Abstract
Purpose of Review
The 2020 Dietary Guidelines for Americans (DGA) recommends that American adults consume 2 to 3 daily servings of dairy foods as part of healthy dietary patterns. The DGA’s recommended dietary patterns are intended to meet nutrient needs and reduce the risk of chronic diseases, including overweight and obesity. However, the evidence reviews that the 2020 DGA is based on, the 2020 Dietary Guidelines Scientific Advisory Report, did not assess the body of evidence linking individual foods to adiposity. The purpose of this review is to assess the evidence published in the last 10 years on dairy consumption, adiposity, and satiety.
Recent Findings
The twenty studies included in this review, primarily randomized controlled trials, include interventions with the dairy foods recommended by the DGA—milk, cheese, and yogurt—of varying fat levels (whole fat, reduced fat (2%), low fat (1%), and fat free). Most of these studies were conducted in individuals who were overweight or had obesity at baseline. Therefore, these studies do not measure the impact of eating dairy foods on prevention of adiposity or obesity. Instead, they focus on whether dairy foods support weight loss/weight maintenance or how they affect satiety and prospective food consumption.
Summary
Overall, recent evidence indicates that consuming dairy foods does not increase risk of overweight or obesity in adults but also does not protect against adiposity. Solid and semi-solid dairy foods like cheese and yogurt may be more satiating than milk and other beverages, though more research is needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One approach that the field of nutrition science has adopted to understand the dietary drivers of overweight and obesity is to study the associations between the development of adiposity and intake of a specific food or food group. Accordingly, many studies have investigated the link between consuming dairy foods like milk, cheese, and yogurt with markers of adiposity. A body of research has also been dedicated to the links between consuming certain food groups, including dairy foods, and satiety, which drives food intake.
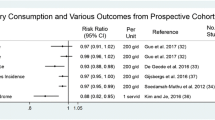
Previous reviews and meta-analyses on the associations between dairy intake and adiposity report conflicting results. A meta-analysis of randomized clinical studies published by Benatar et al. in 2013 [1] found that, while interventions that provided either low-fat or whole-fat dairy foods increased body weight, there was not a significant impact of either the low- or whole-fat dairy intake on other cardiometabolic outcomes including waist circumference (WC). However, this meta-analysis included studies that grouped butter, cream, and ice cream among “dairy foods,” which differs from the dairy foods recommended as part of healthy dietary patterns in the most recent official US dietary guidance, the 2020 Dietary Guidelines for Americans (DGA) [2]. In contrast, a systematic review of prospective cohort studies by Louie et al. [3] indicated that consuming dairy foods seemed to have a protective effect on the risk of overweight and obesity in children and adults. Another systematic review of studies on yogurt and weight management [4] indicated that there was not a significant impact of yogurt consumption on weight loss. However, Eales et al. indicated that yogurt may be connected to a lower BMI, lower body weight, less weight gain, a smaller WC, and lower body fat. Both systematic reviews [3, 4] stated that there was insufficient data to determine a causal relationship.
Since 2005, the DGA has recommended that Americans ages 9 and older consume 3 servings of dairy foods as part of healthy eating patterns intended to be protective of chronic diseases and health conditions, including overweight and obesity [2, 5,6,7]. However, while these recommendations were carried through in the 2020 DGA, the evidence review that the 2020 DGA is based on did not actually assess the evidence on specific foods and risk of obesity, focusing instead on overall eating patterns and their links to health outcomes such as excess weight gain. Because the recommendations in the 2020 DGA were based on dietary patterns research versus studies on individual foods, the purpose of this review is to assess the literature from the past 10 years on the impact of consuming dairy foods on adiposity and satiety [2].
Methods
This review focused on studies with interventions that included the dairy foods (milk, cheese, and yogurt) recommended by the DGA but was not restricted by fat level, so studies including whole-fat, reduced-fat (2%), low-fat (1%), and fat-free products were all eligible for inclusion. Trials that utilized dairy products fortified with nutrients or dietary components aside from vitamin A or vitamin D (standard fortificants for dairy foods in the USA) were not considered, as these products are not representative of typically available and consumed dairy foods in the USA. Trials conducted in individuals with multiple metabolic abnormalities and conditions, including the metabolic syndrome, were not included. Studies with participants who had obesity or type 2 diabetes but were otherwise generally healthy were included as these individuals are representative of the general adult population in the USA.
