Abstract
Femoroacetabular impingement (FAI) is a condition increasingly being recognized as a cause of hip pain and disability. Hip arthroscopy is a common method used to treat this condition. The purpose of this review was to identify reported radiographic outcomes after arthroscopic surgery for FAI. Online databases (PubMed, EMBASE, and Medline) were screened for studies involving arthroscopic management of FAI. Full-text reviews of eligible studies were conducted. We identified 23 eligible studies involving 1348 patients from an initial screen of 1304 studies involved. There were 15 different radiographic parameters among the 23 studies. The most commonly reported radiographic outcomes included the alpha angle (69.6 %), center edge angle (34.7 %), and femoral offset ratio (17.4 %). This study highlights the significant variation in reported radiographic outcomes after arthroscopic FAI surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Femoroacetabular impingement (FAI) is a condition increasingly being recognized as a cause of hip pain and disability in the active patient, as well as one of the risk factors of osteoarthritis of the hip in non-dysplastic patients [1–3]. The concept of FAI, as initially described by Ganz [3, 4], involves the abnormal contact between the femoral head and the acetabulum. Thus, a primary bone lesion predisposes to soft tissue injury, such as labral tearing or chondral delamination. Three different types of FAI have been described: CAM, Pincer, and mixed impingement. CAM impingement involves a non-spherical femoral head abutting the acetabular rim. Pincer impingement involves a prominent acetabular rim abutting a normally shaped femoral head [3, 4]. Mixed impingement involves varying degrees of both CAM and Pincer impingement in the same patient. This mixed impingement is the most common pattern seen in FAI patients [5].
FAI is a complex diagnosis involving pathology at various locations within the hip joint. Several radiographic measurements have been described to quantify the severity of the disease in symptomatic hips. These include the alpha angle, center edge angle, femoral offset, presence of a crossover sign, etc. To make the diagnosis, the clinician must combine several radiographic parameters with findings on clinical examination.
Numerous surgical options have been described to treat symptomatic FAI. These can be classified into three main categories: (1) open surgical dislocation, (2) arthroscopic assisted combined with an open component, and (3) arthroscopy alone. Hip arthroscopy is increasingly being utilized, given the potential advantages of reduced surgical trauma and decreased morbidity. A recent review of the American Board of Orthopaedic Surgeons database showed an eightfold increase in the number of hip arthroscopies performed between 1999 and 2004 [6].
Reported short-term clinical outcomes after FAI surgery are generally shown to be favorable in most clinical series [7–9]. Unfortunately, radiographic outcomes are not as consistently reported in the literature [10•]. The purpose of this systematic review was to identify reported radiographic outcome measures used in arthroscopic FAI surgical studies. We hypothesized that there is high variability among surgical studies in reporting of radiographic outcomes.
Methods
Search strategy
The online databases PubMed, EMBASE, and Medline were used to search for literature addressing radiographic outcomes after FAI correction reported in clinical studies from database inception until January 7, 2016. The search terms “femoral acetabular impingement”/“femoroacetabular impingement”, and “arthroscopy” were used (Appendix A).
Study screening
Two reviewers (J.K. and M.M.) independently screened the titles, abstracts, and full-text articles. Any disagreements were discussed between the reviewers until consensus was reached, and a senior author was included for consultation when necessary. The references of the eligible, included studies were then screened to capture any additional articles that may have eluded the initial search strategy.
Assessment of study eligibility and quality
The research questions and inclusion and exclusion criteria were determined a priori. The inclusion criteria were studies on human adults 18 years or older, English-language studies, studies on arthroscopic FAI surgery, and studies with reporting of postoperative radiographic data. All levels of evidence were included. The exclusion criteria were studies reporting on patients that had arthroscopic surgery with no bony work (i.e., no change in radiographic parameters from preoperative values), non-human studies, cadaveric studies, conference papers, book chapters, review articles, and technical reports. The methodological index for nonrandomized studies (MINORS) checklist was used by two independent reviewers to assess the quality of the methodology used by the included studies [11]. Non-comparative studies are assessed out of a maximal MINORS score of 16, while comparative studies are assessed out of a maximal MINORS score of 24.
