Abstract
Precise risk stratification of atherosclerotic cardiovascular disease guides best management and therefore is a public health priority. In addition to risk estimation using traditional risk factors, tools such as coronary artery calcium, high-sensitivity C-reactive protein, ankle-brachial index and carotid imaging, and clinical features such as family history of premature coronary heart disease may offer opportunities for a more personalized risk assessment. In this review, we discuss the strengths and limitations of each of these tools, focusing on the evidence provided by the latest studies relevant to the field. Among them, coronary artery calcium currently stands out as the most powerful tool for cardiovascular risk assessment, as recognized by the 2013 ACC/AHA Risk Assessment Guideline. Recent studies have expanded our knowledge regarding its value for improving the detection of both low and high absolute risk within clinically relevant subgroups, as well as for cost-effectively guiding preventive therapy allocation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction—Current Challenges in Cardiovascular Risk Assessment
Cardiovascular disease (CVD) remains a leading cause of death throughout the world. A large fraction is atherosclerotic CVD (ASCVD), including myocardial infarction and stroke. Even in those countries in which the combination of primordial preventive interventions, improved risk factor management, and modern acute-phase pharmacologic and invasive therapies have resulted in a marked reduction in cardiovascular mortality, ASCVD still represents a major cause of morbidity, disability, hospital discharges, and healthcare costs [1, 2, 3•]. Furthermore, the growing prevalence of risk factors such as obesity and diabetes—with striking increases in their prevalence among young adults and the youth [1]—threatens to worsen this situation in the next few decades. These phenomena highlight the need for effective preventive interventions, among which the early, accurate detection of asymptomatic individuals at an increased cardiovascular risk is crucial.
On the other hand, increased life expectancy and population aging in Western countries have increased the size of the elderly population, a group often affected by multiple chronic diseases and treated with several pharmacotherapies at the same time. This context underscores the need for tools that accurately discriminate individuals who are likely to have ASCVD events and, thus, more likely to benefit from preventive pharmacotherapies, from those in whom costly treatments with potential drug-drug interactions and side effects could be downscaled or minimized.
Thus, the accurate detection of both high and low cardiovascular risk appears more important than ever and carries important clinical and public health implications. In this review, we address the strengths and limitations of currently available cardiovascular risk assessment tools, discussing the findings from the most recent, highest quality literature relevant to the field.
Traditional Cardiovascular Risk Factors and Risk Scores
The causal role of high blood pressure, dyslipidemia, diabetes, and tobacco use in the development and progression of atherosclerosis is undisputed [4, 5]. However, their performance as predictors of an individual’s risk is modest. On the one hand, neither lifetime exposure nor individual/genetic susceptibility—which are believed to play a key role in the eventual development of disease [6•]—are captured by scores combining one-time measurements of a limited set of those factors. On the other hand, risk scores provide predictions based on group averages (with confidence intervals around the predictions) and may be helpful guiding preventive strategies at the population level. However, even though an individual patient may be classified in a group that is expected to derive net benefit from a preventive therapy, that does not mean that a specific patient will definitely benefit from it [7•].
Furthermore, as a consequence of the heavy weight of chronological age in risk scores, young adults with significant risk factors tend to be misclassified in lower risk categories [8–10]. This may result in the late treatment of those subjects likely to get the greatest benefit from timely interventions. In contrast, elderly adults are systematically classified into high-risk categories regardless of their risk factor profile [11, 12, 13•], leading to an expanded indication for preventive pharmacotherapies in that group. However, concentrating preventive therapies in the second half of life would seem to be a reactive approach that is somewhat in conflict with the underlying principles of preventive healthcare.
Thus, even though traditional risk factors and risk assessment scores may provide a first approximation to an individual’s absolute risk in clinical practice, there may be a wide range of scenarios in which they will fall short, providing an opportunity for other risk assessment tools for moving the risk needle to a more reliable, accurate evaluation.
The 2013 Risk Assessment Guidelines
The American College of Cardiology and the American Heart Association (ACC/AHA) released in November 2013 a new set of joint cardiovascular prevention guidelines, with recommendations for both ASCVD risk assessment [14••] and management [15••, 16, 17] in asymptomatic adults. These new guidelines addressed important limitations from previous versions, particularly by developing specific risk prediction equations for women and African-Americans. Stroke was included as part of an aggregated cardiovascular events outcome, and a lifetime risk estimator was provided for those aged 20–59 years.
Yet, this new version of the guidelines still relied on the traditional approach that started with the Framingham Risk Score to cardiovascular risk assessment—the use of a limited set of single-time measurements of traditional cardiovascular risk factors, combined in a 10-year risk score. Age, sex, levels of total and HDL cholesterol, systolic blood pressure, hypertension treatment use (yes/no), diabetes (yes/no), and smoking status (yes/no), which are indeed the same factors considered in previous versions of the guidelines, were combined in race/ethnicity specific equations as an ASCVD risk estimator. It was intended to be used in adults 20–79 years of age by the Risk Assessment Guideline (age 40–75 by the Cholesterol Guideline) without clinical ASCVD, LDL cholesterol ≥190 mg/dL, or diabetes plus LDL cholesterol ≥70 mg/dL (subgroups already considered to be at high risk) [14••]. Treatment algorithms were built on the results of the estimator by the Cholesterol Guideline Panel, which recommended a clinician-patient risk discussion including consideration of statin treatment for those subjects with a 10-year ASCVD risk ≥7.5 % (Class I, Level of Evidence A) [15••].