Search Strategy
This review used the following search terms in PubMed to identify articles: overweight OR adiposity OR abdominal adiposity OR abdominal obesity OR body mass index AND adult AND dairy product. Results were further filtered to include only those publications that describe clinical trials conducted in humans, with a full-text available, conducted in the last 10 years, published in the English language, and in adults ages 19 and older. An initial query yielded 260 studies. After a title review to remove duplicates and studies not fitting the criteria for this review, 92 studies remained, and after reviewing abstracts, 38 studies remained. Following a full-text review, 19 studies from the original query were included in this review. In addition to the studies obtained from the PubMed query, one additional study was added during the full-text review stage [8]. Included studies had to assess interventions or effects of milk, cheese, or yogurt, compared to a non-dairy control or placebo on an adiposity- or weight-related outcome including BMI, body composition, body weight, WC, waist-to-hip ratio (WHR), or a satiety-related outcome such as energy intake and subjective ratings of satiety using visual analog scales (VAS). Several studies on adiposity, including many of the studies in this review, evaluate multiple outcomes including postprandial glycemia and bone health markers, among others. In this review, only those outcomes relevant to adiposity and satiety will be discussed.
Results
The results of this literature review have been divided into two sections: studies that assess the links between consuming dairy foods with markers of adiposity and studies that assessed the impact of consuming dairy foods on satiety.
Body Weight and Body Composition
Fifteen studies assess the links between consuming dairy foods and markers of adiposity. These studies include 4 publications [8,9,10,11] on randomized crossover trials from 3 studies, 9 randomized controlled trials [12,13,14,15,16,17,18,19,20], one substudy of a randomized controlled trial [21], and one observational study [22]. These studies have also been summarized in Table 1.
The 4 randomized crossover trials included in this review all compared a high-dairy diet to a low-dairy diet in individuals who were overweight or had obesity and reported few differences in adiposity-related outcomes between the two interventions. In one randomized crossover trial [11], 45 overweight participants between 45 and 65 years of age consumed a high-dairy diet (5–6 servings of dairy foods daily) for 6 weeks and a low-dairy diet (less than 1 serving of dairy foods daily) with a 4-week washout in between treatments. While participants were advised to keep their caloric intake consistent, caloric intake during the high-dairy diet was slightly higher. Body weight was lower after the low-dairy diet (p=0.012), but there were no differences in WC, hip circumference (HC), body fat percentage, or lean mass between the two treatments [11]. A secondary outcome analysis of this same trial [10] with data from 52 participants reported similar results. Total energy intake was higher during the high-dairy diet (p=0.021). And, after the high-dairy diet, participants had a slightly higher body weight (p=0.008) and higher BMI (p=0.007), but there were no differences in HC, WC, or total body fat between the two interventions.
Another randomized crossover trial [9•] compared 6 months of high- and low-dairy diets on 23 healthy participants with BMIs within the overweight to obese range. Participants consumed 4 servings per day of dairy foods (high-dairy diet) or no more than 2 servings per day of dairy foods (low-dairy diet), while keeping their diets overall isocaloric with their pre-intervention eating patterns. There were no significant differences in body weight, WC, total body fat percentage, or abdominal body fat percentage after the two interventions. A similar randomized crossover trial [8] also had participants consume high- and low-dairy diets for 6 months each. The 36 adults ages 18 to 75 in this study were overweight or had obesity and typically consumed little dairy. Participants consumed 4 servings per day of reduced-fat dairy for 6 months and a low-dairy control diet (1 or fewer servings of dairy per day) for 6 months. Mean energy intake was higher during the high-dairy phase (p=0.004). However, after 6 months, there were no differences in WC, body weight, HC, BMI, total body fat, or abdominal fat. The authors concluded that dairy foods can be incorporated into the diet without weight or fat gain [8].
