Abstract
Purpose of Review
The purpose of this study was to review the clinical and functional outcomes of meniscus repair in children and adolescents.
Recent Findings
The sequel of meniscal tears and the outcome of meniscus repair have been well studied in adults. However, these topics have received less attention in the pediatric population despite the high prevalence and potentially critical effect on long-term knee function in children.
Summary
Meniscus repair has a healing rate ranging from 33 to 100% with less than 40% reoperation rate. Several factors have been suggested to play a role in healing, such as concomitant ACL reconstruction and complexity of the tear. There is a lack of standardization among the utilization of functional outcome and activity level questionnaires across studies; however, most report improved function postoperatively. Other important considerations include bucket handle tears, the discoid meniscus, rehabilitation and return to sports, and alternatives after failed meniscus repair. Based on the favorable outcomes reported, meniscus repair should be attempted in most meniscus tears in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscus tears, together with ACL tears, are recognized as the most common injuries in pediatric athletes, increasing over time [1, 2]. This increase is believed to be multifactorial, due to a combination of increased recognition of the issue, improved diagnostic methods, an increase in sports participation and sport intensity, as well as a trend towards earlier athletic specialization [3, 4, 5•, 6,7,8].
The clinical effect of meniscal tears and subsequent repair has been poorly described in the pediatric population. The menisci play a critical role in load sharing and shock absorption, with injuries resulting in significant rates of long-term morbidity [3, 7]. The potential impact of the meniscus injuries can be appreciated when considering that approximately 50% of patients with meniscus injury may develop knee osteoarthritis within 10 to 20 years from the injury [9, 10]. Therefore, it is important to study the outcomes of meniscus repair in children and to identify factors that can enhance meniscus healing in an attempt to prevent osteoarthritis progression at an early age.
Unfortunately, the exact prevalence of meniscal injuries in the pediatric population is unknown. Initially, meniscus injuries in children were thought to be extremely rare [11]. A closer look at epidemiological studies conducted almost 30 years ago shows an incidence of meniscus injury in adolescent patients of 52 per 100,000 patients, which is almost half to that of patients 20–50 years old. Interestingly, meniscus injuries in patients up to 9 years old are rare with 1 meniscus injury per 100,000 patients [12]. Recent work suggests that true occurrence of meniscus injury is greater than previously thought, mainly due to increased sports participation [3, 4]. The incidence of meniscal injury in US high school athletes have been reported as high as 40.7 per 100,000 in males and 22.3 per 100,000 in females [13•]. Meniscus tears are also shown to occur in the less commonly affected preadolescent population. One retrospective study evaluating patients with hemarthrosis demonstrated meniscal injury in up to 45% of preadolescents presenting with an acutely swollen knee following an injury [2].
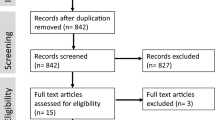
Once torn, most meniscal tears require surgical intervention, the two primary options being resection of the damaged tissue or suture repair [4]. While there has been a recent trend towards repair in pediatrics and adolescents, the evidence surrounding these treatment algorithms are widely adopted from literature in adults [5•, 8]. However, a recent meta-analysis of studies reviewing the operative management of meniscus tears in children confirmed a trend towards repair from 1979 to 2015, suggesting the shift to be based on poor long-term outcomes after partial meniscectomy [14]. Herein, we present a review of the clinical and functional outcomes of meniscus repair in children and adolescents, in an attempt to identify potential risk factors for failure but also to discuss specific conditions of the pediatric meniscus.
Surgical Outcome of Meniscus Repair in Children
A recent systematic review evaluating 287 patients (mean age range, 13–16 years) in eight studies reported healing rates ranging from 33 to 100% (100%, 96%, 89%, 84%, 74%, 62%, 50%, and 33% respectively) suggesting a favorable outcome in most studies [5•]. Another systematic review that also performed a meta-analysis evaluated isolated meniscus tears in adolescent patients aged from 10 to 19 evaluated 373 patients in which 64 repairs were performed. At an average follow-up of 10.8 years, a combined 37% re-tear rate with a combined Tegner score of 7.6 was reported, even though the heterogeneity of the studies is rather high not allowing safe conclusions to be drawn from the pooled data [14].