Beyond the inherent limitations of the traditional risk factors approach, immediately following the release of the guidelines, it was noted that application of the risk estimator in modern cohorts resulted in an overestimation of risk up to 150 % [18•]. This phenomenon was consistent with some overestimation already detected in the external validation studies [19] and could not be fully explained by increased statin use or coronary revascularizations in modern cohorts nor by differences in event ascertainment [20•]. Thus, the causes remain unclear, although it has been suggested that discrepancies between modern cohorts and the ones used for developing the 2013 Pooled Cohort Equations may be in part attributed to temporal trends of cardiovascular risk factors and disease. The inclusion of stroke in the outcome, resulting in an increased sensitivity of the new risk calculator to chronologic age, may also play a role [21•]. Finally, another reasonable hypothesis is that traditional risk factors alone cannot account for the lower risk of those in a higher socioeconomic class.
Importantly, using the new risk estimator and following the related risk management algorithms overall reduces the threshold for initiating a clinician-patient risk discussion to consider statin treatment. It appears that a clinician-patient risk discussion is now indicated in almost every white man 65 years of age or older and in almost every African-American male age 55 and older [22]. This is a good step forward as too few patients are aware of their risk status and the potential options for managing it. However, treatment decisions must be individualized, and clinicians need to grow more comfortable using other risk assessment tools to help refine the score-based risk estimate. Specifically, while other tools are commonly thought of as useful for upgrading risk classification, downgrading score-based risk predictions is particularly important to consider in elderly groups that are classified as high risk entirely or predominantly on the basis of chronologic rather than biologic age.
These issues can be discussed between the patient and clinician, who together can use the model of shared decision-making to personalize treatment decisions. They can consider current best evidence, the clinician can offer clinical judgment, and the patient can state his or her preferences. Highlighting the clinician-patient risk discussion in the 2013 ACC/AHA is a key virtue of the guidelines [23, 24•], and we anticipate that more specific guidance to clinicians will be forthcoming.
The discussion is indeed an opportunity to address uncertainty in risk estimation and consider the use of other tools to refine the risk estimate, potentially allowing for more personalized management [25•]. Although an “intermediate risk” group is no longer specified in the guideline, we have proposed 5 to 15 % 10-year predicted risk to roughly define such a group [24•, 25•], but the performance of such an approach has not been formally tested. Ultimately, the goal is to match intensity of preventive interventions with absolute risk [26].
Family History of Premature Coronary Heart Disease
Given genetically based clustering of disease, family history is part of routine medical assessment, though greater attention to ascertaining it may be needed in some practices [27]. A family history of premature ASCVD may be considered present if ASCVD manifested in a first-degree male relative before <55 years of age or a first-degree female relative <65 years [14••, 28]. Such individuals are candidates for Lp(a) testing and management [29], which may be one avenue to address the need for greater mitigation of risk [30].
Observational studies of family history, albeit somewhat heterogeneous in definitions, have repeatedly shown an independent association with subclinical atherosclerosis [31–35]. For example, in the Multi-Ethnic Study of Atherosclerosis (MESA), a family history of coronary disease was independently associated with the presence and extent of coronary artery calcium (CAC) [32]. In addition, the Coronary Artery Risk Development in Young Adults (CARDIA) investigators observed an independent association of parental history of premature CVD with CAC and carotid intima-media thickness (CIMT), though it was limited to white participants [33].
In MESA, incidence and progression of CAC were most strongly related to family history in white individuals, though formal interaction testing by ethnicity was non-significant [34]. Considering risk of ASCVD events, another recent MESA analysis assessed risk associated with a positive family history in individuals with a baseline CAC score of 0 (CAC = 0) [35]. Although the absolute event rate was low in these individuals, there was approximately a 70 % proportional increase in CVD events in those with a family history of coronary disease.
Overall, family history may provide a rough approximation of an individual’s genetic susceptibility. Patients will vary in their ability to accurately report family history. The 2013 ACC/AHA guidelines recommend family history assessment “in subjects in whom treatment decisions are uncertain after quantitative risk assessment” [14••]. We also advise that clinicians consider assessing family history regularly—particularly in young adults—as a cheap way to contextualize the risk assessment approach.
Coronary Artery Calcium
Provided the limitations of traditional risk factors as predictors of risk, in the last two decades several tests including coronary atherosclerosis-imaging techniques, serum biomarkers and other diagnostic and prognostic tests have been developed, aimed to provide a more personalized, accurate cardiovascular risk assessment, and enhance subsequent decision-making.
Among them, since the publication in 1990 of Agatston’s method for measuring the CAC score [36], a wealth of studies have shown CAC being the most powerful single tool for cardiovascular risk assessment. CAC is a reliable marker of total atherosclerotic plaque burden [37–39], is independently associated with CVD events and mortality in asymptomatic subjects, and improves risk predictions beyond traditional risk factors [40, 41, 42••, 43••, 44••, 45••]. Of note, high-quality studies have shown such improvement to be greater than that attained by any other currently available advanced risk assessment tool [42••, 43••, 44••] (Table 1).
Accordingly, the 2013 ACC/AHA guidelines consider CAC “likely to be the most useful of the current approaches to improving risk assessment among individuals found to be at intermediate risk after formal risk assessment” [14••, 46•]. Moreover, beyond the further risk assessment of subjects considered at intermediate risk (which, as noted above, is unclearly defined in the new guidelines though we have provided potential ranges to consider), CAC may be helpful in other relevant risk assessment scenarios as well (Table 2).
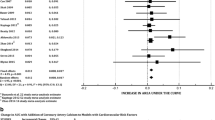
In the last year, several studies further expanded knowledge on the potential utility of CAC in clinical practice. In MESA, CAC improved CVD risk predictions among subjects at the extremes of traditional risk factor burden [47•], as well as among categories of number of lipid abnormalities, levels of LDL and non-HDL cholesterol, and quartiles of total/HDL cholesterol [48•] (Fig. 1.). Of note, in MESA, the threshold of a CAC score ≥100 was associated with CVD event rates similar to those of secondary prevention populations [48•]. Thus, the binary distinction between primary and secondary prevention becomes blurred from an absolute risk and management standpoint.