Results of the non-crossover studies reported some benefits to the dairy interventions compared to the controls. A trial of 135 postmenopausal overweight women or women with obesity found that women consuming 4–5 servings per day of low-fat dairy foods for 6 months as part of an energy-restricted weight loss diet saw a greater percentage decrease in WC, HC, and abdominal circumference than women either consuming a low-dairy diet (with calcium and vitamin D supplements) or taking placebo pills, though not all of the differences reached statistical significance [12•]. A similar trial conducted in 100 premenopausal women who were overweight or had obesity assigned participants to consume one of 4 hypocaloric diets for 8 weeks: control diet, control diet with 800 mg per day calcium supplement, a diet with three daily servings of low-fat milk, or a diet with 3 daily servings of calcium-fortified soy milk [19]. Body weight, BMI, WC, WHR, body fat mass, and percent body fat mass decreased in all groups, but including 3 servings of milk in the weight reduction diet led to greater reductions in BMI (compared to the control; p<0.01), weight (compared to the control; p<0.01), WC (compared to the control; p<0.01), and WHR (compared to the control; p<0.01). Changes in WC and WHR were also higher in the soy milk groups relative to the control (p<0.05).
A substudy of a randomized weight loss trial and an observational study also showed some benefits to consuming dairy foods for healthy weight maintenance. Champagne et al. [21] conducted a substudy with 828 participants who successfully achieved at least a 4-kg weight loss during a randomized controlled clinical trial. According to food frequency questionnaires administered at 12 and 30 months following the weight loss intervention, those individuals who increased low-fat dairy intake did not lose more weight during the trial but did maintain their weight post-trial. A cross-sectional study from Radavelli-Bagatini et al. [22] found that women (n=1456) ages 70 to 85 who consumed 1.5 or more servings of dairy foods per day had greater whole body lean mass (p=0.001) and appendicular skeletal muscle mass (p=0.002) than women consuming 1.5 or fewer servings per day both before and after multivariate adjustment for age, BMI, energy intake, physical activity, smoking, and alcohol consumption. There were no differences with body fat mass or BMI.
Yet, several more studies reported few or no differences on adiposity markers following interventions with dairy foods. A randomized controlled trial [14] assigned 65 women ages 18 to 49 with obesity to one of three hypocaloric diets: high-dairy (30 g low-fat cheese plus three glasses milk daily), low-dairy (30 g low-fat cheese plus one glass milk), or a control diet (30 g low-fat cheese) for 12 weeks and found no differences in body weight, BMI, HC, WC, WHR, or body composition measurements between the three groups. Bendtsen et al. [15•] compared hypocaloric high-dairy and low-dairy diets in 96 men and women who were either overweight or had obesity. At the end of the 24-week trial, there were no differences in weight, body composition, or WC between the two groups. Participants in the low-dairy group had a higher decrease in HC (p=0.003 after adjustments), but it was the only significant difference between the groups. Among 25 adults with obesity who regularly consumed less than 700 mg per day of calcium, following a high-dairy diet (4 servings per day) compared to a diet with 700 mg calcium from diet and 600 mg of calcium from supplements or a placebo for 21 weeks did not lead to any additional benefits for weight, BMI, or body composition [18]. Another trial comparing higher dairy intake (at least 711 mL per day of milk) with lower dairy intake (less than 238 mL per day of milk) as part of a hypocaloric dietary intervention over 12 weeks among 51 women with obesity found that baseline and end of intervention weight, fat mass, BMI, and WC did not differ between the two groups [20]. Finally, after forty-seven overweight adults were asked to consume either 1 L per day of diet cola, mineral water, cola, or an isocaloric serving of semi-skimmed milk for 6 months, total fat mass, total lean mass, and weight did not differ between the 4 beverage groups. Drinking regular cola did lead to higher visceral adipose tissue than the other drinks as well as greater relative accumulation of liver fat (p<0.05) and muscle fat (p<0.05) [13].