Data abstraction and statistical analysis
Relevant data were abstracted and recorded in a Microsoft Excel spreadsheet (Version 2007, Microsoft Inc, Redmond, WA, USA). Recorded data included details on the characteristics of the included studies such as authors, country, year of publication, sample size, and study design. Specifics regarding the reported radiographic outcomes were then extracted from each study. Descriptive statistics (including means, medians, standard deviations, and ranges) were used to summarize the data.
Assessment of agreement
In order to assess the inter-reviewer agreement, a kappa (k) statistic was calculated for the title, abstract, and full-text screening stages. Agreement was categorized a priori as follows: k of 0.61 or greater was considered substantial agreement; k of 0.21 to 0.60, moderate agreement; and k of 0.20 or less, slight agreement. Agreement for quality assessment using the MINORS score was determined using an intraclass correlation coefficient (ICC). An ICC less than 0.25 was considered to indicate little to no agreement, 0.25 to 0.50 fair agreement, 0.50 to 0.75 moderate agreement, and greater than 0.75 was considered to indicate high agreement [12].
Results
Search strategy
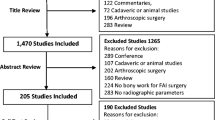
The initial search of three databases resulted in 1304 total studies. Three-hundred thirty-nine duplicates were removed. A systematic screening approach resulted in 23 available full-text articles for review (Fig. 1). There was substantial agreement among reviewers at the title (k = 0.817; 95 % CI, 0.785–0.849), abstract (k = 0.876; 95 % CI, 0.824–0.928), and full-text (k = 1.00) screening stages.
Study characteristics
All included studies were conducted between 2007 and 2015. Table 1 lists descriptive characteristics of the studies included for analysis. The articles included in this review involved a total of 1348 patients. Twenty of the studies involved arthroscopic management, while three of the studies compared arthroscopic management with open surgical treatment [28, 30, 31]. Of the studies included, 15 were conducted in the USA and three in Switzerland. The remaining five studies were conducted in France (two), Chile (one), China (one), and Mexico (one). The mean sample size was 57.8 patients.
Study quality
We identified five level II studies (two prospective comparative studies, two lesser-quality randomized controlled trials, and one prospective matched-pair comparative study) (21.7 %), five level III studies (three cohort studies, one retrospective comparative study, and one retrospective case series) (21.7 %), and 13 level IV studies (nine case series, three therapeutic case series, and one prospective cohort study) (60.9 %). There were no level I studies identified. The level of inter-rater agreement in the assessment of quality using the MINORS score was high with an ICC of 0.93 (95 % CI 0.83–0.97). The median MINORS score of the non-comparative studies was 10/16 (range 7/16 to 13/16). For comparative studies, the median MINORS score was 17.5/24 (range 12/24 to 21/24). The factor most consistently reported was a clearly stated aim, which was reported by 20 (87 %) of the studies. The factor that was least consistently identified was prospective calculation of sample size, which was reported by only 5 (22 %) of the studies (Table 1).
Radiographic outcomes
Across all the studies, 15 different radiological outcomes were reported postoperatively (Table 2). The alpha angle was the most frequently reported postoperative radiographic outcome (16 studies, 69.6 %). For these studies that reported postoperative alpha angles, seven studies indicated that lateral images were used to calculate alpha angle (with frog-leg lateral, cross-table lateral, and Dunn view all being mentioned). Two studies mentioned that anteroposterior (AP) images were used to calculate alpha angle. For the remaining studies, there was no mention on what view was used. Center edge angle on postoperative radiographs was used in eight studies (34.7 %). Femoral offset was measured in four studies (17.4 %). Tonnis classification was mentioned in three studies (13 %). Tonnis angle and resection depth ratio (%) was mentioned in two studies (8.7 %). Other radiographic outcomes measured included ischial prominence size (mm), presence of crossover sign, anterior rim angle, anterior wall angle, anterior margin ratio, resection depth (mm), beta angle, sector of resection, and acetabular bony impingement angle.
