability, the treatment for them are the same. Furthermore, given the capsular extension of the type 4 tears, it can be noted that these tears tend to be more hemorrhagic due to the proximity of the inferior lateral genicular artery and its branches that supply the posterior horn of the lateral meniscus being commonly disrupted. This is not to infer that type 3 LMORT lesions lack signs of bleeding as they do penetrate through the red-white zone of the meniscus, but just not all the way to the vascular capsule. Nonetheless, the common theme between Krych’s and Jeon’s studies was that despite this variability, the LMORT 4 lesion appeared to be the most prevalent. Whether it is a type 3 or 4 lesion, it is biomechanically important to treat them both in the same manner with repair [12•, 13•].
Biomechanics
In a robotic biomechanical study examining the knee kinematics associated with types 3 and 4 LMORT tears, Smith et al. [12•] demonstrated that when compared to an isolated ACL (iACL) tear, ACL tears associated with LMORT type 3 and 4 tears increased anterior laxity for both the anterior drawer and the pivot shift. LMORT 3 lesions plus ACL tears demonstrated a statistically significant anterior drawer at 90° of flexion; while the LMORT 4 plus ACL tears demonstrated a statistically significant anterior drawer at both 60° and 90° and for the pivot shift at 15° and 30°, respectively. The increased laxity found for LMORT 4 lesions would be consistent with these lesions extending all the way to the capsule like a complete radial tear. Lateral meniscal extrusion measured by ultrasound was also increased by these LMORT lesions, and greater for the LMORT 4 vs. 3 lesions. Consequently, due to the unstable nature of these LMORT tears, a higher axial load is transmitted directly on the tibial surface at certain degrees of knee flexion [18].
In a second cadaveric study using the same study parameters as the first, Smith et al. [13•] examined the knee kinematics of the clinical scenario of ACLR in the presence of a LMORT 3 or 4 tear (Fig. 6). Specifically, the LMORT 3 and 4 tears were either left alone in-situ or treated with either partial meniscectomy or repair using spanning sutures following ACLR. In the first testing condition utilizing robotic measurements of translation, they confirmed an all-inside soft tissue allograft ACLR restored anterior translation with the anterior drawer and the pivot shift comparable to the intact ACL state.
Kinematic results of LMORT lesions [13•]. ACLR + LMORT3/4 repair resulted in comparable kinematic results to completely intact lateral menisci (asterisks). Leaving the lesion in situ or excising it with ACLR led to increased laxity when compared to intact menisci at most or all degrees of knee angulation. (A) ACLR + LMORT3 tear demonstrated an increase in anterior translation at 15° of knee flexion during pivot shift compared to an intact ACL and intact lateral meniscus (small circle). (B) ACLR + LMORT4 treated with partial meniscectomy demonstrated increased meniscal extrusion at all knee flexion angles during anterior drawer compared to ACLR with an intact meniscus, an intact ACL with an intact meniscus, and ACLR + LMORT4 repair; it also demonstrated increased extrusion with anterior drawer with the knee flexed at 90° compared to ACLR with the LMORT4 left in situ
Subsequently, creation of both a LMORT 3 and 4 tear left in-situ after ACLR led to significantly more anterior translation with anterior drawer and with pivot shift compared to both the intact state and iACLR [13•]. This increased laxity effect was greater for the LMORT 4 lesions compared to both the intact state and iACLR being found at all flexion angles. Meniscal extrusion was significantly greater at all flexion angles for both LMORT 3 and 4 lesions. However, repairing both types of LMORT tears with all-inside spanning sutures restored baseline normal stability for both anterior translation and meniscal extrusion [13•]. In contrast, surgically managing these lesions with partial meniscectomy resulted in similar findings to the in situ LMORT 3 and 4 lesions, but there was even more joint laxity with the anterior drawer at 90° following partial meniscectomy, and a LMORT 4 lesion treated with partial meniscectomy had the greatest overall meniscal extrusion.
Given the time zero biomechanical unstable nature of not repairing the LMORT type 3 and 4 lesions relative to increased joint laxity and meniscal extrusion-made even worse with partial meniscectomy of these tears- an ACL graft may experience additional strain following reconstruction which could impede the healing process or contribute to graft failure [19]. The major kinematic effects of LMORT 3 and 4 lesions after ACLR left in situ or repaired or treated with partial meniscectomy are summarized in Fig. 6.