The two studies in this review that included an exercise component to their intervention found benefits of a dairy-rich intervention on fat mass loss and lean mass gain. Maltais et al. conducted a randomized controlled trial in 26 overweight men with sarcopenia and a BMI under 30 [16]. Participants completed 4 months of resistance exercise and consumed one of three isovolumetric and isocaloric postexercise shakes: control (rice milk), milk-based, and soy-based. While there were no differences in BMI measurements, the dairy group lost more fat mass and gained more muscle mass relative to fat mass (p< 0.05). Body weight increased in the soy group (p<0.05) [16]. A randomized controlled trial by Josse et al. [17] compared the impacts of three different diets—a high-protein/high-dairy diet (6–7 dairy servings per day), an adequate-protein/medium-dairy diet (3–4 dairy servings per day), and an adequate-protein/low-dairy diet (0–1 dairy servings per day) in 90 premenopausal overweight women or women with obesity for 16 weeks. Participants were asked to expend 250 kcal of energy in a workout session each day with 2 days per week of resistance exercise. There were no differences in total body mass decreases between the groups after the intervention. However, the high-dairy group lost more fat mass and gained more lean mass (p<0.05) over the 16 weeks compared to the other two groups. During weeks 8 to 16, the high-dairy group gained more lean mass than the medium- (p>0.05) and low-dairy groups (p<0.01). The medium-dairy group did not change their lean mass, and the low-dairy group lost lean mass (p<0.05). The high-dairy group also lost more trunk fat (p<0.005) and visceral adipose tissue volume (p<0.05) than the low-dairy group. The authors concluded that higher protein and dairy intakes led to “more favorable body composition changes in women characterized by greater total and visceral fat loss and lean mass gain” [16].
Satiety
Five randomized crossover trials also assessed the impact of dairy intake (milk, yogurt, and/or cheese) on satiety, when compared to water, soy beverage, cola, diet cola, orange juice, crackers, and chocolate. These studies are summarized below and in Table 2.
When dairy foods were compared, in two separate randomized crossover trials, cheese and yogurt had greater appetite-suppressant impacts than either milk, water, or soy beverage, but there were no differences between the dairy foods on energy intake at subsequent ad libitum meals [23, 24]. In one trial [23], dairy snacks (isocaloric and isovolumetric amounts of milk, yogurt, and cheese) or water was provided to 32 overweight men after a standardized breakfast. VAS ratings of satiety (hunger, fullness, desire to eat, prospective food consumption) were assessed at regular intervals and energy intake was assessed with an ad libitum pasta lunch provided 90 min after the dairy snacks. All dairy snacks reduced appetite and energy intake at the ad libitum lunch compared to water, but yogurt had the greatest suppressant effect on appetite ratings overall, followed by cheese, milk, and water. Fullness was higher and prospective food consumption was lower after yogurt versus milk and water but was not different from cheese. Another trial [24] compared the satiety impacts of 2% milk, soy beverage, 2% Greek yogurt, or cheddar cheese consumed as part of an isocaloric (380 kcal) meal with bread and jam with water (served by itself) as a control. Participants completed VAS ratings of satiety at regular intervals and, after 180 min, were provided an ad libitum rice and meat sauce meal. Although there were no differences in food or energy intake at the ad libitum meal, all treatments led to higher fullness than water, and yogurt led to higher fullness than milk. Yogurt and cheese suppressed appetite and desire to eat more than milk and water and lowered appetite more than milk and soy beverage. Cheese reduced prospective food consumption compared with water and milk.
In a third randomized crossover trial, 20 young women with normal BMIs found that eating yogurt led to greater reductions in hunger but no differences in fullness compared to eating an isocaloric amount of chocolate [26]. In this study, eating yogurt also delayed eating by 30 min compared to chocolate and led to lower caloric consumption at a subsequent ad libitum meal [26]. Another randomized crossover trial had participants (n=24 adults who were overweight or had obesity) consume a standardized evening meal the night before the intervention, arrive fasted, and consume 500 mL of either a cola beverage, semi-skimmed milk, diet cola, or mineral water. Four hours after drinking the beverages, participants were provided an ad libitum pizza lunch. Satiety was assessed with VAS scales and energy intake was evaluated with the pizza lunch. Compared to drinking cola, drinking milk led to greater subjective fullness and less hunger, but there were no differences in energy intake between groups at the pizza meal, meaning that the energy from the caloric beverages was not compensated for at the subsequent meal [25]. Similarly, when compared to an isovolumetric amount of orange juice, fat-free yogurt (flavored with strawberry or honey) and skim milk consumed by 18 healthy young men did not have different impacts on either VAS satiety ratings or energy intake at an ad libitum pizza meal provided 120 min after the dairy and orange juice treatments [27].