The incidence of isolated meniscus tears in children varies significantly among different studies. Furthermore, most studies reporting healing rates are in knees with concomitant ACL reconstruction, which has been shown to affect meniscus healing in adults [15, 16]. To our knowledge, there are only two studies evaluating the outcomes related to isolated meniscal tears. In a retrospective case series of 45 patients under 18 years (mean age 15.8 years), overall clinical success was reported in 62% of patients who underwent arthroscopic repair [17]. This data is supported by another case series, reporting clinical healing in 68% of 19 repairs and normal MRI in 50% of patients [18].
Several other studies report healing rate for meniscus tears in children and adolescents regardless the presence of an ACL reconstruction at the time of the meniscus repair. Few of these studies included a population of primarily isolated meniscus tear with a concomitant ACL reconstruction performed in less than 50% of the patients. A complete healing rate of only 33% has been reported in a small case series of 12 patients with mean age 13 years old. In this study, CT arthrogram or MRI was used for healing evaluation and only 3 patients were graded as completely healed. A closer evaluation showed that 3 patients underwent subsequent surgery and another two had occasional pain, leaving 7 asymptomatic patients (58%). This suggests that some patients may be asymptomatic without evidence of complete healing [19]. A retrospective analysis of meniscus repairs in 25 patients less than 17 years old with 29 meniscus tears showed healing by clinical criteria in 82.7% of the lesions (or 84% when considering number of patients versus meniscus tears) [20].
Most studies report presence of concomitant ACL reconstruction surgery in more than 50% of the included patients with the rate ranging from 58 to 79% of patients. In a study of 29 patients younger than 20 years old with follow-up longer than 10 years, 62% of meniscus repairs were shown to have healed based on a rigorous multifactorial battery of assessment including imaging, physical examination, and subjective patient reported outcome questionnaires. Interestingly, an additional 3 patients were asymptomatic, however with incomplete healing per MRI criteria [21]. In a large case series of 250 meniscus repairs in 240 patients with a 61.8% of complete healing, data were reported separately for pediatric patients. Of those, 11 patients were from 9 to 14 years old and 57 were 15–18 years old with a healing rate of 63% and 66%, respectively. Even though age was not found to be significant for outcome, the healing rates for the 15 patients and the 6 patients in the age groups of 31–35 and over 36 were lower, approximately 53% and 33%, respectively [22].
Excellent healing rates have been documented in a retrospective review of 29 meniscal repairs in 26 knees, in which no patient underwent subsequent meniscus surgery suggesting 100% healing at a minimum follow-up of 2 years, and 24 out of 26 patients returning to previous activity level [7]. Another retrospective review of 49 knees in 45 patients younger than 18 years old (mean age 13.2, open physes in 78%), approximately 96% of the patients were considered healed based on clinical criteria. Forty out of 45 patients returned to their pre-injury level of activity [8]. In a case series involving 19 patients with meniscus tears treated with all-inside arthroscopic repair, the healing rate was 89.5% at 6 years average follow-up [23]. In a study reporting two cases of repaired meniscus in two 4-year-old patients, both patients did extremely well with no symptoms and return to previous activity level [24]. Finally, in a study of 99 patients with meniscus repair in conjunction with ACL reconstruction, a 74% clinical healing rate was reported [25].
Factors Affecting Healing
Concomitant ACL
The healing rate for repaired meniscus tears in isolation versus that in concomitant ACL reconstruction is unclear in children. In adults, several studies have shown the beneficial outcome of ACL reconstruction in meniscus healing [15, 16]. In children, there are no high level of evidence directly comparing the healing rate between isolated and meniscus tears combined with ACL reconstruction. Most of the reports would consist of comparative analyses as part of a case series that have limited power. In one of those reports of 13 children as part of a large series, 100% of the 5 isolated meniscus tears failed to heal at 7-month follow-up. In contrast, only 37.5% of the 8 meniscus repairs done with concomitant ACL reconstruction showed evidence of non-healing, suggesting an enhancing healing effect for the ACL reconstruction [26].
