Abstract
The global epidemic of cardiovascular diseases (CVDs) is spiraling upwards primarily due to a sharp rise in the low and middle income countries (LMICs) which are experiencing rapid health transition driven by socioeconomic, technological and lifestyle changes. LMICs currently face a double burden of communicable and non-communicable diseases, leading to competing claims of health conditions that vie for policy makers’ attention as public health priorities in a setting of limited resources, substantially high out-of-pocket expenditure and weak systems of healthcare delivery. Evidence from high income countries suggests that most CVDs are largely preventable as the major CVD risk behaviours including tobacco use, physical inactivity, unhealthy diet, harmful use of alcohol, are avoidable and modifiable. Effective and sustainable behaviour change strategies for LMICs would require low cost, affordable and scalable interventions. There is limited evidence from LMICs on effective interventions to prevent, control and manage CVDs in LMICs. The global guidelines and framework for addressing CVD calls for an urgent need to identify and assess contextually relevant and resource sensitive health care interventions augmented by policy actions. A combination of population based and high risk individual based strategies which are evidence based, cost-effective, feasible as well as scalable would reduce CVD mortality and its devastating impact in LMICs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global epidemic of cardiovascular diseases (CVDs) is spiraling upwards primarily due to a sharp rise in the low and middle income countries (LMICs) which are experiencing rapid health transition driven by socioeconomic, technological and lifestyle changes. Most LMICs have witnessed rapid socio-economic and demographic transition, leading to improved life expectancy and population ageing. Further recent urbanization, globalization and improved life expectancy increase the duration of exposure of the populations to CVD risk factors and lifestyle related risk behaviours, leading to rapid health and epidemiological transition in these countries. Amongst LMICs, there is wide variation in the stage of health transition and intra-country variations in bigger LMICs like China and India which is partly explained by urban-rural differences. Unlike developed countries, LMICs currently face a double burden of communicable and non-communicable diseases, leading to competing claims of health conditions that vie for policy makers’ attention as public health priorities as well as for clinical care, in a setting of weak systems of healthcare delivery and limited resources for strengthening them adequately to meet the needs.
Cardiovascular diseases (CVDs) including ischemic heart disease (IHD) and cerebrovascular diseases cause 17.3 million (30 %) deaths, and account for nearly half of all non-communicable disease (NCD) related mortality [1, 2, 3•]. More than 80 % of all CVD related deaths occur in LMICs [4]. The profile of CVDs varies among the LMIC countries based on their stage of epidemiological transition. Those in the earliest phase of transition have a large burden of rheumatic heart disease, as well as infectious and nutritional cardiomyopathies. Countries in the next phase witness hypertension as a major public health problem and as salt consumption rises, hemorrhagic stroke and hypertensive heart diseases add to the burden of rheumatic heart disease. Countries in advanced stages of transition experience the burden of coronary heart disease and thrombotic strokes due to increased fat intake and rising lipids [5].
The increasing tide of CVDs imposes a substantial economic burden in LMICs at both population and household levels. CVDs associated cumulative lost economic output in LMICs is projected to be US$ 3.76 trillion, over the period 2011- 2025 [6]. Most LMICs face the challenge of low public funding on non-communicable diseases which leads to catastrophic out of pocket expenditure. In 2005, private expenditure accounted for 74 % of all health expenditure in LMICs [7]. In contrast to developed countries which have around 20-25 % out-of-pocket expenditure, most LMICs have substantially higher out-of-pocket expenditure, ranging from a high of 70 % in India [8] to between 40 and 45 % for countries like Argentina, Colombia, Mexico and Thailand [9].
CVDs are linked to poverty, uneven distribution of wealth, low levels of literacy, poor housing, unplanned urbanization and wider social determinants of health. According to the World Bank, CVD mortality increases with higher Gini index (higher income inequality) in low income countries compared to high income countries (HIC) [10]. In India, 25 % of families with a member with CVD experiences catastrophic expenditure and ten percent are driven into poverty [11]. The progress in addressing CVD in LMICs is relatively slower than high income settings as the countries face the challenge of insufficient funds, inadequate health infrastructure, and lack of trained health personnel to address CVD and associated risk factors.