Discussion
While the adiposity-focused studies in this review used different methods, their conclusions are similar. The four publications of randomized crossover trials compared the impacts of a high-dairy diet and a low-dairy diet and found few differences between the two dietary interventions on adiposity measures [8,9,10,11]. The randomized controlled trials and the single substudy of a randomized controlled trial echo these findings. Most of the studies reported no differences or minimal differences [13,14,15, 18, 20] between a dairy-rich intervention and control interventions, which included soft drinks, water, and “low-dairy” diets, on measures of adiposity.
Some studies focused on either weight loss or weight loss maintenance did find a benefit to including 3–5 servings of dairy foods or their nutrients (especially calcium and vitamin D) in weight loss diets compared to a placebo [12•] or soy milk [19]. Including dairy foods did also help participants in one study maintain their weight loss [21]. The two studies in this review that included exercise interventions also both found that the dairy or “high-dairy” groups had greater increases in lean mass gain and greater fat mass loss compared to other groups with non-dairy interventions or low-dairy interventions [16, 17]. While consuming dairy foods may not in itself offer benefits for body composition or weight loss, when paired with resistance exercise or a hypocaloric diet, consuming at least the amounts of dairy foods recommended by the DGA may help support weight loss, lean mass gain, fat mass loss, and weight maintenance. More research is needed on these topics, however, especially with more diverse cohorts. Most of these studies [8,9,10,11,12,13,14,15, 17,18,19,20,21, 23, 25] were conducted in individuals who were overweight or had obesity at baseline. Only four of the studies included in this review assessed the impacts of dairy intake in normal-weight individuals [22, 24, 26, 27]. This review does not include adequate information to assess the ability of dairy intake to prevent overweight or obesity.
Satiety, the postprandial state that inhibits hunger and further eating, influences food intake and, therefore, can affect weight status and maintenance [28, 29]. Most ratings of satiety rely on human participants to subjectively assess their own sensations of fullness and appetite using VAS. Energy intake at an ad libitum meal is also commonly used as a quantitative assessment of satiety. However, there is not a systematic way to pair this subjective and quantitative data together when the results do not align. For instance, in this review, when the satiating impacts of dairy foods were compared in two separate randomized crossover trials, cheese and yogurt had greater appetite-suppressant abilities than milk, water, or soy beverage. However, these differences did not extend to energy intake at subsequent ad libitum meals [23, 24]. While participants reported feeling less hungry after eating yogurt and cheese, this subjective reporting was not reflected in actual energy intake. Therefore, while the authors of these studies concluded that yogurt and cheese were more satiating than milk and other beverages, the data indicates a more complex relationship.
In addition, these studies on satiety assess the satiating properties of dairy foods relative to other foods, like water, soy beverage, cola, diet cola, crackers, chocolate, and orange juice, which makes it challenging to draw conclusions about how satiating milk, cheese, and yogurt are. Furthermore, dairy foods were not always compared to similar foods. In the two studies that found that cheese and yogurt exerted a greater impact on subjective satiety measures [23, 24], cheese and yogurt—a solid and a semi-solid food—were compared to beverages that did not necessarily have the same macronutrient profile either. More research is needed in this area that compares foods with more similar physical structures, as previous evidence in satiety research indicates that food form and the role of different foods in an eating occasion context have an impact on perceived satiety, as does macronutrient content [30,31,32].
Conclusions
Dairy foods do not appear to exert a unique role in weight loss or weight gain. While some previous studies have indicated a more straightforward relationship between consuming dairy foods and adiposity [33,34,35], the body of more recent research discussed in this review indicates that the relationship between dairy foods and adiposity remains incompletely understood. Dairy foods do not seem to increase adiposity in overweight adults and adults with obesity, and cheese and yogurt may be more satiating than milk. To apply the findings in this review in a clinical setting, clinicians could counsel their patients that while dairy foods provide important nutrients in recommended healthy dietary patterns, they do not appear to either increase weight gain or promote weight loss. Additionally, clinicians could share that, based on subjective measures, solid and semi-solid dairy foods like cheese and yogurt may be more satiating than liquid ones, like milk, as well as other beverages and less nutrient-dense foods.