As reported above, the clinical success of meniscus healing in isolated meniscus tears ranged from 62 to 68% [17, 18]. In contrast, 74% healing rate was reported for 99 patients with meniscus repair in conjunction with ACL reconstruction [25], which again may faintly suggest a beneficial effect of concomitant ACL reconstruction.
Type of Tear
In a retrospective review of 45 meniscus tears, it was found that the type of the tear may contribute to successful repair. Specifically, in this series, the repaired meniscus healed in approximately 62%. However, 80% of the simple tears and 68% of the displaced bucket handle tears had a clinical successful outcome, but only 13% of the complex meniscus tears have healed. An analysis of the 17 failed menisci showed that almost half of the failures (47%) occurred within the first 6 months from the repair. Overall, the average time for failure was 17 months with a range of 3 to 60 months. Apart from complexity of tear, rim width was also found to affect outcome with tears located at a distance of 3–6 mm from the meniscosynovial junction have a higher chance to fail compared with those within 3-mm distance [17]. The same group evaluated 99 patients with meniscus repair in conjunction with ACL reconstruction 2 years after the initial study and reported an 84% healing rate in simple tears, 59% in bucket handle tears and 57% in complex tears, confirming their previous findings that complex and bucket handle tears have a higher risk of non-healing [25].
Medial Versus Lateral Meniscus
In terms of medial or lateral meniscus repairs, a case series of 29 patients identified a significantly higher incidence of medial meniscus failure rate compared with lateral meniscus tears. Specifically, only 4 out of 18 lateral menisci failed to heal, in contrast to 7 out of 11 medial menisci (22% versus 64%) [21]. In a study of 99 patients, a tear of the medial meniscus was also found to predispose to failure with 15 out of 48 failures (31%) in the medial meniscus versus 2 out of 26 (7%) failures of the lateral meniscus (p = 0.03) [25]. A similar trend favoring the lateral meniscus was found by Kyrch et al. with 15 out of 20 lateral meniscus healed versus 13 out of 25 medial meniscus (75% versus 52%), without statistical significance (p = 0.11).
Skeletal Maturity and Age
Presence of open physes has been associated with better outcome in meniscus healing. Specifically, in a retrospective review of 49 knees in 45 patients younger than 18 years old, all 35 patients with open physes healed their meniscus repair, compared with 80% healing rate for the remaining 10 skeletally mature patients [8]. In contrast, a statistically significant difference in healing rate was also demonstrated in a retrospective analysis of 99 meniscal repairs with concomitant ACL reconstruction. Healing was achieved in 29 out of 32 repairs in skeletally mature patients versus only in 44 out of 67 repairs in skeletally immature patients (91% versus 66%, respectively, p = 0.01) [25].
When comparing outcomes of meniscus repair in children versus adults, one could expect better outcome in children due to their higher of healing potential. As described in detail above, two recent systematic reviews that explore the current outcomes of meniscal repair in pediatrics and adolescents showed statistically significant improvements in postoperative activity level and knee function with a failure rate of 37% at more than 10 years [5•, 14]. Two recent systematic reviews in adult population demonstrated similar if not better results [27, 28]. Specifically, in a systematic review of studies with more than 5-year follow-up, the re-operation rate was 23% [27]. Another systematic review that reported outcomes of meniscus repairs at more than 10 years demonstrated a re-operation rate of 20.7% [28]. While children and adolescents are considered to have an advanced capacity for healing compared with adults, the previous literature show possibility for successful repair of meniscal lesions regardless of age.