Dimensions of CVDs in LMICs
Around ten percent of the global burden of disease as measured by disability adjusted life years (DALYs) is attributed to CVDs [3•]. Out of 151377 million DALYs due to CVDs, 62,587 million are attributed to coronary heart disease and 46,591 million to cerebrovascular disease [2]. CVD burden in LMICs has doubled over the past two decades [3•], and the nature of the burden is very different from the high income countries. During the last decade, number of individuals with peripheral artery disease increased by 28 · 7 % in LMICs and 13 · 1 % in HICs. Out of 202 million such people globally, 69.7 % belong to LMIC (including 54.8 million in Southeast Asia and 45.9 million in the western Pacific Region) [12]. Nearly 58 % of CVD deaths in LMICs occur below 60 years of age compared with 20 % in high income settings [13]. Around 26 % of coronary heart disease deaths in Mexico and 35 % of CVD related deaths in India occur in persons under 65 years of age in contrast to 12 % CVD deaths in US in the same age range [14]. It is projected that by 2015 CVD will be the single most important cause of mortality in India [15].
Major risk factors for CVD (including hypertension, diabetes, dyslipidemia and obesity) and modifiable risk behaviours (tobacco use, unhealthy diet, physical inactivity and harmful use of alcohol) are the leading cause of death and disability in most countries. Worldwide high blood pressure accounts for 12.8 % of total annual deaths (3.7 % DALYs) [1, 2]. The overall prevalence of hypertension is high in LMICs (40 %) [1]. Further, low income countries like China and India share a huge proportion of global burden of diabetes. In 2013, India was the largest contributor of diabetes related deaths (1.1 million) in the South East Asian region. India is home to over 65.1 million diabetic patients which is estimated to increase to about 109 million by 2035 [16]. Moreover, due to "Asian Indian Phenotype”, Indians get the disease at least 5-6 years earlier than their western counterparts [17]. Around 18 % of men and 21 % of women were insufficiently physically active and physical inactivity accounted for 3.2 million deaths and 32.1 million DALYs annually in LMICs [3•]. This varies within LMICs from a high of 51.5 % in Bhutan and 48.6 % in Brazil to 14 % in India and 4.7 % in Bangladesh. Around a third of adults in lower middle income countries had raised total cholesterol (Table 1).
Determinants of CVDs
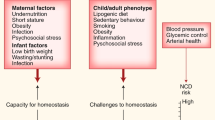
Multiple cohort studies like the Framingham Heart study from the US, WHO MONICA study, and INHEART study have provided valuable insights into the risk factors and determinants of CVDs. Pathway to CVD involves multiple drivers including social determinants (globalization, urbanization, ageing, income, education, housing) which lead to behavioural risk factors (tobacco use, unhealthy diet, physical inactivity, harmful use of alcohol). Prolonged unhealthy behaviours over many years lead to metabolic and/or physiological changes such as hypertension, diabetes, dyslipidemia, obesity which translates into CVD epidemic (heart, stokes and failure) [18]. These behavioural and metabolic risk factors coexist, thereby increasing cumulative CVD risk for an individual.
Risk Factors
Hypertension
Undetected and uncontrolled hypertension is a major cause of stroke worldwide [3•]. According to the Global burden of disease study 2010, high blood pressure levels or hypertension is the leading risk factor for CVDs, being positively associated with risk of ischemic heart disease and stroke [19].
Diabetes
CVD accounts for about 60 % of all mortality in diabetic people. The risk of CVD event is two to three times higher in people with diabetes [3•, 18]. A recent study of 50,000 Chinese adults revealed that diabetes was associated with a doubling of the odds of prevalent cardiovascular disease [20].