Treatment Options
Nonoperative
Historically, LMORT type tears were treated conservatively at the time of the ACLR [6]. Perhaps this was because the lateral meniscus is believed to have greater healing potential when compared to the medial meniscus [20, 21]. However, given the unstable nature of most of these tears, nonoperative management for these lesions should not be considered. The only exception being a LMORT 1 lesion that has a low chance of propagating, but even then, it might be worth considering a partial meniscectomy to decrease this chance.
Arthroscopic Partial Meniscectomy
This treatment option is likely best reserved for only type 1 LMORT lesions. It may not be possible to repair these smaller tears due to the lack of tissue needed for the repair to hold with a spanning suture and a transtibial repair would be difficult for the same reason. Furthermore, this tear is in a region with low vascularization which makes the healing potential of a repair relatively low [22].
Transtibial Repair
This technique is preferred for type 2 LMORTs (Fig. 7). This lesion shares a striking resemblance to a type 4 root tear [10] and can be thought of almost as a “root variant” lesion. Type 2 LMORTs typically can be well reduced to the root via suturing with a transtibial tunnel. This repair method is the treatment of choice for all types of root tears except for the type 1 tear (partial) which is treated with debridement similar to a LMORT 1 lesion.
Repair with Spanning Sutures
This technique with side-to-side suturing is done arthroscopically with a suture passing instrument. Tying an arthroscopic knot is typically preferred for the LMORT types 3 and 4 (Fig. 8). Based on procedural comfortability and surgeon preference, these repairs can be accomplished utilizing an arthroscopic all-inside approach with spanning sutures or even an inside-out approach [23]. These alternative capsular-based suturing methods theoretically could decrease normal lateral meniscal mobility compared to a spanning suture repair construct (meniscus-based), but this difference has not been studied.
Special Considerations
There can be circumstances where a certain LMORT lesion can be affectively treated with a different technique, dependent on the presenting anatomy and the surgeon’s comfortability in treating these lesions. For example, there may be a scenario where a LMORT 1 may extend far enough posteriorly but not necessarily completely transect that portion of the meniscus. These more extensive type 1 LMORTs may benefit from a one spanning suture repair. This can be similarly done with type 2 LMORTs as well (Fig. 9). In both cases the medial portion must contain enough healthy tissue for adequate purchase to prevent repair failure.
Clinical Outcomes
Patient Selection
A sample of 15 patients who underwent surgical repair of types 2–4 LMORTs between the years of 2017–2020 and who were enrolled in our institution’s registry (Surgical Outcomes System [SOS]) were selected for analysis. The demographics of this patient population can be seen in Table 1. The mean age of this cohort was 18.0 years old (95% CI [16.8, 19.2]).
Data Collection
The patients completed the following validated patient-reported outcome measures (PROMs) both pre- and postoperatively: the visual analog scale (VAS) [24], the single assessment numeric evaluation (SANE) [25], the Knee Injury and Osteoarthritis Outcome Score (KOOS) subscales [26], the Lysholm survey [27], and the International Knee Documentation Committee (IKDC) survey [28].
Each patient was individually assessed using the minimal clinically import difference (MCID), the substantial clinical benefit (SCB), and the patient acceptable symptom state (PASS) thresholds for the KOOS subscales [29, 30] and the IKDC [29, 30]. The MCID and SCB thresholds were unable to be assessed in 2 of the patients as they did not complete their preoperative surveys.
Statistical Analysis
Quantitative variables were assessed using the Mann–Whitney U test and were expressed using mean (95% confidence intervals). Qualitative variables were assessed using either the Chi-square or the Fischer exact test and were expressed using absolute frequency (percentage). Statistical analysis was performed using JMP®, Version 17. SAS Institute Inc., Cary, NC, 1989–2021. For statistical analysis in this study, P < 0.05 was considered statistically significant.
Results
Each patient completed their surveys at their 2-year follow-up, the details are summarized in Table 2. All PROMs significantly improved (p < 0.01) at final follow-up compared to their preoperative levels.
PASS, MCID, and SCB thresholds for each individual patients is summarized in Table 3. It was noted that 5 (33%) patients did not meet the SCB of Δ35.8 for the KOOS ADL subscale despite achieving the PASS (100). Furthermore, 2 (15%) did not achieve the MCID of Δ25.9 for the same reason.