Functional Outcomes of Meniscus Repair in Children
Clinical outcomes are significantly improved after meniscus repair. In a retrospective study of 19 patients with mean age 14 years old (range 9–18), mean Tegner score improved from 3.9 to 7.1 and mean Lysholm score improved from 55.9 to 85.4 at a mean follow-up of 22.3 months. Seventy percent of patients achieved good/excellent outcome versus 30% who did fair or poor [18]. In a case series of 12 patients, Accadbled et al. reported an improvement in Lysholm score from 65.3 to 96.3 (p = 0.002) while Tegner score remained unchanged from 6.9 to 6.6 postoperatively [19]. Kyrch et al. reported similar improvement in IKDC subjective score from 65.1 to 89.4 (p = 0.0001) postoperatively [17]. In another study evaluating meniscus repairs in the setting of concomitant ACL reconstruction, Kyrch et al. reported an improvement in subjective IKDC from 48 preoperatively to 90 postoperatively and in Tegner from 1.9 preoperatively to 6.2 postoperatively [25]. Mintzer et al. reported a postoperative Lysholm score of 90 and a SF-36 physical functioning score of 91 demonstrating excellent outcomes after meniscus repair [7]. Similarly, Vanderhave et al. reported an average Tegner score of 7.7 in 45 patients under 18 years old that underwent meniscus repair [8]. Schmitt et al. reported a mean Lysholm score of 95.7 and a mean subjective IKDC of 90.7 postoperatively. Mean Tegner score was 7.6 preoperatively and 7.3 postoperatively [23]. In another study of 29 menisci, mean Lysholm score was 95 postoperatively, but Tegner score showed a slight postoperatively decrease from 7.8 to 7.2 [20].
An overview of the clinical score assessment after meniscus repair shows excellent Lysholm and IKDC scores postoperatively. In contrast, Tegner score has the tendency to remain unchanged or even decrease postoperatively in several studies when compared to pre-injury activity level [19, 20, 23]. As a consequence, the improved outcome in functional scores needs to be evaluated carefully, since the favorable outcomes can be originating from an overall decrease in activity level.
Specific Considerations
Bucket Handle Tears
Even though initially thought to be less common than other variants, comprising ~ 10% of overall meniscal tear pathology [29], recent studies of isolated meniscus injuries in children indicate a prevalence of bucket handle lesions ranging from 21 to 49% [17, 18]. Treatment recommendation is repair, pending viability of the handle fragment [30] due to the increased risk of later development of osteoarthritis after meniscectomy in pediatric knees [31].
Repair of bucket handle tears appears to be associated with poor clinical outcome due to their limited potential to heal [17, 25]; however, clinical success rate for isolated tears has been reported as high as 68% [17]. Factors affecting outcome include rim width and tear complexity. Bucket handle tears have not been shown to have a higher statistical incidence of failure compared with simple tears (32% failure versus 20% failure, p = 0.49) [17] when treated in isolation. However, these results are significantly affected when performed in conjunction with ACL reconstruction (bucket handle repair failure, 41%; simple repair failure, 16%; p = 0.006) [25].
Discoid Meniscus
The estimated incidence of discoid lateral menisci in the USA is 3 to 5% [32]. Most stable variants remain clinically silent, noted incidentally during surgery or imaging of the affected knee. Presentation in younger patients is generally with a painless “snapping knee,” which may progress to mechanical symptoms and limited range of motion (ROM), while adolescents typically present with pain, locking, catching, or swelling after an associated joint trauma [30, 33]. Historically, complete meniscectomy was advocated for the treatment of discoid menisci; however, reports of subsequent degenerative changes, early onset of osteoarthritis, or even development of osteochondritis dissecans, in conjunction with the promising findings of meniscus preservation techniques, have shifted the paradigm to support saucerization with repair [30, 34, 35•].
Ahn et al. expanded on their 2008 retrospective review of pediatric patients treated with partial meniscectomy and repair who demonstrated significantly improved postoperative function and activity level after a mean of 4.2 years, with a clinical series documenting similar outcomes in a cohort with comparable patient demographics at a mean of 10.1-year follow-up [36]. Degenerative changes were observed (39%), however at a significantly lower rate than those who underwent subtotal meniscectomy from the same group (88%) [35•, 36]. In a direct comparative study of 57 knees in patients a mean age of 11.7 years, no differences were found between complication rate, physical exam findings, or self-reported functional outcome scores between patients who underwent discoid meniscal saucerization alone and those who received additional stabilization, after a mean of 15 months [4]. Similar conclusions of functional improvement regardless of surgical treatment have been reached in a retrospective review of 100 knees followed for a minimum of 2 years; however, patients < 10 years old had a 2.37 chance of achieving greater Lysholm scores than those > 10 years old (p = 0.054; 95% CI, − 0.9 to 12.3) [34]. In a recent 2018 prospective comparison of arthroscopic treatment for lateral discoid meniscus in children (age < 13) versus adults (age > 13), previous findings were further supported with no difference in IKDC scores between meniscectomy alone and meniscectomy with repair groups at 30 months, although children had significantly higher functional activity (IKDC score, 91.1) as compared with adults (IKDC score, 73.7, p = 0.001) [34].