Dyslipidemia
Raised blood cholesterol increases the risk of heart disease and stroke. Globally, one third of ischemic heart disease is attributable to hypercholesterolemia [2, 21]. High levels of both cholesterol and low density lipoprotein is causally associated with Ischemic heart disease [21].
Overweight and Central Obesity
Overweight/obesity is a precursor to number of CVD risk factors. Extensive review concluded that measures of general obesity (e.g. BMI) and measures of abdominal adiposity (e.g. waist circumference, waist–hip ratio and waist–height ratio) are associated with CVD risk factors and incidence of CVD events [22]. For any given level of BMI, waist circumference or waist–hip ratio, the absolute risk of diabetes or hypertension (risk factors for CVD incidence) is higher among South Asians (Indians) than in Caucasian adults [23].
Risk Behaviours
Inappropriate Nutrition or Diet
Frequent consumption of energy dense foods, rich in saturated fat, trans fat and cholesterol predisposes an individual to CVD risk factors like obesity and dyslipidemia. A recent systematic review suggests protective associations between vegetables, nuts, monounsaturated fatty acids and a “Mediterranean” style, high-quality diet and coronary heart disease (CHD), and harmful associations with the intake of trans fatty acids and foods with a high glycemic index or load [24]. High salt intake increases risk of hypertension but in most populations, the level of salt consumption is higher than WHO recommendations (5 g/person/day) [25].
Reduced Physical Activity
Reduced physical activity is an established risk factor for CVD. Studies have shown that reduced physical activity leads to increased CHD and stroke in dose response manner [26]. The US Surgeon General report concluded that regular physical activity decreases the risk of CVDs and CHDs [27]. A recent meta-analysis of prospective cohort studies revealed that high level of leisure time physical activity reduces the risk of incident coronary heart disease and stroke among both men (RR 0.76 95 % CI 0.70–0.82, p < 0.001) and women (RR = 0.73, 95 % CI 0.68–0.78, p < 0.001). Further, moderate level of occupational activity was protective in both men (RR = 0.89, 95 % CI 0.82–0.97, p = 0.008) and women (RR = 0.83, 95 % CI 0.67–1.03) [28].
Smoking and Smokeless Tobacco use
Smoking is estimated to cause nearly 10 % of CVD. Prospective cohort studies have shown the beneficial effects of smoking cessation on coronary heart disease mortality [2, 3•].
Alcoholism
Harmful use of alcohol accounted for an estimated 4.5 % of DALYs globally [20]. High levels of alcohol consumption (>60 g of pure alcohol per day) is reported to be associated with risks of CVD. Worldwide an estimated 14 % of alcohol related deaths are caused by CVD and diabetes [3•].
Environment as a Determinant of CVD
Though the major CVD risk behaviours are rooted in individual choices, the immediate environments in which an individual lives are often not conducive for establishing healthy behaviours. The current environment brought about by globalization of food and agriculture, aggressive advertising and promotion of unhealthy food products, alcohol and tobacco industry encourages the over-consumption of obesogenic energy-dense and unhealthy foods. The challenge is further exaggerated due to high pricing of healthy food options. Poor urban planning and lack of provision of safe lanes for healthy modes of transport like cycling, restricts the opportunity for habitual physical activity.
Imperatives for Public Health Action in LMICs
Most LMICs currently focus on managing acute conditions and emphasize symptomatic care of late stage disease. These countries require affordable, cost effective and operationally feasible interventions that can be contextualized to the specific settings and are sensitive to the available resources. Evidence suggests that modifying risk behaviours can explain 44-76 % decline in CHD mortality while treatment explains 23-47 % [29]. Strategies of dietary salt control and tobacco control are estimated to prevent one million deaths per year in LMICs at a cost of US$0.50 per person per year [30].