Abbreviations
- BMI:
-
Body mass index
- DGA:
-
Dietary Guidelines for Americans
- HC:
-
Hip circumference
- VAS:
-
Visual analog scale
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Benatar JR, Sidhu K, Stewart RAH. Effects of high and low fat dairy food on cardio-metabolic risk factors: a meta-analysis of randomized studies. PLoS One [Internet]. PLoS One. 2013;8(10):e76480. Available from: https://pubmed.ncbi.nlm.nih.gov/24146877/. Accessed 22 Feb 2021.
USDA and HHS. 2020-2025 Dietary Guidelines for Americans [Internet]. 2020. Available from: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf. Accessed 22 Dec 2020.
Louie JCY, Flood VM, Hector DJ, Rangan AM, Gill TP. Dairy consumption and overweight and obesity: a systematic review of prospective cohort studies. Obes Rev [Internet]. 2011;12:e582–92. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21521450. Accessed 7 Nov 2020.
Eales J, Lenoir-Wijnkoop I, King S, Wood H, Kok FJ, Shamir R, et al. Is consuming yoghurt associated with weight management outcomes? Results from a systematic review [Internet]. Int. J. Obes. Nature Publishing Group; 2016;40(5):731–46. Available from: https://pubmed.ncbi.nlm.nih.gov/26443336/. Accessed 16 Apr 2021.
USDA and HHS. Dietary Guidelines for Americans 2005 [Internet]. 2005. Available from: http://health.gov/dietaryguidelines/dga2005/document/. Accessed 6 Jan 2021.
USDA and HHS. Dietary Guidelines for Americans, 2010 [Internet]. 7th ed. Washington, DC: U.S. Government Printing Office; 2010. Available from: DietaryGuidelines.gov
USDA, HHS. 2015-2020 Dietary Guidelines - health.gov [Internet]. 2016. Available from: http://health.gov/dietaryguidelines/2015/guidelines/. Accessed 8 Jan 2021.
Crichton GE, Howe, PRC, Buckley JD, Coates AM, and Murphy KJ. Dairy consumption and cardiometabolic health: outcomes of a 12-month crossover trial. Nutr Metab [Internet]. BioMed Central Ltd; 2012;9:1–11. https://doi.org/10.1186/1743-7075-9-19
Rideout TC, Marinangeli CPF, Martin H, Browne RW, Rempel CB. Consumption of low-fat dairy foods for 6 months improves insulin resistance without adversely affecting lipids or bodyweight in healthy adults: a randomized free-living cross-over study. Nutr J [Internet]. 2013;12:56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23638799. The randomized crossover trial from Rideout et al. found no significant differences in body weight and body fat outcomes after overweight adults and adults with obesity followed high-dairy and low-dairy diets for 6 months. Accessed 3 Nov 2020.
Rietsema S, Eelderink C, Joustra ML, Van Vliet IMY, Van Londen M, Corpeleijn E, et al. Effect of high compared with low dairy intake on blood pressure in overweight middle-aged adults: results of a randomized crossover intervention study. Am J Clin Nutr [Internet]. Oxford University Press; 2019;110(2):340–48. Available from: https://pubmed.ncbi.nlm.nih.gov/31237322/. Accessed 21 Aug 2020.
Eelderink C, Rietsema S, Van Vliet IMY, Loef LC, Boer T, Koehorst M, et al. The effect of high compared with low dairy consumption on glucose metabolism, insulin sensitivity, and metabolic flexibility in overweight adults: a randomized crossover trial. Am J Clin Nutr [Internet]. Oxford University Press; 2019;109(6):1555–68. Available from: https://pubmed.ncbi.nlm.nih.gov/30997492/. Accessed 20 Oct 2020.
Ilich JZ, Kelly OJ, Liu PY, Shin H, Kim Y, Chi Y, et al. Role of calcium and low-fat dairy foods in weight-loss outcomes revisited: results from the randomized trial of effects on bone and body composition in overweight/obese postmenopausal women. Nutrients MDPI AG. 2019;11(5):1157 Ilich et al. conducted a randomized control trial during which participants consumed a high-dairy diet, low-dairy diet with calcium and vitamin D supplements, or placebo pills. Both the high-dairy and supplement group lost more body fat, though the high-dairy group also had greater decreases in WC, HC, and abdominal circumference.