Overall, these data suggest that preservation of the discoid meniscus may not necessarily to lead to superior short-term outcomes in terms of patient ability or activity; however, longer-term studies implicating the deleterious sequel of meniscectomy on joint health support repair of discoid meniscus in these patients.
Return to Sports
Postoperative rehabilitation characterized by limitation in ROM, weight-bearing restriction, and muscular strengthening is key to allow healing after meniscus repair. Suggested immobilization ranges from 2 weeks to 1 month with the leg locked in extension or placed in a hinged brace. Conservative protocols delay increase in ROM from 0° to 90° until 3 to 4 weeks. Protected weight-bearing with crutches occurs initially, with full weight-bearing commencing at 3 to 4 weeks, as tolerated [17,18,19, 37•]. Theoretically, immobilization and protected weight-bearing protects the healing tissue from damaging shear forces, which occur during pivoting and squatting motions.
Closed-chain exercises for quadriceps strengthening and physical therapy are suggested to begin by 4 to 6 weeks. Full clearance for pivoting or contact sports occurs after 6 months [17,18,19, 37•]. Timeline may be dependent on tear variant, with healing in the discoid meniscus requiring longer protected rehabilitation as compared with non-discoid menisci and also the presence of concomitant ACL reconstruction [25, 37•].
Alternatives for Meniscal Tears Not Amenable for Repair
When the meniscus is not amenable for repair, occurring with degenerated, macerated tears, or as lesion margins cannot be coapted and stabilized, surgical alternatives can be considered.
Arthroscopic partial meniscectomy is widely practiced in cases during which arthroscopic repair is not possible or has failed to heal, patients aged ≥ 40 years, or with meniscal tears located in the centralized white-white zone. Removal of any portion of the meniscus allows transmission of force that would be otherwise dissipated through the cartilaginous cushion, to be inappropriately translated to the unprotected articular surfaces. Biomechanical cadaveric studies have displayed increased contact pressures of 80–90% with meniscectomy, progressively increasing with size of the resection while contact stress forces have been shown to increase by 65% in partial meniscectomy of small bucket handle meniscal tears [38,39,40]. Increased contact stress and knee adduction moment are believed to lead to premature cartilage damage and progression to tibiofemoral osteoarthritis. While a necessary option in some patients, the documented risk of osteoarthritis and the successful outcome of meniscus repair should urge surgeons to perform partial meniscectomy repair in limited number of pediatric patients.
Meniscal allograft transplantation is a salvage procedure recommended for patients with a symptomatic meniscal deficient knee. In adults, a survivorship of 82.3% of transplants was reported at a mean of 8.6 years with a significant improvement in postoperative Lysholm scores by 17.7 points (p < 0.001), IKDC scores by 15.6 points (p = 0.01), and Oxford Knee score by 8 points (p = 0.031) [41•]. A recent study in 36 patients less than 16 years old (mean age 15.4, range 13–16) demonstrated an improvement in functional outcomes with a meniscal reoperation rate of 6%, and an overall reoperation rate of 22%, most of those being for associated chondral disorders [42•]. An improvement of preoperative Lysholm score from 43.8 to 74.6 and of preoperative IKDC score from 40.2 to 81.8 has been reported postoperatively, indicating that meniscus allograft transplantation can offer beneficial outcomes [42•]. Considering the potential benefit of delay or prevention of osteoarthritis in the knee, with associated high rate of transplant success, meniscal allograft transplantation is a reliable option for meniscus deficient patients.