Evidence from HICs suggests that CVDs are largely preventable as the major CVD risk behaviours including tobacco use, exposure to second hand smoke, consumption of food high in fats, sugar, and salt, lack of physical activity and excessive use of alcohol are avoidable and modifiable [31]. The biggest challenge with LMICs is the lack of adequate health resources and capacities for CVD prevention and control. It is estimated that out of 178 countries only 50 % countries had a national NCD plan consistent with the global NCD action plan. Only 56 % countries had strategies/policies to reduce physical inactivity, 60 % to promote healthy diet and 52 % to reduce harmful effects of alcohol [32].
WHO has developed a comprehensive global monitoring framework and an action plan for NCD prevention and control (2013-2020). This acts as a roadmap for member countries to develop contextualized frameworks, set priorities and make policies for prevention and control of CVDs, towards achieving a set of nine voluntary global targets by 2025. The targets primarily aim at reducing CVD risk behaviours through relative reduction in current tobacco use, prevalence of insufficient physical activity, mean population intake of sodium/salt and harmful use of alcohol. Further, the targets also aims to provide therapeutic interventions and counselling to at least half of individuals who are at high risk of developing CVDs and ensure availability of affordable diagnosis and treatment to more than three fourths of patients in both public and private facilities [33•].
Most LMICs are currently formulating national guidelines to address population wide NCD risks, however these countries are at varying levels of capacities to address the upsurge of CVDs. WHO has recommended a set of cost-effective and affordable interventions termed as “best buys” (Table 2) which can be prioritized for implementation in resource constrained settings [34•]. These can be contextualized based on local needs and feasibility of implementation in each country. It has been estimated that the economic losses due to ischemic heart disease and stroke would be three times higher than the actual cost of scaling up “best buy” interventions [6]. A focused two-pronged approach of “population-based” interventions and “high-risk individual” based interventions may be pragmatic and operationally feasible to address the rising CVD epidemic in LMICs.
Population Based Interventions
Health Promotion
Health promotion through education and media is an effective strategy to influence public attitudes, behaviours and policy making. Studies have shown that mass media interventions to reduce salt consumption, smoking cessation and improve dietary characteristics have been cost effective. The North Karelia project addressed high CHD mortality rates through comprehensive community interventions comprising mass-media campaigns and activities, engaging primary health care to improve the preventive services, collaborating with food industry and relevant policy changes. This resulted in 73 % fall in coronary heart disease in North Karelia and 63 % in the rest of Finland [35]. Mass media campaigns for diet/cholesterol in Kyrgyzstan reduced total serum cholesterol by 2 % [36]. Further, mass media interventions for smoking cessation has shown 2 % decline in smoking prevalence and strategies like increasing price of cigarettes led to 5-15 % reduction in smoking related deaths [37•].
Reducing dietary salt intake is a cost-effective intervention to reduce heart disease and stroke [38]. Worldwide, 2.5 million CVD deaths can be prevented by reducing salt intake to less than 5gm/day [20]. Mass campaigns for salt reduction showed that total dietary salt intake reduced by 20 % in Kyrgyzstan [35] and by 15 % in Vietnam [39].
Recent evidence has shown that CVD risk factors and risk behaviours originate in fetal life and infancy and rise during early life years establishing a pattern that persists throughout life [40]. Increasing awareness about the requisite interventions to prevent CVDs and its catastrophic impact should begin early in life and continue through the life course. Schools are ideal settings to initiate healthy behaviours among children which could potentially get established for life. Interventions at schools, worksites and communities to raise awareness about country specific dietary recommendations including harmful effects of trans fatty acids and high salt intake and knowledge about food labelling would enable people to make informed healthy choices. Schools and workplaces are also ideal settings for interventions to increase knowledge, and modify attitudes and behaviours related to physical activity.