Atherosclerotic cardiovascular disease event rates per 1000 person-years by number of lipid abnormalities (upper left), LDL cholesterol levels (upper right), quartiles of total/HDL cholesterol (lower left) and non-HDL cholesterol levels (lower right), and coronary artery calcium score. Abbreviations: CVD cardiovascular disease, LA lipid abnormalities, CAC coronary artery calcium, LDL-C low-density lipoprotein cholesterol, TC total cholesterol, HDL-C high-density lipoprotein cholesterol. Reproduced with permission from Martin SS et al.: dyslipidemia, coronary artery calcium, and incident atherosclerotic cardiovascular disease: implications for statin therapy from the multi-ethnic study of atherosclerosis. Circulation. 2014 Jan 7;129(1):77-86
Moreover, in MESA, CAC improved the prediction of incident cerebrovascular events beyond clinical features [49], highlighting its potential value as a tool for guiding stroke prevention efforts. This makes sense given the shared underlying pathophysiology. Furthermore, CAC has been found to be a cost-effective strategy for guiding statin therapy [50•], as well as a potentially helpful tool for guiding aspirin allocation [51] and the use of the polypill [52]. In a context of cost-constrained healthcare systems, these findings are likely to have important public health and economic implications.
Beyond its performance identifying asymptomatic subjects at an increased risk, CAC may be particularly valuable as a “negative” test to downgrade risk or “de-risk” an individual. A CAC = 0 is associated with an excellent 10-year prognosis [53] and may aid the detection of true low risk among subjects stratified as intermediate or high risk by clinical scores, leading to a more selective use of preventive pharmacotherapies. Importantly, recent research has expanded our understanding regarding the stability or “warranty period” of a CAC = 0 over time, assessing the potential role of combining information derived from different imaging techniques and measurements for predicting calcium conversion (the development of detectable coronary calcium in a subject with CAC = 0 in a first scan) [54]. In the future, the interplay between clinical features and the information derived from imaging techniques will likely allow building personalized, safe, and cost-effective follow-up strategies for subjects with CAC = 0 on a first scan [55].
Finally, the performance of new CAC scoring modalities for risk assessment has also been tested recently. The regional distribution of CAC among the coronary arteries has been found to be strongly and independently associated with frequency and mode of future coronary revascularization [56•]. Coronary calcium density has shown an inverse, independent association with CVD at any level of CAC volume [57•]. In the next years, the combination of improved CAC scoring methods such as CAC density with the information provided by regional patterns will likely further improve risk assessment beyond the standard CAC score.
CAC also has limitations that must be considered. No randomized, adequately powered trial has assessed the use of CAC for guiding preventive interventions and their impact on cardiovascular outcomes. Moreover, because of technical and funding reasons, such trial is unlikely to be performed in the near future [58]. However, this limitation also applies to the guideline-supported strategy of statin allocation guided by risk scores, as well as to any other advanced risk assessment tool. In such context, the results from carefully designed observational studies have provided consistent evidence regarding the superiority of CAC compared to any other risk assessment approach [42••, 43••, 44••, 45••].
Second, computed tomographic (CT) scanning for CAC scoring involves radiation exposure, even though with modern scans, the associated radiation dose is ≤1.0 mSv. This amount of radiation is roughly equivalent to two transatlantic flights or a bilateral mammogram. When considering the importance of radiation, one should also take into account the age of the patient. It is generally felt that the importance of radiation exposure may be greater in a younger patient.
Third, CAC may fail to detect early non-calcified atherosclerotic plaque. Nevertheless, recent evidence has shown that asymptomatic subjects with CAC = 0 have a very low presence of non-calcified atherosclerotic plaque, including only a 1 % of subjects with obstructive, non-calcified plaque, and a very low event rate after a median follow-up of 22 months [59]. Fourth, there needs to be greater consideration of whether examination of the lung window during a CAC scan is truly justified, and, if so, whether routine follow-up CT scans add clinical value.
Finally, a recent propensity-score matched study suggested that the use of CAC for risk assessment may be associated with increased downstream testing and healthcare costs compared to other risk assessment tools [60•]. Nonetheless, in the same study, CAC-guided management was associated with lower CVD event rates. Furthermore, it is unknown whether that increased testing and cost offsets the potential savings of a more accurate risk assessment attained with CAC.
High-Sensitivity C-Reactive Protein
Inflammation is believed to have a critical role in the development and stability of coronary atherosclerotic plaque [61]. Accordingly, in the last two decades, a number of serum biomarkers have been tested for their association with CVD events, as well as for their potential value for improving risk predictions beyond traditional risk factors. Among them, high-sensitivity C-reactive protein (hsCRP), which was first linked with coronary artery disease risk in 1996 [62], has gained the greatest attention.
Studies have shown hsCRP being independently associated with CVD events and mortality [63, 64]. The 2013 risk assessment guidelines recommend considering hsCRP testing selectively for further risk assessment when clinical management is uncertain. However, widespread use of hsCRP in clinical practice either as a tool for risk assessment or for the allocation of statin therapy—as suggested by the JUPITER trial [65]—is currently not justified [66•]. In intermediate-risk subjects in MESA, the majority of events actually occurred in subjects with hsCRP <2 mg/L, whereas approximately 90 % occurred in individuals with CAC > 0 [67]. Finally, a recent study reported that 440 intermediate-risk individuals would have to be screened using hsCRP levels—and treated with statins accordingly—in order to prevent one additional CVD event over the course of 10 years [68].
Hence, currently available evidence suggests that the performance of hsCRP as a tool for risk assessment or preventive therapy allocation is modest. Indeed, hsCRP has a marked ethnic, sex-related, and intra-individual short-term variability [66•, 69], and its ability for capturing long-term exposure is limited. Moreover, whereas other tests such as CAC improve risk predictions among hsCRP categories [67], the value of hsCRP for improving risk predictions beyond the information provided by those tools is unknown.