Data Interpretation
Subjectively, the patients significantly improved in all areas which more than likely was the result of the ACLR and being able to return to normal activities. Given there being no control group to compare to, the PASS, MCID, and SCB thresholds were applied to each individual patient. More than 65% of the patients achieved the PASS threshold for all PROMs with exception of the KOOS: activities of daily living (ADL) (53%) which carries a PASS of 100.0. The SCB for this subscale is noted to be 35.8, meaning that for a patient to achieve “substantial benefit” from the surgery for that given parameter, they would have to have a difference of at least 35.8 at final follow-up compared to their preoperative state. The issue with this is that 5 patients scored 65 + on their preoperative ADL subscale which makes them ineligible of achieving the SCB. So it really would be best to look at the PASS for each patient and if it reaches the threshold, then one can see whether a substantial gap had to be crossed to achieve it. This example highlights the importance of using multiple PROMs to aid in final data interpretation.
Do LMORTs Heal?
LMORTs tend to heal very well (Fig. 10).
In our clinical experience, patients rarely return to the OR due to a failed LMORT repair. Typically, if a patient presents with a subsequent LMORT it occurs following a retear of their ACL graft; however, they will often occur in locations that differ from their previous LMORT (Fig. 11).
Out of the 61 (62.8%) patients that underwent second-look arthroscopy a year following their primary surgery for either residual discomfort or persistent irritation at the post-tie screw fixation site, Jeon et al. [14•] noted that 80.3% (n = 49) of the LMORTs healed completely. Nonetheless, if a patient does return to the operating room and a subsequent LMORT is found it is important to distinguish between a repair failure and a new LMORT entirely.
In series of 29 patients with a mean follow-up of 26.68 months, Zhou et al. found that 96.6% of the patients achieved meniscus healing on postoperative MRI following repair of complete radial posterior lateral meniscus root tears using spanning sutures [31•]. Additionally, during a second-look of 22 of those patients, it was noted that 86.4% of the patients achieved a completely healed meniscus with the remaining patients exhibiting partial healing [31•]. Furthermore, none of the 29 patients exhibited symptoms suggestive of lateral meniscal pathology [31•].
In a series of 41 consecutive patients who underwent ACLR with either inside-out or all-inside repair of radial/flap tears of the posterior lateral meniscus with a mean follow-up > 3 years, Tsujii et al. found that patients with these meniscal lesions (study group) demonstrated comparable patient outcomes with those who underwent iACLR (control) [32•]. It was noted that patients in the study group exhibited more sagittal extrusion on postoperative MRI compared to the control group [32•]. 30 patients in the study group underwent a second arthroscopic look which showed complete healing in 60% of patients, partial healing in 30% of patients, and failure to heal in 10% of the patients [32•]. Between the two groups, there were no significant chondral differences seen in the lateral femoral condyles; however, it was noted that patients in the study group demonstrated significantly worse chondral lesions of the lateral tibial plateau [32•].
Conclusion
LMORT lesions are tears of the posterior horn of the lateral meniscus that commonly occur at the time of an acute ACL injury. Despite the prevalence of the LMORT, it has not been until recently that these tears have been classified and studied in detail. Due to the unstable nature of these tears evidenced by biomechanical studies, surgical repair of the LMORT types 2–4 is necessary to adequately reduce the posterior horn of the lateral meniscus to decrease strain on the ACL graft, and also to slow the progression of osteoarthritis. Due to the paucity in current literature surrounding this relatively new description of LMORT lesions, especially given the new classification and treatment guidelines, it is difficult to speculate how objectively similar a repaired LMORT is compared to a lateral meniscus with no prior pathology. Though the results of recent case series and biomechanical studies have been promising, further studies are needed to further elucidate the success of these repairs. Furthermore, given the results of previous studies demonstrating the healing properties of these lesions [13•, 31•, 32•], repair technique for the higher grade LMORT lesions may need to be optimized.
Data Availability
The Intraoperative arthroscopic images in figures 1-5 and 7-11are not publicly available in order to protect the patients' privacy; additionally, the data in tables 1-3 was retrieved from our institution's registry and may be available upon request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Borchers JR, Kaeding CC, Pedroza AD, et al. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–93. https://doi.org/10.1177/0363546511406871.
Mansori AE, Lording T, Schneider A, Dumas R, Servien E, Lustig S. Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: possible local and generalized risk factors. Int Orthop. 2018;42(9):2113–21. https://doi.org/10.1007/s00264-018-3992-x.
Praz C, Vieira TD, Saithna A, et al. Risk Factors for lateral meniscus posterior root tears in the anterior cruciate ligament-injured knee: an epidemiological analysis of 3956 patients from the SANTI Study Group. Am J Sports Med. 2019;47(3):598–605. https://doi.org/10.1177/0363546518818820.