High-risk Individual Based Interventions
Early Screening and Initial Management at Primary Health Care Units
People with established CVD or those at high risk of CVDs require individual level interventions to avoid acute events such as heart attacks, strokes and cardiac failure. Primary health care units in context of LMICs include, both government owned health facilities and privately owned clinics which are easily available, accessible, affordable and are the first point of contact for all health needs of the population. As CVDs have slow rate of progression, early screening of high risk individuals at primary health care units can prevent acute conditions thereby reducing cost of hospitalization, health care and out of pocket expenditure. Prevalence of undiagnosed hypertension and diabetes is high in LMICs like India [41], and those diagnosed have limited or poor access to proper treatment. Many LMICs lack population wide surveillance data on CVD. Screening of individuals with high risk of CVD based on a combination of risk factors is an effective strategy for settings where mass screenings are implausible due to resource constraints.
Prevention of CVDs cannot be addressed without strengthening primary care [3•] which are key for timely and appropriate screening and initial management of CVD events in LMIC settings. In some countries like India, Bangladesh, Nepal etc. in both rural and urban areas, the primary health care providers may be an untrained or non- allopathic physician. Key strategies for strengthening primary care centres in LMICs would include engaging, motivating and training non physician health staff (such as nurses, community health workers and non-allopathic practitioners) for service delivery of CVD including basic screening procedures, determining the level of CVD risks, initial management and timely and effective referral to secondary or tertiary level of health care if required. Further ensuring availability of essential medications and technologically advanced screening devices as well as strengthening of referral system within different levels of healthcare service delivery would be essential. Individual level counselling by trained non-physician health personnel at primary care centres can motivate people who are at medium to high risk and also those with established CVD for acquiring healthy behaviours.
Pharmacological Interventions
Key pharmacological interventions include multi drug therapy in primary care for people at high risk of developing heart attacks and strokes and providing acetylsalicylic acid for acute myocardial infarction [42]. Use of aspirin and low cost drugs for hypertension and hypercholesterolemia among high risk individuals can prevent 2 million deaths per year, costing US$1.00 per year per person [43]. Drugs to lower blood pressure are found to be very cost effective in LMICs. In a study conducted in South Africa, treatment of high BP resulted in 10 mm Hg lowering of BP, yielding 40 % RR reduction in stroke and 14 % reduction in CHD [44]. Drug treatments using multi drug therapy or polypill which contains fixed dose combination of multiple drugs like beta blockers, statins and angiotensin converting enzymes inhibitors are effective in preventing recurrence and complications of CVD [45]. Polypills are recommended for LMICs as they cost less than multiple individual drugs and lead to improved compliance.
Rehabilitation
Rehabilitation measures such as graded physical activity, appropriate dietary recommendation, knowledge about management of diabetes and hypertension, sufficient support for de-addiction to smokers, smokeless tobacco users and alcohol consumers are required. In Thailand, use of nicotine replacement therapy (NRT) showed increased likelihood of smoking cessation (OR = 1.66). Also there was a 5 % increase in use of NRT by those who quit smoking [42, 46]. Regular follow up and monitoring by trained health professionals are required for those who quit harmful practices of sustained tobacco and alcohol use.
Policy Interventions
Public health policies are pivotal for creating a conducive environment for CVD prevention and control and are also effective means of sensitizing various stakeholders and the community. Though behaviours are individual choices, they are embedded in wider social environments which are in turn influenced by wider public policies. Any change is unlikely to happen based solely on health promotion and health system strategies. The CVD determinants cuts across different sectors including health, finance, education, transport, food, trade, agriculture, environment and urban planning. Prevention and control measures demand multi-sectoral actions and coherent policy responses from all sectors.
Modifying Dietary and Physical Activity Behaviours
Policy interventions aimed at modifying dietary behaviours to prevent CVDs include reducing intake of saturated fats, replacing trans fatty acids with polyunsaturated fats, reducing intake of salt, and increasing consumption of fruits, vegetables and whole grains. This involves increasing taxes on unhealthy foods, sugar sweetened and carbonated beverages. The revenue generated by levying these taxes can be used for providing subsidies on healthy foods, and increasing production, storage and marketing fruits and vegetables. Legislative measures are required to regulate food industries to reduce amount of salt added to processed food, ensure nutrition and salt labelling on packed foods and consumer education through electronic media. Evidence from LMICs has shown that salt reduction policies are cost effective and regulation on salt in food has shown reduction in total dietary salt intake by 30 % [47].