Eight studies reported multiple measures in their results [20, 21, 23, 25, 26, 28, 29, 31]. Of these, five reported outcomes for both CAM and Pincer radiographic outcomes in the same study [20, 25, 26, 29, 31]. Three studies included magnetic resonance imaging (MRI) as part of their postoperative imaging protocol [22, 26, 31], while three other studies utilized computed tomography (CT) scan as part of their postoperative imaging protocol [27, 29, 32]. Table 2 shows radiographic outcomes for the included studies.
CAM-type FAI
Alpha angle was the most commonly reported radiographic outcome for CAM deformities, reported in 16 studies. The pooled mean ± standard deviation for postoperative alpha angle was 45.6° ± 8.2 (range 36.4–68.5°) [8, 14–16, 18–20, 22, 23, 25–32]. The second most commonly reported radiographic outcome for CAM deformities was femoral offset reported in four studies. The pooled mean ± standard deviation for postoperative femoral offset was 8.8 mm ± 0.9 mm (range 7.8–9.56 mm) [20, 23, 28, 31]. The resection depth ratio reported in two studies to be 13.2 % (osteochondroplasty group) versus 21.8 % (femoral neck fracture group) [23], and 6 % [31]. Mean change from preoperative values to postoperative values could not be calculated due to wide variation in how the data was presented.
Pincer-type FAI
Center edge angle was the most commonly reported radiographic outcome for Pincer-type FAI, reported in eight studies. The pooled mean ± standard deviation for postoperative center edge angle was 34.1° ± 6.2° (range 30.3–35.9°) [13, 17, 21, 25, 26, 29, 31, 33]. The second most commonly reported radiographic outcome for Pincer impingement was the Tonnis angle reported in two studies to be 8.2 ± 3.4° [21] and 3.1° [25]. Mean change from preoperative values to postoperative values could not be calculated due to wide variation in how the data was presented.
Discussion
Interest in FAI has increased over the last decade, which has led to an increase in the number of hip arthroscopy procedures being performed [6]. Unfortunately, there is a paucity of strong level 1 or 2 evidence studying clinical outcomes after FAI surgery. There is even less literature studying postoperative radiographic parameters and how these relate to clinical outcomes in the long term [10]. Reporting postoperative radiographic outcomes has been shown to be important as it may predict outcome following the index surgical procedure, while under-correction of bony pathology has been identified as a leading cause of failure in these patients [35•, 36•].
A full comprehensive radiographic assessment of FAI involves a true AP pelvis, false-profile, cross-table lateral, frog-leg lateral, and a 45° lateral Dunn view in order to extrapolate spherical pathology from one-dimensional imaging [37]. In addition, the pathology can be quite complex involving abnormal bony changes on the femoral head, acetabulum, or both. This systematic review explores the consistency of radiographic outcomes after arthroscopic management of FAI. Given the heterogeneity of pathology seen with FAI, it is not surprising that studies report a wide variety of radiographic outcomes postoperatively.
There was substantial variability among the studies reviewed when comparing postoperative radiographic outcomes reporting of both CAM and Pincer-type FAI. Fifteen different outcomes were described among the studies included (Table 2). The alpha angle was the most commonly reported outcome. Even with the alpha angle, there was heterogeneity in how the measurement was calculated. Two studies calculated the alpha angle on AP radiographs. Seven studies indicated that lateral images were used to calculate the alpha angle, with frog-leg lateral, cross-table lateral, and Dunn views all being mentioned as views used to calculate the alpha angle. It is difficult for a surgeon to compare their results with the literature when there is such heterogeneity in reporting postoperative images. Given that FAI is a complex morphological alteration of the hip joint, it is not possible to have one postoperative radiographic parameter that can be inclusive of all the correction that has been performed. Although there was variability in how alpha angle was calculated, this measure was consistently used in papers that reported on CAM impingement. Of 16 papers that report on CAM impingement, all the 16 included alpha angle as part of their analysis. Similarly for Pincer-type, eight of ten papers that report on this form of impingement use center edge angle as part of their analysis. There is not the same heterogeneity in calculating center edge angle compared to alpha angle. This angle was consistently calculated on AP radiographs of the pelvis.