Feucht MJ, Bigdon S, Bode G, et al. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34. https://doi.org/10.1186/s13018-015-0184-x. (Published 2015 Mar 18).
Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):112–8. https://doi.org/10.1007/s00167-014-3467-6.
Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(7):1439–43. https://doi.org/10.1177/0363546511398212.
Westermann RW, Wright RW, Spindler KP, Huston LJ, MOON Knee Group, Wolf BR. Meniscal repair with concurrent anterior cruciate ligament reconstruction: operative success and patient outcomes at 6-year follow-up. Am J Sports Med. 2014;42(9):2184–92. https://doi.org/10.1177/0363546514536022.
Wilson PL, Wyatt CW, Romero J, Sabatino MJ, Ellis HB. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6(11):2325967118803888. https://doi.org/10.1177/2325967118803888. (Published 2018 Nov 8).
•• Krych AJ, LaPrade MD, Cook CS, et al. Lateral meniscal oblique radial tears are common with acl injury: a classification system based on arthroscopic tear patterns in 600 consecutive patients. Orthop J Sports Med. 2020;8(5):2325967120921737. https://doi.org/10.1177/2325967120921737. (Published 2020 May 19). Explanation: This was the original study where the classification and prevalence of the LMORT lesion was first introduced.
LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–9. https://doi.org/10.1177/0363546514559684.
Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5(4):e871–5. https://doi.org/10.1016/j.eats.2016.04.009. (Published 2016 Aug 8).
• Smith PA, Bezold WA, Cook CR, et al. Kinematic analysis of lateral meniscal oblique radial tears in the anterior cruciate ligament-deficient knee. Am J Sports Med. 2021;49(14):3898–905. https://doi.org/10.1177/03635465211052521. Explanation: This was the first of the 2 LMORT biomechanical studies highlighting the increased anterior translation and meniscal extrusion associated with the LMORT lesion compared to an isolated ACL injury with an intact lateral meniscus.
• Smith PA, Bezold WA, Cook CR, et al. Kinematic analysis of lateral meniscal oblique radial tears in anterior cruciate ligament-reconstructed knees: untreated versus repair versus partial meniscectomy. Am J Sports Med. 2022;50(9):2381–9. https://doi.org/10.1177/03635465221102135. Explanation: this was the second of the 2 LMORT biomechanical studies highlighting the restoration of knee stability with LMORT type 3 and 4 repair to levels comparable to an intact meniscus. It is also highlighted the residual anterior translation and meniscus extrusion associated with leaving a higher grade LMORT lesion in situ or treating it with a partial meniscectomy at the time of ACLR.
• Jeon YS, Alsomali K, Yang SW, Lee OJ, Kang B, Wang JH. Posterior horn lateral meniscal oblique radial tear in acute anterior cruciate ligament reconstruction incidence and outcomes after all-inside repair: clinical and second-look arthroscopic evaluation. Am J Sports Med. 2022;50(14):3796–804. https://doi.org/10.1177/03635465221126506. Explanation: this was a second large LMORT study detailing the prevalence of the different LMORT lesions in consecutive patients who underwent ACLR. Additionally, a large percentage of the LMORT patients underwent a second-look arthroscopic procedure which demonstrated good healing potential of these lesions.
Weber J, Koch M, Angele P, Zellner J. The role of meniscal repair for prevention of early onset of osteoarthritis. J Exp Orthop. 2018;5(1):10. https://doi.org/10.1186/s40634-018-0122-z. (Published 2018 Apr 2).
Patil SS, Shekhar A, Tapasvi SR. Meniscal preservation is important for the knee joint. Indian J Orthop. 2017;51(5):576–87. https://doi.org/10.4103/ortho.IJOrtho_247_17.
Shimomura K, Hamamoto S, Hart DA, Yoshikawa H, Nakamura N. Meniscal repair and regeneration: current strategies and future perspectives [published correction appears in J Clin Orthop Trauma. 2020 Nov-Dec;11(6):1169-1171]. J Clin Orthop Trauma. 2018;9(3):247–53. https://doi.org/10.1016/j.jcot.2018.07.008.
Ohori T, Mae T, Shino K, et al. Different effects of the lateral meniscus complete radial tear on the load distribution and transmission functions depending on the tear site. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):342–51. https://doi.org/10.1007/s00167-020-05915-8.
Uffmann W, ElAttrache N, Nelson T, et al. Posterior lateral meniscal root tears increase strain on the reconstructed anterior cruciate ligament: a cadaveric study. Arthrosc Sports Med Rehabil. 2021;3(2):e505–13. https://doi.org/10.1016/j.asmr.2020.11.005. (Published 2021 Feb 3).
Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K. Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(8):1953–61. https://doi.org/10.1177/0363546504263702.
Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17(4):396–401. https://doi.org/10.1007/s00167-008-0711-y.
Doral MN, Bilge O, Huri G, Turhan E, Verdonk R. Modern treatment of meniscal tears. EFORT Open Rev. 2018;3(5):260–8. https://doi.org/10.1302/2058-5241.3.170067. (Published 2018 May 21).
Golz AG, Mandelbaum B, Pace JL. All-inside meniscus repair. Curr Rev Musculoskelet Med. 2022;15(4):252–8. https://doi.org/10.1007/s12178-022-09766-3.
Höher J, Münster A, Klein J, Eypasch E, Tiling T. Validation and application of a subjective knee questionnaire. Knee Surg Sports Traumatol Arthrosc. 1995;3(1):26–33. https://doi.org/10.1007/BF01553522.
Shelbourne KD, Barnes AF, Gray T. Correlation of a single assessment numeric evaluation (SANE) rating with modified Cincinnati knee rating system and IKDC subjective total scores for patients after ACL reconstruction or knee arthroscopy. Am J Sports Med. 2012;40(11):2487–91. https://doi.org/10.1177/0363546512458576.
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. https://doi.org/10.2519/jospt.1998.28.2.88.
Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–4. https://doi.org/10.1177/036354658201000306.
Greco NJ, Anderson AF, Mann BJ, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form in comparison to the Western Ontario and McMaster Universities Osteoarthritis Index, modified Cincinnati Knee Rating System, and Short Form 36 in patients with focal articular cartilage defects. Am J Sports Med. 2010;38(5):891–902. https://doi.org/10.1177/0363546509354163.
Beletsky A, Naami E, Lu Y, et al. The minimally clinically important difference and substantial clinical benefit in anterior cruciate ligament reconstruction: a time-to-achievement analysis. Orthopedics. 2021;44(5):299–305. https://doi.org/10.3928/01477447-20210819-03.
Muller B, Yabroudi MA, Lynch A, et al. Defining thresholds for the patient acceptable symptom state for the IKDC subjective knee form and KOOS for patients who underwent ACL reconstruction. Am J Sports Med. 2016;44(11):2820–6. https://doi.org/10.1177/0363546516652888.
• Zhuo H, Chen Q, Zhu F, Li J. Arthroscopic side-to-side repair for complete radial posterior lateral meniscus root tears. BMC Musculoskelet Disord. 2020;21(1):130. https://doi.org/10.1186/s12891-020-3156-1. Explanation: demonstrated great healing potential for LMORT-like lesions when surgically repaired using an all-inside spanning suture repair. Additionally, the cohort in this series demonstrated satisfactory PROs following their procedure.
• Tsujii A, Yonetani Y, Kinugasa K, Matsuo T, Yoneda K, Ohori T, Hamada M. Outcomes more than 2 years after meniscal repair for radial/flap tears of the posterior lateral meniscus combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(12):2888–94. https://doi.org/10.1177/0363546519869955. Explanation: This study demonstrated that patients with LMORT-like lesions had comparable postoperative PROMs when compared to those patients who underwent iACLR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All patients signed an informed consent to be enrolled in our institution’s registry (Surgical Outcomes System [SOS]; Arthrex, Naples, FL) under the protection of the Salus IRB (Protocol: SOS #1).
Conflict of Interest
Adam V. Daniel, MD declares that he has no conflict of interest.
Aaron J. Krych, MD has received consulting fees from Arthrex, JRF, Vericel, and Responsive Arthroscopy; royalties from Arthrex and Responsive Arthroscopy; grants from DJO and Exatech; and research support from Aesculap/B.Braun, Ceterix, and Histogenics.
Patrick A. Smith, MD has received consulting fees and royalties from Arthrex; compensation for services other than consulting from Alpha Orthopedic Systems and Medical Device Business Services; support for education from Elite Orthopedics; and hospitality payments from Sanofi-Aventis, Davol Inc, Flexion Therapeutics, Scilex Pharmaceuticals, DePuy Synthes Sales, Lilly, Novartis Pharmaceuticals, and Breg.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Daniel, A.V., Krych, A.J. & Smith, P.A. The Lateral Meniscus Oblique Radial Tear (LMORT). Curr Rev Musculoskelet Med 16, 306–315 (2023). https://doi.org/10.1007/s12178-023-09835-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-023-09835-1