Conclusions
Meniscus repair in children has shown to demonstrate a healing rate ranging from 33 to 100%, with most studies showing a clinical success rate in more than 70% of patients. While increased rates of healing were reported during the performance of concomitant ACL reconstruction, further research is necessary to clarify the exact role of ACL reconstruction in meniscus healing. Tear configuration can affect healing rate, with complex and bucket handle tears demonstrating a higher risk of failure, while tears in the lateral meniscus and skeletal immaturity have suggested favorable, yet inconsistent outcomes in the literature. Alternatives exist in cases where repair is not possible; however, based on the favorable medium-term and long-term outcomes reported, repair should be considered as the primary treatment option for most meniscal tears in children.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
McConkey MO, Bonasia DE, Amendola A. Pediatric anterior cruciate ligament reconstruction. Curr Rev Musculoskelet Med. 2011;4(2):37–44.
Stanitski CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in children and adolescents. J Pediatr Orthop. 1993;13(4):506–10.
Bellisari G, Samora W, Klingele K. Meniscus tears in children. Sports Med Arthrosc Rev. 2011;19(1):50–5.
Carter CW, Kocher MS. Meniscus repair in children. Clin Sports Med. 2012;31(1):135–54.
• Ferrari MB, Murphy CP, Gomes JLE. Meniscus repair in children and adolescents: a systematic review of treatment approaches, meniscal healing, and outcomes. J Knee Surg. 2018. This recent systemic review analyzed the available literature for meniscus repairs and concluded that meniscus repair in children is associated with good to excellent outcomes.
Merkel DL. Youth sport: positive and negative impact on young athletes. Open Access J Sports Med. 2013;4:151–60.
Mintzer CM, Richmond JC, Taylor J. Meniscal repair in the young athlete. Am J Sports Med. 1998;26(5):630–3.
Vanderhave KL, Moravek JE, Sekiya JK, Wojtys EM. Meniscus tears in the young athlete: results of arthroscopic repair. J Pediatr Orthop. 2011;31(5):496–500.
Starke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy. 2009;25(9):1033–44.
Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–69.
Andrish JT. Meniscal injuries in children and adolescents: diagnosis and management. J Am Acad Orthop Surg. 1996;4(5):231–7.
Hede A, Jensen DB, Blyme P, Sonne-Holm S. Epidemiology of meniscal lesions in the knee. 1,215 open operations in Copenhagen 1982-84. Acta Orthop Scand. 1990;61(5):435–7.
• Mitchell J, Graham W, Best TM, Collins C, Currie DW, Comstock RD, et al. Epidemiology of meniscal injuries in US high school athletes between 2007 and 2013. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):715–22. This study evaluated 1082 meniscal injuries in high school athletes and reported a rate of 5.1 meniscus injury per 100,000 athletes and highlighted associations with gender, sport, and type of exposure.
Mosich GM, Lieu V, Ebramzadeh E, Beck JJ. Operative treatment of isolated meniscus injuries in adolescent patients: a meta-analysis and review. Sports Health. 2018;10(4):311–6.
Shelbourne KD, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 2003;31(5):718–23.
Wasserstein D, Dwyer T, Gandhi R, Austin PC, Mahomed N, Ogilvie-Harris D. A matched-cohort population study of reoperation after meniscal repair with and without concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(2):349–55.
Krych AJ, McIntosh AL, Voll AE, Stuart MJ, Dahm DL. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36(7):1283–9.
Lucas G, Accadbled F, Violas P, Sales de Gauzy J, Knorr J. Isolated meniscal injuries in paediatric patients: outcomes after arthroscopic repair. Orthop Traumatol Surg Res. 2015;101(2):173–7.
Accadbled F, Cassard X, Sales de Gauzy J, Cahuzac JP. Meniscal tears in children and adolescents: results of operative treatment. J Pediatr Orthop B. 2007;16(1):56–60.
Kraus T, Heidari N, Svehlik M, Schneider F, Sperl M, Linhart W. Outcome of repaired unstable meniscal tears in children and adolescents. Acta Orthop. 2012;83(3):261–6.
Noyes FR, Chen RC, Barber-Westin SD, Potter HG. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39(5):1008–17.
Scott GA, Jolly BL, Henning CE. Combined posterior incision and arthroscopic intra-articular repair of the meniscus. An examination of factors affecting healing. J Bone Joint Surg Am. 1986;68(6):847–61.
Schmitt A, Batisse F, Bonnard C. Results with all-inside meniscal suture in pediatrics. Orthop Traumatol Surg Res. 2016;102(2):207–11.