Ankle-Brachial Index
Endothelial dysfunction and atherosclerosis are systemic processes, and subjects with a diseased vascular bed are more likely to have disease in other locations as well [70]. Accordingly, a number of tests aimed at detecting atherosclerosis in territories other than the coronary arteries have been proposed as tools for improving coronary and cerebrovascular risk assessment in clinical practice. Among them, the ankle-brachial index (ABI) and carotid ultrasound imaging have generated the greatest research interest.
Beyond its role as a surrogate marker for peripheral arterial disease (PAD) [71], the ABI is robustly and independently associated with incident CVD events [72] including recurrent stroke [73]. The 2013 ACC/AHA guidelines support the use of ABI for further cardiovascular risk assessment in subjects for whom risk-based decision-making is uncertain after risk estimation using traditional risk factors, specifically by “revising risk assessment upward” in subjects with an ABI <0.9 [14••]. Such a cut point has a high specificity, but its sensitivity for detecting increased CVD risk is low [74], with only 5 % of the US population ≥40 years of age without known CVD having an ABI ≤0.9 [75].
Moreover, a recent systematic review on the added value of ABI in risk prediction noted that, currently, there is insufficient evidence to assess the balance of harms and benefits of CVD risk assessment using the ABI [76•, 77]. The same review also found limited trial evidence regarding treatment of CVD in persons with asymptomatic or minimally symptomatic PAD [76•, 77]. Specifically, the value of the ABI in risk reclassification is considered almost non-existent in adults <65 years of age. Finally, a recent study detected important technical issues associated with the measurement of ABI in clinical practice [78].
Thus, even though the ABI may be an informative test in the elderly and in subgroups of subjects with high CVD event rates [76•, 77], its widespread use as a tool for further risk assessment is likely to provide limited information in most patients.
Carotid Ultrasound Imaging
CIMT and the presence of carotid plaque can be assessed non-invasively using ultrasound imaging. Regarding CIMT, baseline [79] and some progression measurements [80] have each shown an independent association with incident CVD events. Furthermore, CIMT in MESA was a better predictor of incident stroke than CAC [81]. However, the 2013 AHA/ACC guidelines recommend against the routine measurement of CIMT for CVD risk assessment in clinical practice (class of recommendation III, level of evidence B) based on concerns regarding measurement quality and standardization, as well as on the evidence provided by recent studies [82] and a meta-analysis [83•] of 14 population-based cohorts (N = 45,828) showing a very modest performance of CIMT to improve risk predictions beyond traditional risk factors [14••]. More recent studies published after the release of the guidelines have reported similar findings [84•].
On the other hand, the prognostic value of CIMT increases when combined with measurements of carotid plaque [85, 86], a strategy not addressed in the 2013 ACC/AHA guidelines [14••] but which has been suggested as a reasonable screening strategy by expert consensus documents [87]. Interestingly, the combination of CIMT and carotid plaque measurements may be particularly useful for downgrading risk estimates in subjects unlikely to have events [88]. Finally, a recent MESA study on carotid plaque measurements using magnetic resonance imaging (MRI), which provides insight into carotid plaque morphology, composition, and remodeling, reported improved risk predictions when carotid plaque measurements were added to traditional risk factors [84•]. Future studies will expand our understanding regarding the potential role of combined measurements of CIMT and plaque and of carotid MRI, as well as their performance and cost-effectiveness compared to other tests.
Other Potential Risk Assessment Tools
Coronary computed tomography angiography, which allows for the detection of non-calcified atheroma, and the detailed study of coronary plaque using MRI, offer opportunities for advanced imaging in selected individuals and specific clinical scenarios, but currently are not recommended as tools for routine risk assessment in asymptomatic subjects [14••, 89–91]. Similarly, stress testing is not routinely recommended for risk stratification in asymptomatic adults [14••, 89, 90].
Measurements of arterial reactivity (such as brachial flow-mediated dilation) and stiffness (such as pulse wave velocity) are independently associated with CVD events [92, 93]; however, their clinical role remains unclear. A number of serum biomarkers beyond hsCRP have also been considered as potential risk assessment tools, either individually or combined in “multiple biomarker” panels; however, their performance seems to be modest [42••, 43••, 44••].
In addition to the standard lipid profile, multiple other lipid tests are available, such as apolipoprotein B and LDL particle concentration. Recent studies have demonstrated the importance of lipid discordance, an under-detected but common phenomenon that may lead to risk misclassification [94, 95•, 96]. Additional discordance analyses are warranted, and future guidelines may clarify the groups of patients that may benefit from additional lipid testing at baseline and on-treatment.
Chronic kidney disease (CKD) is strongly associated with incident CVD in the general population [97] and has been proposed as a coronary heart disease risk equivalent [98]. Furthermore, preventive treatments reduce CVD events in this group [99]. Thus, some scientific societies consider CKD patients at high CVD risk and advocate for the aggressive management of their risk factors [28, 90].
Cardiorespiratory fitness is considered an integrative predictor of all-cause mortality and may offer complementary information to that provided by atherosclerosis-imaging techniques such as CAC [100•]. However, the role of fitness measurements in the prediction of cardiovascular events is currently unclear, and further research is needed.
Finally, despite the identification of genetic variants that predispose to the development of CVD, whether the results of genotype testing alter management or improve clinical outcomes is currently unknown, and current guidelines do not recommend genetic testing as part of a cardiovascular risk assessment strategy [14••, 89, 90].
Conclusion
CAC, the flagship of a personalized atherosclerosis-imaging, disease-detection paradigm, is the best single tool for cardiovascular risk assessment. CAC refines risk predictions within clinically relevant subgroups and among a wide range of risk assessment scenarios, and offers opportunities for a more cost-effective allocation of preventive pharmacotherapies. On the other hand, recent evidence has shown that the improvement in risk prediction with hsCRP and ABI is likely to be modest.