Maersk M, Belza A, Stødkilde-Jørgensen H, Ringgaard S, Chabanova E, Thomsen H, et al. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: a 6-mo randomized intervention study. Am J Clin Nutr [Internet]. Am J Clin Nutr. 2012;95(2):283–9. Available from: https://pubmed.ncbi.nlm.nih.gov/22205311/
Celik N, Inanc N. Effects of dairy products consumption on weight loss and blood chemistry in premenopausal obese women. J Pak Med Assoc. 2016;66(1):76–82.
Bendtsen LQ, Blædel T, Holm JB, Lorenzen JK, Mark AB, Kiilerich P, et al. High intake of dairy during energy restriction does not affect energy balance or the intestinal microflora compared with low dairy intake in overweight individuals in a randomized controlled trial. Appl Physiol Nutr Metab [Internet]. Canadian Science Publishing; 2018;43(1):1–10. Available from: https://pubmed.ncbi.nlm.nih.gov/28829923/. Accessed 20 Oct 2020. Adults with obesity who participated in the randomized controlled study by Bendtsen et al. followed a hypocaloric diet either high or low in dairy for 24 weeks and there was only one significant difference in adiposity-related outcomes (higher decrease in HC among the low-dairy group).
Maltais ML, Perreault K, Courchesne-Loyer A, Lagacé JC, Barsalani R, Dionne IJ. Effect of resistance training and various sources of protein supplementation on body fat mass and metabolic profile in sarcopenic overweight older adult men: a pilot study. Int J Sport Nutr Exerc Metab [Internet]. Human Kinetics Publishers Inc.; 2016;26(1):71–7. Available from: https://pubmed.ncbi.nlm.nih.gov/26894503/. Accessed 10 Apr 2021.
Josse AR, Atkinson SA, Tarnopolsky MA, Phillips SM. Increased consumption of dairy foods and protein during diet- and exercise-induced weight loss promotes fat mass loss and lean mass gain in overweight and obese premenopausal women. J Nutr [Internet]. J Nutr; 2011;141(9):1626–34. Available from: https://pubmed.ncbi.nlm.nih.gov/21775530/. Accessed 10 Apr 2021.
Palacios C, Bertrán JJ, Ríos RE, Soltero S. No effects of low and high consumption of dairy products and calcium supplements on body composition and serum lipids in Puerto Rican obese adults. Nutrition [Internet]. Nutrition; 2011;27(5):520–5. Available from: https://pubmed.ncbi.nlm.nih.gov/20579848/. Accessed 10 Apr 2021.
Faghih SH, Abadi AR, Hedayati M, Kimiagar SM. Comparison of the effects of cows’ milk, fortified soy milk, and calcium supplement on weight and fat loss in premenopausal overweight and obese women. Nutr Metab Cardiovasc Dis. 2011;21:499–503.
Witbracht MG, Van Loan M, Adams SH, Keim NL, Laugero KD. Dairy food consumption and meal-induced cortisol response interacted to influence weight loss in overweight women undergoing a 12-week, meal-controlled, weight loss intervention. J Nutr [Internet]. American Society for Nutrition; 2013;143(1):46–52. Available from: /pmc/articles/PMC3735906/. Accessed 10 Apr 2021.
Champagne CM, Broyles ST, Moran LD, Cash KC, Levy EJ, Lin PH, et al. Dietary intakes associated with successful weight loss and maintenance during the weight loss maintenance trial. J Am Diet Assoc [Internet]. J Am Diet Assoc; 2011;111(12):1826–35. Available from: https://pubmed.ncbi.nlm.nih.gov/22117658/. Accessed 10 Apr 2021.
Radavelli-Bagatini S, Zhu K, Lewis JR, Prince RL. Dairy food intake, peripheral bone structure, and muscle mass in elderly ambulatory women. J Bone Miner Res [Internet]. 2014;29(7):1691–700. Available from: http://doi.wiley.com/10.1002/jbmr.2181. Accessed 7 Nov 2020.
Dougkas A, Minihane AM, Givens DI, Reynolds CK, Yaqoob P. Differential effects of dairy snacks on appetite, but not overall energy intake. Br J Nutr [Internet]. Br J Nutr; 2012;108(12):2274–85. Available from: https://pubmed.ncbi.nlm.nih.gov/22380537/. Accessed 10 Apr 2021.