With strict adherence to policies in developed countries, food industries are now aiming at potential markets in the developing world. LMIC countries require strict policies to regulate marketing of unhealthy foods and non-alcoholic beverages to children, which in turn need healthy school policies to ensure enabling environment for children to establish and practice healthy behaviours. Increased screen time and advertisements influence the food choices made by children and youth. Key celebrities should be sensitized and refrained from advertising tobacco and alcohol products, and unhealthy foods and beverages that impact children most. Policies on raising taxes on unhealthy foods and beverages can generate revenue which can be used to further promote healthy behaviours in the population.
Physical activity recommendations will need to be contextualized to LMIC resources and settings. Comprehensive and concurrent public policies across transport, urban planning, and sports are needed to provide enabling environment for promoting physical activity in the population. Rapid urbanization in LMICs has led to mushrooming of unplanned cities in many LMICs, which lack sufficient infrastructure and green spaces. It also leads to sedentary jobs, motorized transportation and unsafe traffic which limit people to engage in recommended levels of physical activity. This calls for country specific policies involving multi-sectoral actions aiming at provision for appropriate built environment and for promoting physical activity for all age groups. School policies need to ensure adherence to the mandate of regular physical education and adequate levels of physical activity among children and encouraging school staff and parents to be good role models.
Availability of safe and healthy spaces for undertaking physical activity remains a challenge in LMIC countries. Exercise recommendations for individuals with CVD or at high risk of CVD, would have to take into account the likely non-availability of requisite equipments in such settings. Physical activity recommendations for cardiovascular patients would involve an essential pre-exercise assessment to assess the cardiovascular risk category of low, medium or high CVD risk and preclude any contra-indications and advise an appropriate regimen of graded physical activity.
Tobacco Control
The international convention on tobacco control called by WHO (2003) provided the global framework and strategies for all signatory countries for tobacco control. In 2008, WHO provided a set of six focus areas for implementation, commonly referred by the acronym MPOWER which provides the route map for tobacco control at national level for each country. It is noteworthy that CVD risk factors such as tobacco use are more prevalent and rising among the LMIC countries and among lower socio-economic strata in all countries, which have less access to expensive health care and de-addiction centres. In addition to this, the tobacco industry is now targeting women and youth in LMICs which has resulted in increase of tobacco use among youth and women.
It has been shown that CVD mortality could decrease by 20 % within months of implementing ban on smoking in enclosed public places [48]. These tobacco control measures are highly cost effective, as the cost of demand reduction measures in LMICs is estimated to be US$0.11 per person of the population [3•]. However, since the regulatory and enforcement mechanisms in most LMICs are very weak, it would be important to prioritize and scale up the tobacco quitting support services to individual tobacco users as an intervention to potentially reduce the prevalence in these countries.
Reduce the Harmful use of Alcohol
Alcohol control strategies could include regulating availability of alcoholic beverages, including and ensuring strict adherence to minimum legal age of purchasing alcohol, restrictions on time of sale, raising taxes on alcoholic drinks and strict comprehensive bans on advertising alcohols. Treatment of alcohol use disorders and rehabilitation measures for those who quit heavy alcohol consumption is essential.
Role of the ICCPR
The International Council of Cardiovascular Prevention and Rehabilitation (ICCPR) was created in 2011 by a group of experts dedicated to the promotion of cardiovascular disease prevention and cardiac rehabilitation. It was formed with the help of a funding grant received from the Canadian Institute of Health Research. The ICCPR consists of leading experts from around the world. ICCPR is an Associate International Member of the World Heart Federation. At present it is made up of over 20 representative associations from all five main continents. In keeping with its primary goals the ICCPR is currently working on a consensus statement on a cardiac rehabilitation (CR) delivery model for low-resource settings. The purpose of this position statement is to review the literature on low-cost approaches to delivering the core components of CR, to propose a testable model of CR for these settings, as well as to make recommendations on how to increase CR delivery capacity.