Bloome DM, Blevins FT, Paletta GA Jr, Newcomer JK, Cashmore B, Turker R. Meniscal repair in very young children. Arthroscopy. 2000;16(5):545–9.
Krych AJ, Pitts RT, Dajani KA, Stuart MJ, Levy BA, Dahm DL. Surgical repair of meniscal tears with concomitant anterior cruciate ligament reconstruction in patients 18 years and younger. Am J Sports Med. 2010;38(5):976–82.
Cannon WD Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20(2):176–81.
Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94(24):2222–7.
Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27(9):1275–88.
Shakespeare DT, Rigby HS. The bucket-handle tear of the meniscus. A clinical and arthrographic study. J Bone Joint Surg Br. 1983;65(4):383–7.
Kramer DE, Micheli LJ. Meniscal tears and discoid meniscus in children: diagnosis and treatment. J Am Acad Orthop Surg. 2009;17(11):698–707.
Manzione M, Pizzutillo PD, Peoples AB, Schweizer PA. Meniscectomy in children: a long-term follow-up study. Am J Sports Med. 1983;11(3):111–5.
Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthop Surg. 1996;4(4):191–200.
Fields LK, Caldwell PE 3rd. Arthroscopic saucerization and repair of discoid lateral meniscal tear. Arthrosc Tech. 2015;4(2):e185–8.
Yoo WJ, Jang WY, Park MS, Chung CY, Cheon JE, Cho TJ, et al. Arthroscopic treatment for symptomatic discoid meniscus in children: midterm outcomes and prognostic factors. Arthroscopy. 2015;31(12):2327–34.
• Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015;31(5):867–73. This study evaluated arthroscopic reshaping of symptomatic discoid menisci at an average time of 10.1 years with overall satisfactory outcome. However, in approximately 40% of the patients progressive degenerative changes occurred.
Ahn JH, Lee SH, Yoo JC, Lee YS, Ha HC. Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy. 2008;24(8):888–98.
• Kocher MS, Logan CA, Kramer DE. Discoid lateral meniscus in children: diagnosis, management, and outcomes. J Am Acad Orthop Surg. 2017;25(11):736–43. This study provides a comprehensive description of the characteristics of the lateral discoid meniscus and outlined the algorithm of management of discoid lateral meniscus in children.
Bedi A, Kelly N, Baad M, Fox AJ, Ma Y, Warren RF, et al. Dynamic contact mechanics of radial tears of the lateral meniscus: implications for treatment. Arthroscopy. 2012;28(3):372–81.
Koh JL, Yi SJ, Ren Y, Zimmerman TA, Zhang LQ. Tibiofemoral contact mechanics with horizontal cleavage tear and resection of the medial meniscus in the human knee. J Bone Joint Surg Am. 2016;98(21):1829–36.
Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14(4):270–5.
• Mahmoud A, Young J, Bullock-Saxton J, Myers P. Meniscal allograft transplantation: the effect of cartilage status on survivorship and clinical outcome. Arthroscopy. 2018;34(6):1871–6 e1. This study evaluated the survivorship of meniscal allograft transplantations and reported an 18% failure at an average of 6 years postoperatively, all occurring in patients with Outerbridge Cartilage Score of 3 to 4. This study demonstrated the importance of cartilage status for meniscal allograft transplant survivorship.
• Riboh JC, Tilton AK, Cvetanovich GL, Campbell KA, Cole BJ. Meniscal allograft transplantation in the adolescent population. Arthroscopy. 2016;32(6):1133–40 e1. This study evaluated the outcome of meniscus transplantation in 36 children with a mean age of 15.4 and reported significant improvements in KOOS, Lysholm, and IKDC scores. Interestingly, the meniscal reoperation rate was 6% and the overall reoperation rate was 22%, most of them being for chondral disease.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Brian W. Yang, Elizabeth S. Liotta, and Nikolaos Paschos each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Orthopedics
Rights and permissions
About this article
Cite this article
Yang, B.W., Liotta, E.S. & Paschos, N. Outcomes of Meniscus Repair in Children and Adolescents. Curr Rev Musculoskelet Med 12, 233–238 (2019). https://doi.org/10.1007/s12178-019-09554-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-019-09554-6