There were limitations with this study. This review is limited both by the number of studies available and the quality of these studies. This review looked solely at studies published in the English language. As such, there may be a publication bias. No attempt was made to contact the authors of the included studies to ensure data accuracy. It is possible that patients were included in more than one publication and therefore counted more than once in this study.
There are several strengths to this review. Our search strategy was comprehensive in its review of the literature. We used focused and clear inclusion and exclusion criteria to define our research question. We included multiple reviewers when screening, evaluating, and abstracting the data from the literature. This study provides a novel focus on radiographic outcomes following arthroscopic management of FAI relative to the increasing body of literature on clinical outcomes. This review is thorough, containing literature from North America, Europe, South America, and Asia.
Future studies should aim to standardize radiographic outcome reporting and combine these with clinical outcomes. Large-scale clinical trials that attempt to explore clinical outcomes combined with radiographic outcomes should be used to determine successful FAI management. Ideally, outcomes would be reported using plain radiographs so as to minimize cost and radiation exposure to the patient. For this to be possible, correlation of plain imaging to advanced imaging (3-D CT scan, MRI, etc.) would need to be established. Computer templating software would be an instrumental tool for a surgeon to accurately plan the amount and location of resection in order to maximize clinical outcomes.
Conclusions
There is significant variation in the reported radiographic outcomes after arthroscopic FAI surgery, with the vast majority of studies not reporting these values. Alpha angle was the most commonly reported outcome for correction of femoral-sided deformity, while center edge angle was the most commonly reported outcome for acetabular deformity. No single radiographic parameter is sufficient in diagnosing FAI. The clinician must use a combination of radiographic values in conjunction with clinical examination to make an accurate diagnosis. This study highlights the need for consistent radiographic outcome reporting in conjunction with clinical outcomes after arthroscopic FAI surgery.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ito K, Minka II MA, Leunig M, et al. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg (Br). 2001;83:171–6.
Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–7.
Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–20.
Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–72.
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg (Br). 2005;87:1012–8.
Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94, e23.
Byrd JW, Jones KS, Gwathmey FW. Femoroacetabular impingement in adolescent athletes: outcomes of arthroscopic management. Am J Sports Med. 2016
Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24(5):540–6.
Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39(Suppl):7S–13.
Hetaimish BM, Khan M, Crouch S, Simunovic N, Bedi A, Mohtadi N, et al. Consistency of reported outcomes after arthroscopic management of femoroacetabular impingement. Arthroscopy. 2013;29(4):780–7. Recent review studying consistency of both clinical and radiographic outcomes in the literature. Important study in that highlights the lack of consistency in outcome reporting with FAI surgery.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–6.
Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 2nd ed. Upper Saddle River: Prentice Hall Health; 2000. p. 90–3.
Philippon MJ, Wolff AB, Briggs KK, Zehms CT, Kuppersmith BS. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy. 2010;26(6):757–61.
Kelly BT, Bedi A, Robertson CM, Dela Torre K, Giveans MR, Larson CM. Alterations in internal rotation and alpha angles are associated with arthroscopic cam decompression in the hip. Am J Sports Med. 2012;40(5):1107–12.
Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40(5):1015–21.
Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25(4):369–76.
Safran MR, Epstein NP. Arthroscopic management of protrusio acetabuli. Arthroscopy. 2009;29(11):1777–82.
Ilizaliturri VM, Nossa-Barrera JM, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg (Br). 2007;89-B(8):1025–30.
Wylie JD, Beckman JT, Maak TG, Aoki SK. Arthroscopic treatment of mild to moderate deformity after slipped capital femoral epiphysis: intra-operative findings and functional outcomes. Arthroscopy. 2015;31(2):247–53.
Gupta A, Redmond JM, Stake CE, Finch NA, Dunne KF, Domb BG. Does the femoral cam lesion regrow after osteoplasty for femoroacetabular impingement?: two-year follow-up. Am J Sports Med. 2014;42(9):2149–55.
Gross CE, Hellman M, Freedman R, Hart M, Reddy A, Salata M, et al. Effect of anterior acetabular rim recession on radiographic parameters: an in vivo study. Arthroscopy. 2013;29(8):1292–6.
Brunner A, Horisberger M, Herzon RF. Evaluation of a computer tomography-based navigation system prototype for hip arthroscopy in the treatment of femoroacetabular cam impingement. Arthroscopy. 2009;25(4):382–91.