Conclusion
CVD epidemic continues to grow in LMICs and imposes huge socio-economic burden on the population. Countries are required to set national targets and identify priority areas of immediate policy actions and health care interventions. A combination of population based and high risk individual based strategies which are evidence based, cost-effective, feasible as well as scalable would reduce CVD mortality and its devastating impact in low and middle income countries.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
World Health Organization. Global Status Report on non-communicable diseases 2010. Geneva: WHO; 2010.
World Health Organization.: Global health risks: mortality and burden of disease attributable to selected major risks. WHO Geneva. 2009. Accessed online at: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf
Mendis S, Puska P, Norrving B et al.: Global Atlas on Cardiovascular Disease Prevention and Control World Health Organization Geneva, Switzerland.2011.This publication provides comprehensive overview on CVD prevention and control, including updated estimates of CVDs and associated risk factors.
World Health Organization.: Causes of death 2008, WHO Geneva 2008 accessed online at http://www.who.int/healthinfo/ global_burden_disease/ cod_2008_sources_methods.pdf.
Pearson TA, Jamison DT, Trejo-guarez H. In Jamison DT, ed. Disease control priorities in developing countries. New York: Oxford University Press, 1993; 577-99
World Health Organization and World Economic Forum. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. Geneva, Switzerland: World Health Organization and World Economic Forum: 2011; Accessed online at : www.who.int/nmh/publications/best_buys_summary.
World Health Organization. World Health Statistics.2008; accessed online at www.who.int/whosis/whostat/EN_WHS08_Full.pdf.
World Health organisation. Country cooperation strategy at a glance., 2013; accessed online at http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_ind_en.pdf.
Xu K. Household catastrophic health expenditure: A multicountry analysis. Lancet. 2003;362:111–7.
World Development Indicators. Accessed online at data.worldbank.org/data…/world-development-indicators.
Engelgau MM, Saharty S, Kudesia P, et al. Capitalizing on the demographic transition: Tackling noncommunicable diseases in South Asia. World Bank: Washington, DC; 2011.
Fowkes F, Gerald R, Rudan D, Rudan I, Aboyans V, Denenberg JO, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013;382(9901):1329–40.
Gaziano TA. Reducing the growing burden of cardiovascular disease in the developing world. Health Aff. 2007;26(1):13–24.
Lopez AD, Murray CC. The global burden of disease, 1990-2020. Nat Med. 1998;4:1241–3.
Upadhyay PR. An overview of the burden of non-communicable diseases in India. Iranian J Publ Health. 2012;41(3):1–8.
International Diabetes Federation (IDF). Diabetes Atlas 2013. Accessed online at http://www.idf.org/diabetesatlas.
Xavier D, Pais P, Devereaux PJ, Xie C, Prabhakaran D, Reddy KS, et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–42.
World Health Organization. A global brief on high blood pressure (hypertension): preventing heart attacks, strokes and kidney failure. Geneva: WHO; 2013.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Bragg F, Li L, Smith M, Guo Y, Chen Y, Millwood I, et al. Associations of blood glucose and prevalent diabetes with risk of cardiovascular disease in 500 000 adult Chinese: the China Kadoorie Biobank. Diabet Med. 2014;31(5):540–51.
Varbo A, Benn M, Tybjærg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128(12):1298–309.
Huxley R, Mendis S, Zheleznyakov E, Reddy S, Chan J. Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk–a review of the literature. Eur J Clin Nutr. 2010;64(1):16–22.
Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3(3):141–6.
Mente A, De Koning L, Shannon HS, et al. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69.
Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567.