Future iterations of the risk assessment guidelines should incorporate the findings from the latest, highest quality studies regarding the role that advanced risk assessment tools can play in clinical practice. Thus, beyond traditional risk scores and easy-to-follow recommendations, by providing decision-makers with clear guidance regarding the use of such personalized risk assessment tools, the accurate stratification and management of absolute cardiovascular risk in clinical practice will be closer to becoming a reality.
Abbreviations
- ABI:
-
Ankle-brachial index
- ACC/AHA:
-
American College of Cardiology/American Heart Association
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CAC:
-
Coronary artery calcium
- CAC = 0:
-
Coronary artery calcium score of zero
- CIMT:
-
Carotid intima-media thickness
- CKD:
-
Chronic kidney disease
- CT:
-
Computed tomography
- CVD:
-
Cardiovascular disease
- hsCRP:
-
High-sensitivity C-reactive protein
- MRI:
-
Magnetic resonance imaging
- PAD:
-
Peripheral arterial disease
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–292.
World Health Organization. Global Health Observatory. World Health Statistics 2014. Available at http://www.who.int/gho/publications/world_health_statistics/en/ Accessed January 6, 2015.
Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64(4):337–45. This study showed that acute myocardial infarction hospitalization rates in young adults have not declined over the past decade in the US.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368(21):2004–13.
Erbel R, Budoff M. Improvement of cardiovascular risk prediction using coronary imaging: subclinical atherosclerosis: the memory of lifetime risk factor exposure. Eur Heart J. 2012;33(10):1201–133. This review addressed the role of subclinical atherosclerosis as the vascular memory of lifetime exposure to risk factors, and of CAC, an atherosclerosis-imaging technique, as a tool for a more accurate risk prediction.
McEvoy JW, Diamond GA, Detrano RC, Kaul S, Blaha MJ, Blumenthal RS, et al. Risk and the physics of clinical prediction. Am J Cardiol. 2014;113(8):1429–35. This review addressed the inherent limitations of the risk score-based approach for predicting an individual’s cardiovascular risk.
Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the national cholesterol education panel III guidelines perform? J Am Coll Cardiol. 2003;41:1475–9.
Lakoski SG, Greenland P, Wong ND, Schreiner PJ, Herrington DM, Kronmal RA, et al. Coronary artery calcium scores and risk for cardiovascular events in women classified as "low risk" based on Framingham risk score: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2007;167:2437–42.
Michos ED, Nasir K, Braunstein JB, Rumberger JA, Budoff MJ, Post WS, et al. Framingham risk equation underestimates subclinical atherosclerosis risk in asymptomatic women. Atherosclerosis. 2006;184:201–6.
Ford ES, Giles WH, Mokdad AH. The distribution of 10-year risk for coronary heart disease among US adults: findings from the national health and nutrition examination survey III. J Am Coll Cardiol. 2004;43(10):1791–6.
Ford ES, Will JC, Mercado CI, Loustalot F. Trends in predicted risk for atherosclerotic cardiovascular disease using the pooled cohort risk equations among US adults from 1999 to 2012. JAMA Intern Med. 2014. doi: 10.1001/jamainternmed.2014.6403.
Pencina MJ, Navar-Boggan AM, D’Agostino Sr RB, Williams K, Neely B, Sniderman AD, et al. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370(15):1422–31. This study used NHANES to calculate the number of US adults who would be considered eligible for statin therapy according to the 2013 ACC/AHA guidelines.
Goff Jr DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino Sr RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59. The 2013 ACC/AHA cardiovascular risk assessment guidelines.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934. The 2013 ACC/AHA treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk guidelines.
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960–84.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023.
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382(9907):1762–5. This study found that the implementation of the 2013 ACC/AHA risk assessment guidelines in modern cohorts resulted in a risk overestimation of up to 150%.
Goff DC, Lloyd-Jones DM, Bennett G, Gibbons R, Greenland P, Lackland DT, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Risk Assessment Full Work Group Report. Available at: http://circ.ahajournals.org/content/early/2013/11/11/01.cir.0000437741.48606.98/suppl/DC1
Cook NR, Ridker PM. Further insight into the cardiovascular risk calculator: the roles of statins, revascularizations, and underascertainment in the Women’s health study. JAMA Intern Med. 2014;174(12):1964–71. This study found that differences in statin use, revascularizations or underascertainment of events did not fully explain the discrepancy between observed rates of ASCVD in the WHS and those predicted by the 2013 ACC/AHA risk estimator.
Karmali KN, Goff Jr DC, Ning H, Lloyd-Jones DM. A systematic examination of the 2013 ACC/AHA pooled cohort risk assessment tool for atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2014;64(10):959–68. This study addressed potential explanations for the risk overestimation resulting from the implementation of the 2013 ACC/AHA risk estimator in modern cohorts.
Miedema MD, Lopez FL, Blaha MJ, Virani SS, Coresh J, Ballantyne CM, et al. Eligibility for statin therapy according to new cholesterol guidelines and prevalent Use of medication to lower lipid levels in an older US Cohort: the Atherosclerosis Risk in Communities Study Cohort. JAMA Intern Med. 2015;175(1):138–40.
Lloyd-Jones DM, Goff D, Stone NJ. Statins, risk assessment, and the new American prevention guidelines. Lancet. 2014;383(9917):600–2.
Martin SS, Blumenthal RS. Concepts and controversies: the 2013 American College of Cardiology/American Heart Association Risk Assessment and Cholesterol Treatment Guidelines. Ann Intern Med. 2014;160(5):356–8. This editorial comment discussed the key controversies of the 2013 ACC/AHA risk assessment guidelines, and provided recommendations regarding the key features that should be addressed in the patient-physician discussion.