Zingg PO, Buehler TC, Poutawera VR, Alireza A, Dora C. Femoral neck fractures after arthroscopic femoral neck osteochondroplasty for femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:926–31.
Gicquel T, Gedouin JE, Krantz N, May O, Gicquel P, Bonin N. Function and osteoarthritis progression after arthroscopic treatment of femoro-acetabular impingement: a prospective study after a mean follow-up of 4.6 (4.2-5.5) years. Orthop Traumatol Surg Res. 2014;100(6):651–6.
Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39 Suppl 1:14S–9.
Rafols C, Monckeberg JE, Numair J, Botello J, Rosales J. Platelet-rich plasma augmentation of arthroscopic hip surgery for femoroacetabular impingement: a prospective study with 24-month follow-up. Arthroscopy. 2015;31(10):1886–92.
Zhuo H, Wang X, Liu X, Song G, Li Y, Feng H. Quantitative evaluation of residual bony impingement lesions after arthroscopic treatment for isolated pincer-type femoroacetabular impingement using three-dimensional CT. Arch Orthop Trauma Surg. 2015;135:1123–30.
Bedi A, Zaltz I, De La Torre K, Kelly BT. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39 Suppl 1:20S–8.
Ross JR, Larson CM, Adeoyo O, Kelly BT, Bedi A. Residual deformity is the most common reason for revision hip arthroscopy: a three-dimensional CT study. CORR. 2015;473:1388–95.
Domb BG, Stake CE, Botser IB, Jackson TJ. Surgical dislocation of the hip versus arthroscopic treatment of femoroacetabular impingement: a prospective matched-pair study with average 2-year follow-up. Arthroscopy. 2013;29(9):1506–13.
Zingg PO, Ulbrich EJ, Buehler TC, Kalberer F, Poutawera VR, Dora C. Surgical hip dislocation versus hip arthroscopy for femoroacetabular impingement: clinical and morphological short-term results. Arch Orthop Trauma Surg. 2013;133:69–79.
Bedi A, Dolan M, Hetsroni I, Magennis E, Lipman J, Buly R, et al. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med. 2011;39 Suppl 1:43S–9.
Larson CM, Stone RM. The rarely encountered rim fracture that contributes to both femoroacetabular impingement and hip stability: a report of 2 cases of arthroscopic partial excision and internal fixation. Arthroscopy. 2011;27(7):1018–22.
Gedouin JE, Duperron D, Langlais F, Thomazeau H. Update to femoroacetabular impingement arthroscopic management. Orthop Traumatol Surg Res. 2010;96:222–7.
de Sa D, Urguhart N, Philippon M, Ye JE, Simunovic N, Ayeni OR. Alpha angle correction in femoroacetabular impingement. Knee Sports Traumatol Arthrosc. 2014;22(4):812–21. Recent review looking at clinical outcomes associated with alpha angle correction. Review suggests that correction to less than 55° leads to improved patient outcomes. Highlights the importance in stressing radiographic measures in helping to predict patient outcome.
Sardana V, Philippon MJ, de Sa D, Redi A, Ye L, Simunovic N, et al. Revision hip arthroscopy indications and outcomes: a systematic review. Arthroscopy. 2015;31(10):2047–55. Recent review looking at indications and outcomes of revision hip arthroscopy. Review suggests that residual deformity is a predictor of requiring revision surgery. Again, highlights the importance of using radiographic measures to ensure adequate bony resection of deformity.
Clohisy JC, Dobson MA, Robison JF, Warth LC, Zheng J, Liu SS, et al. Radiographic structural abnormalities associated with premature, natural hip-joint failure. J Bone Joint Surg Am. 2011;93 Suppl 2:3–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in the preparation of this article.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Outcomes Research in Orthopedics
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Dzaja, I., Martin, K., Kay, J. et al. Radiographic outcomes reporting after arthroscopic management of femoroaceabular impingement: a systematic review. Curr Rev Musculoskelet Med 9, 411–417 (2016). https://doi.org/10.1007/s12178-016-9366-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-016-9366-3