Law M, Huot PSP, Lee YT, Vien S, Luhovyy BL, Anderson GH. The effect of dairy and nondairy beverages consumed with high glycemic cereal on subjective appetite, food intake, and postprandial glycemia in young adults. Appl Physiol Nutr Metab [Internet]. Canadian Science Publishing; 2017;42(11):1201–9. Available from: http://www.nrcresearchpress.com/doi/10.1139/apnm-2017-0135. Accessed 10 Apr 2021.
Maersk M, Belza A, Holst JJ, Fenger-Grøn M, Pedersen SB, Astrup A, et al. Satiety scores and satiety hormone response after sucrose-sweetened soft drink compared with isocaloric semi-skimmed milk and with non-caloric soft drink: a controlled trial. Eur J Clin Nutr [Internet]. Eur J Clin Nutr; 2012;66(4):523–9. Available from: https://pubmed.ncbi.nlm.nih.gov/22252107/. Accessed 10 Apr 2021.
Ortinau LC, Hoertel HA, Douglas SM, Leidy HJ. Effects of high-protein vs. high- fat snacks on appetite control, satiety, and eating initiation in healthy women. Nutr J [Internet]. BioMed Central; 2014;13:97. Available from: http://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-13-97. Accessed 6 Dec 2020
El Khoury D, Brown P, Smith G, Berengut S, Panahi S, Kubant R, et al. Increasing the protein to carbohydrate ratio in yogurts consumed as a snack reduces post-consumption glycemia independent of insulin. Clin Nutr [Internet]. Clin Nutr; 2014;33(1):29–38. Available from: https://pubmed.ncbi.nlm.nih.gov/23591152/. Accessed 10 Apr 2021.
Clark MJ, Slavin JL. The effect of fiber on satiety and food intake: a systematic review. J Am Coll Nutr [Internet]. Taylor & Francis Group; 2013;32(3):200–11. Available from: http://www.tandfonline.com/doi/abs/10.1080/07315724.2013.791194?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3Dpubmed#.VdSx4_lVhHw. Accessed 3 Nov 2020.
Rossner S. Food, diet and obesity. Edited by David J. Mela. Woodhead Publishing in Food Science and Technology, Cambridge, 2005/CRC, Washington DC. Obes Rev [Internet]. 2006;7(3):299–299. Available from: http://doi.wiley.com/10.1111/j.1467-789X.2006.00254.x. Accessed 3 Nov 2020.
Benelam B. Satiation, satiety and their effects on eating behaviour. Nutr Bull [Internet]. John Wiley & Sons, Ltd; 2009;34(2):126–73. Available from: http://doi.wiley.com/10.1111/j.1467-3010.2009.01753.x. Accessed 15 Apr 2021.
Mattes R. Soup and satiety. Physiol Behav. 2005;83:739–47.
Di Meglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes [Internet]. Nature Publishing Group; 2000;24(6):794–800. Available from: www.nature.com/ijo. Accessed 15 Apr 2021.
Zemel MB, Teegarden D, Van Loan M, Schoeller DA, Matkovic V, Lyle RM, et al. Dairy-rich diets augment fat loss on an energy-restricted diet: a multicenter trial. Nutrients [Internet]. MDPI AG; 2009;1(1):83–100. Available from: /pmc/articles/PMC3257590/. Accessed 15 Apr 2021.
Zemel MB, Thompson W, Milstead A, Morris K, Campbell P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes Res [Internet]. North American Assoc. for the Study of Obesity; 2004;12(3):582–90. Available from: http://doi.wiley.com/10.1038/oby.2004.67. Accessed 15 Apr 2021.
Zemel MB, Richards J, Mathis S, Milstead A, Gebhardt L, Silva E. Dairy augmentation of total and central fat loss in obese subjects. Int J Obes [Internet]. Nature Publishing Group; 2005;29(4):391–7. Available from: www.nature.com/ijo. Accessed 15 Apr 2021.
Acknowledgement
JMH was employed by National Dairy Council when this article was being written.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
At the time this article was written, JMH was an employee of National Dairy Council.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Obesity and Diet
Rights and permissions
About this article
Cite this article
Hess, J.M. The Impact of Dairy Intake on Adiposity and Satiety in Adults. Curr Cardiovasc Risk Rep 15, 14 (2021). https://doi.org/10.1007/s12170-021-00676-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s12170-021-00676-6