Blaha MJ, Dardari ZA, Blumenthal RS, Martin SS, Nasir K, Al-Mallah MH. The new "intermediate risk" group: a comparative analysis of the new 2013 ACC/AHA risk assessment guidelines versus prior guidelines in men. Atherosclerosis. 2014;237(1):1–4. This study showed how, compared with previous versions, the 2013 ACC/AHA guidelines produce an abridged, more temporary and lower risk "intermediate risk" group, and addressed its implications regarding the use of personalized risk assessment tools.
27th Bethesda Conference. Matching the intensity of risk factor management with the hazard for coronary disease events. September 14-15, 1995. J Am Coll Cardiol. 1996;27:957–1047.
Dhiman P, Kai J, Horsfall L, Walters K, Qureshi N. Availability and quality of coronary heart disease family history in primary care medical records: implications for cardiovascular risk assessment. PLoS One. 2014;9:e81998.
Anderson TJ, Grégoire J, Hegele RA, Couture P, Mancini GB, McPherson R, et al. 2012 update of the Canadian cardiovascular society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2013;29:151–67.
Jacobson TA. Lipoprotein(a), cardiovascular disease, and contemporary management. Mayo Clin Proc. 2013;88:1294–311.
Williamson C, Jeemon P, Hastie CE, McCallum L, Muir S, Dawson J, et al. Family history of premature cardiovascular disease: blood pressure control and long-term mortality outcomes in hypertensive patients. Eur Heart J. 2014;35:563–70.
Pandey AK, Pandey S, Blaha MJ, Agatston A, Feldman T, Ozner M, et al. Family history of coronary heart disease and markers of subclinical cardiovascular disease: where do we stand? Atherosclerosis. 2013;228:285–94.
Nasir K, Budoff MJ, Wong ND, Scheuner M, Herrington D, Arnett DK, et al. Family history of premature coronary heart disease and coronary artery calcification: multi-ethnic study of atherosclerosis (MESA). Circulation. 2007;116:619–26.
Wilkins JT, Gidding S, Liu K, Ning H, Polak JF, Lloyd-Jones DM, et al. Associations between a parental history of premature cardiovascular disease and carotid intima-media thickness: the coronary artery risk development in young adults (CARDIA) study. Eur J Prev Cardiol. 2014;21:601–7.
Pandey AK, Blaha MJ, Sharma K, Rivera J, Budoff MJ, Blankstein R, et al. Family history of coronary heart disease and the incidence and progression of coronary artery calcification: multi-ethnic study of atherosclerosis (MESA). Atherosclerosis. 2014;232:369–76.
Cohen R, Budoff M, McClelland RL, Sillau S, Burke G, Blaha M, et al. Significance of a positive family history for coronary heart disease in patients with a zero coronary artery calcium score (from the multi-ethnic study of atherosclerosis). Am J Cardiol. 2014;114:1210–4.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte Jr M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32.
Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation. 1995;92(8):2157–62.
Guerci AD, Spadaro LA, Popma JJ, Goodman KJ, Brundage BH, Budoff M, et al. Relation of coronary calcium score by electron beam computed tomography to arteriographic findings in asymptomatic and symptomatic adults. Am J Cardiol. 1997;79(2):128–33.
Tinana A, Mintz GS, Weissman NJ. Volumetric intravascular ultrasound quantification of the amount of atherosclerosis and calcium in nonstenotic arterial segments. Am J Cardiol. 2002;89(6):757–60.
Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358(13):1336–45.
Greenland P. More evidence for coronary calcium as a measure of cardiovascular risk: has anything changed? JAMA. 2014;311(3):247–8.
Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308(8):788–95. This study found that combining CAC with the FRS risk factors provided a superior discrimination and risk reclassification than adding CIMT, ABI, brachial flow-mediated dilation, hsCRP or family history of coronary heart disease.
Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R, Verwoert GC, et al. Evaluation of newer risk markers for coronary heart disease risk classification: a cohort study. Ann Intern Med. 2012;156(6):438–44. This study found that among 12 novel risk assessment tools including atherosclerosis-imaging techniques, serum biomarkers and other tests, adding CAC to the FRS risk factors resulted in the greatest improvement in risk prediction.
Rana JS, Gransar H, Wong ND, Shaw L, Pencina M, Nasir K, et al. Comparative value of coronary artery calcium and multiple blood biomarkers for prognostication of cardiovascular events. Am J Cardiol. 2012;109(10):1449–53. This study found that the addition of CAC but not biomarkers (neither individually nor combined in a multiple biomarker panel) substantially improved risk reclassification for future CVD events beyond traditional risk factors.
Erbel R, Möhlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf recall study. J Am Coll Cardiol. 2010;56(17):1397–406. This study showed that in subjects considered at intermediate risk by the FRS, CAC scoring resulted in a high risk reclassification rate.
Peters SAE, den Ruijter HM, Bots ML, Moons KG. Improvements in risk stratification for the occurrence of cardiovascular disease by imaging subclinical atherosclerosis: a systematic review. Heart. 2012;98(3):177–84. This systematic review provided high-quality evidence regarding the added value of CAC as a tool for further cardiovascular risk assessment beyond traditional risk factors.
Silverman MG, Blaha MJ, Krumholz HM, Budoff MJ, Blankstein R, Sibley CT, et al. Impact of coronary artery calcium on coronary heart disease events in individuals at the extremes of traditional risk factor burden: the multi-ethnic study of atherosclerosis. Eur Heart J. 2014;35(33):2232–41. This study showed how among individuals without traditional risk factors, a high CAC score is associated with high event rates, whereas the absence of CAC even among subjects with a high traditional risk factor burden is associated with low event rates.
Martin SS, Blaha MJ, Blankstein R, Agatston A, Rivera JJ, Virani SS, et al. Dyslipidemia, coronary artery calcium, and incident atherosclerotic cardiovascular disease: implications for statin therapy from the multi-ethnic study of atherosclerosis. Circulation. 2014;129(1):77–86. This study found that among individuals without lipid abnormalities or with low levels of LDL-C, a high CAC score is associated with high CVD event rates, whereas CAC = 0 is associated with low event rates even among subjects with several lipid abnormalities or high levels of LDL-C.
Gibson AO, Blaha MJ, Arnan MK, Sacco RL, Szklo M, Herrington DM, et al. Coronary artery calcium and incident cerebrovascular events in an asymptomatic cohort: the MESA study. JACC Cardiovasc Imaging. 2014;7(11):1108–15.
Pletcher MJ, Pignone M, Earnshaw S, McDade C, Phillips KA, Auer R, et al. Using the coronary artery calcium score to guide statin therapy: a cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes. 2014;7(2):276–84. This study found CAC testing to be a cost-effective strategy for cardiovascular risk assessment and statin therapy allocation in intermediate risk patients.
Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7(3):453–60.
Bittencourt MS, Blaha MJ, Blankstein R, Budoff M, Vargas JD, Blumenthal RS, et al. Polypill therapy, subclinical atherosclerosis, and cardiovascular events-implications for the use of preventive pharmacotherapy: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2014;63(5):434–43.
Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffman U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009;2(6):675–88.
Brodov Y, Gransar H, Rozanski A, Hayes SW, Friedman JD, Thomson LE, et al. Extensive thoracic aortic calcification is an independent predictor of development of coronary artery calcium among individuals with coronary artery calcium score of zero. Atherosclerosis. 2015;238(1):4–8.
Al Rifai M, Cainzos-Achirica M, Blaha MJ. Establishing the warranty of a coronary artery calcium score of zero. Atherosclerosis. 2015;238(1):1–3.
Silverman MG, Harkness JR, Blankstein R, Budoff MJ, Agatston AS, Carr JJ, et al. Baseline subclinical atherosclerosis burden and distribution are associated with frequency and mode of future coronary revascularization: multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging. 2014;7(5):476–86. This study showed that regional distribution of CAC predicted the need for coronary revascularization independently of baseline CAC burden.
Criqui MH, Denenberg JO, Ix JH, McClelland RL, Wassel CL, Rifkin DE, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311(3):271–8. This study found CAC density to be significantly and inversely associated with CHD and CVD risk, at any level of CAC volume.
McEvoy JW, Blaha MJ. Coronary artery calcium testing: exploring the need for a randomized trial. Circ Cardiovasc Imaging. 2014;7(4):578–80.
Cho I, Suh JW, Chang HJ, Kim KI, Jeon EJ, Choi SI, et al. Prevalence and prognostic implication of non-calcified plaque in asymptomatic population with coronary artery calcium score of zero. Korean Circ J. 2013;43(3):154–60.
Shreibati JB, Baker LC, McConnell MV, Hlatky MA. Outcomes after coronary artery calcium and other cardiovascular biomarker testing among asymptomatic medicare beneficiaries. Circ Cardiovasc Imaging. 2014;7(4):655–62. This study found, among asymptomatic Medicare beneficiaries, CAC testing to be associated with increased use of cardiac tests and procedures, and with higher spending, as well as with improved clinical outcomes, compared with hs-CRP testing.
Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111:1805–12.
Kuller LH, Tracy RP, Shaten J, Meilahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study multiple risk factor intervention trial. Am J Epidemiol. 1996;144:537–47.
Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9.
Amrock SM, Weitzman M. Effect of increased leptin and C-reactive protein levels on mortality: results from the National Health and Nutrition Examination Survey. Atherosclerosis. 2014;236(1):1–6.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto Jr AM, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207.
Yousuf O, Mohanty BD, Martin SS, Joshi PH, Blaha MJ, Nasir K, et al. High-sensitivity C-reactive protein and cardiovascular disease: a resolute belief or an elusive link? J Am Coll Cardiol. 2013;62(5):397–408. This review found that currently available evidence does not support the use of hsCRP neither as a tool for routine cardiovascular risk assessment nor for the allocation of statin therapy in clinical practice.
Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378(9792):684–92.
Kaptoge S, Di Angelantonio E, Pennells L, Wood AM, White IR, Gao P, et al. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med. 2012;367(14):1310–20.
Bower JK, Lazo M, Juraschek SP, Selvin E. Within-person variability in high-sensitivity C-reactive protein. Arch Intern Med. 2012;172(19):1519–21.
Anderson TJ, Gerhard MD, Meredith IT, Charbonneau F, Delagrange D, Creager MA, et al. Systemic nature of endothelial dysfunction in atherosclerosis. Am J Cardiol. 1995;75(6):71B–4.
Xu D, Zou L, Xing Y, Hou L, Wei Y, Zhang J, et al. Diagnostic value of ankle-brachial index in peripheral arterial disease: a meta-analysis. Can J Cardiol. 2013;29(4):492–8.
Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, et al. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the strong heart study. Circulation. 2004;109(6):733–9.
Fan H, Hu X, Yu W, Cao H, Wang J, Li J, et al. Low ankle-brachial index and risk of stroke. Atherosclerosis. 2013;229(2):317–23.
Doobay AV, Anand SS. Sensitivity and specificity of the ankle-brachial index to predict future cardiovascular outcomes: a systematic review. Arterioscler, Thromb, Vasc Biol. 2005;25(7):1463–9.
Pande RL, Perlstein TS, Beckman JA, Creager MA. Secondary prevention and mortality in peripheral artery disease: National Health and Nutrition Examination Study, 1999 to 2004. Circulation. 2011;124:17–23.
Lin JS, Olson CM, Johnson ES, Whitlock EP. The ankle-brachial index for peripheral artery disease screening and cardiovascular disease prediction among asymptomatic adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;159(5):333–41. This systematic review found that currently available evidence is insufficient to assess the balance of harms and benefits of CVD risk assessment using the ABI.
Moyer VA. US Preventive Services Task Force Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:342–8.
Davies JH, Kenkre J, Williams EM. Current utility of the ankle-brachial index (ABI) in general practice: implications for its use in cardiovascular disease screening. BMC Fam Pract. 2014;15:69.
Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–67.
Baldassarre D, Veglia F, Hamsten A, Humphries SE, Rauramaa R, de Faire U, et al. Progression of carotid intima-media thickness as predictor of vascular events: results from the IMPROVE study. Arterioscler, Thromb, Vasc Biol. 2013;33(9):2273–9.
Folsom AR, Kronmal RA, Detrano RC, O’Leary DH, Bild DE, Bluemke DA, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2008;168(12):1333–9.
Polak JF, Pencina MJ, Pencina KM, O’Donnell CJ, Wolf PA, D’Agostino Sr RB. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365(3):213–21.
Den Ruijter HM, Peters SA, Anderson TJ, Britton AR, Dekker JM, Eijkemans MJ, et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. 2012;308(8):796–803. This meta-analysis found that the addition of common CIMT measurements to the FRS resulted in a modest improvement in CVD risk prediction, unlikely to have clinical relevance.
Zavodni AE, Wasserman BA, McClelland RL, Gomes AS, Folsom AR, Polak JF, et al. Carotid artery plaque morphology and composition in relation to incident cardiovascular events: the Multi-Ethnic Study of Atherosclerosis (MESA). Radiology. 2014;271(2):381–9. This study found carotid plaque morphology, composition and remodeling (assessed using MRI) to improve cardiovascular risk predictions when added to traditional risk factors.
Belcaro G, Nicolaides AN, Ramaswami G, Cesarone MR, De Sanctis M, Incandela L, et al. Carotid and femoral ultrasound morphology screening and cardiovascular events in low risk subjects: a 10-year follow-up study (the CAFES-CAVE study(1)). Atherosclerosis. 2001;156:379–87.
Irie Y, Katakami N, Kaneto H, Takahara M, Nishio M, Kasami R, et al. The utility of ultrasonic tissue characterization of carotid plaque in the prediction of cardiovascular events in diabetic patients. Atherosclerosis. 2013;230(2):399–405.
Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21(2):93–111.
Gardin JM, Bartz TM, Polak JF, O’Leary DH, Wong ND. What do carotid intima-media thickness and plaque add to the prediction of stroke and cardiovascular disease risk in older adults? The cardiovascular health study. J Am Soc Echocardiogr. 2014;27(9):998–1005.
Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56(25):e50–103.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). Eur Heart J. 2012;33(13):1635–701.
Muhlestein JB, Lappé DL, Lima JA, Rosen BD, May HT, Knight S, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA. 2014;312(21):2234–43.
Shechter M, Issachar A, Marai I, Koren-Morag N, Freinark D, Shahar Y, et al. Long-term association of brachial artery flow-mediated vasodilation and cardiovascular events in middle-aged subjects with no apparent heart disease. Int J Cardiol. 2009;134(1):52–8.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55(13):1318–27.
Sniderman AD, Islam S, Yusuf S, McQueen MJ. Discordance analysis of apolipoprotein B and non-high density lipoprotein cholesterol as markers of cardiovascular risk in the INTERHEART study. Atherosclerosis. 2012;225(2):444–9.
Mora S, Buring JE, Ridker PM. Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events. Circulation. 2014;129(5):553–61. This study found that discordance in lipid levels is a common phenomenon which may result in risk under- or overestimation.
Martin SS, Michos ED. Are we moving towards concordance on the principle that lipid discordance matters? Circulation. 2014;129(5):539–41.
Tonelli M, Muntner P, Lloyd A, Manns BJ, Klarenbach S, Pannu N, et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population-level cohort study. Lancet. 2012;380(9844):807–14.
Foster MC, Rawlings AM, Marrett E, Neff D, Grams ME, Kasiske BL, et al. Potential effects of reclassifying CKD as a coronary heart disease risk equivalent in the US population. Am J Kidney Dis. 2014;63(5):753–60.
Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377(9784):2181–92.
Blaha MJ, Feldman DI, Nasir K. Coronary artery calcium and physical fitness—the two best predictors of long-term survival. Atherosclerosis. 2014;234(1):93–4. This editorial comment addressed the potential value of cardiorespiratory fitness measurements in risk prediction beyond the information provided by CAC scoring.
Acknowledgments
MC-A was funded by a research grant from the Spanish Society of Cardiology. SSM is supported by the Pollin Cardiovascular Prevention Fellowship, Marie-Josée and Henry R Kravis endowed fellowship, and a National Institutes of Health training grant (T32HL07024). RSB is supported by the Kenneth Jay Pollin Professorship in Cardiology.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Michael Blaha served on an Advisory Board for Pfizer and Luitpold Pharmaceuticals and received grant support from the FDA, all outside of the scope of the present work. Roger Blumenthal, Miguel Cainzos-Achirica and Kieran Eissler have no relevant disclosures to report. Seth Martin is listed as a co-inventor on a pending patent filed by Johns Hopkins University for a method of low-density lipoprotein cholesterol estimation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Novel and Emerging Risk Factors
Rights and permissions
About this article
Cite this article
Cainzos-Achirica, M., Eissler, K., Blaha, M.J. et al. Tools for Cardiovascular Risk Assessment in Clinical Practice. Curr Cardiovasc Risk Rep 9, 28 (2015). https://doi.org/10.1007/s12170-015-0455-4
Published:
DOI: https://doi.org/10.1007/s12170-015-0455-4