Kodama S, Shiro T, Yoriko H, Kazuya F, Chika H, et al. Association Between Physical Activity and Risk of All-Cause Mortality and Cardiovascular Disease in Patients With Diabetes A meta-analysis. Diabetes Care. 2013;36(2):471–9.
US Department of Health and Human Services, Physical Activity and Health: A report of the Surgeon General. Atlanta, Ga: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for disease Control and Prevention and Health Promotion: 1996.
Li J, Siegrist J. Physical activity and risk of cardiovascular disease—a meta-analysis of prospective cohort studies. Int J Environ Res Publ Health. 2012;2:391–407.
Ford ES, Capewell S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annu Rev Public Health. 2011;32:5–22.
Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: Health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–53.
Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, et al. UN High-Level Meeting on Non-Communicable Diseases: addressing four questions. Lancet. 2011;378:449–55.
Mendis S, Chestnov O. The Global Burden of Cardiovascular Diseases: A Challenge to Improve. Curr Cardiol Reports. 2014;16(5):1–9.
World Health Assembly. Global Action Plan for the Prevention and Control of NCD 2013-2020, (WHA 66.10). Geneva, Switzerland: World Health Organization: 2013. This publication provides a roadmap and a menu of policy options which could enable member countries to respond more effectively to achieve national and global targets to combat the rising NCD epidemic.
WHO (2011) Prevention and control of NCDs: priorities for investment, Discussion paper http://www.who.int/nmh/publications/who_bestbuys_to_prevent_ncds.pdf Accessed on 17th May 2014. This publication provides assessment of interventions to address NCDs and its underlying risk factors, using four key criteria viz. health impact, cost-effectiveness, feasibility and cost of implementation.
Puska P. Successful prevention of non-communicable diseases: 25 years of experiences with North Karelia Project in Finland. Public Health Med. 2002;4(1):5–7.
Akkazieva B, Chisholm D, Akunov N, Jacab M. The health effects and costs of the interventions to control cardiovascular disease in Kyrgyzstan 2009; Available online at http://hpac.kg/images/pdf/prp60cvd_eng.pdf.
Shroufi A, Chowdhury R, Anchala R, Stevens S, Blanco P, et al. Cost effective interventions for the prevention of cardiovascular disease in low and middle income countries: a systematic review. BMC Public Health. 2013;13(285):1–13. This publication systematically assesses the evidence on cost effectiveness for preventive CVD intervention in low and middle income countries.
World Health Organisation. Salt reduction and iodine fortification strategies in public health. WHO. 2014; accessed online at http://www.who.int/nutrition/publications/publichealth_saltreduc_iodine_fortification/en/.
Ha DA, Chisholm D. Cost-effectiveness analysis of interventions to prevent cardiovascular disease in Vietnam. Health Policy Plan. 2010;26:210–22.
De Boo HA, Harding JE. The developmental origins of adult disease (Barker) hypothesis. Aust N Z J Obstet Gynaecol. 2006;46(1):4–14.
Joshi SR, Banshi S, Muruga V, Dani SI, Mithal A, et al. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India—results from the Screening India's Twin Epidemic (SITE) study. Diabetes Technol Ther. 2012;14(1):8–15.
World Health Organization. Prevention of cardiovascular disease: Pocket guidelines for assessment and management of cardiovascular risk. Geneva: WHO; 2007.
Lim SS et al. Prevention of cardiovascular disease in highrisk individuals in low-income and middle-income countries:Health effects and costs. Lancet. 2007;370:2054–62.
Gaziano TA, Steyn K, Cohen DJ, Weinstein M, Opie L. Cost-effectiveness analysis of hypertension guidelines in South Africa: absolute risk versus blood pressure level. Circulation. 2005;112(23):3569–76.
Gaziano Thomas A, Opie LH, Weinstein MC. Cardiovascular disease prevention with a multidrug regimen in the developing world: a cost-effectiveness analysis. Lancet. 2006;368(9536):679–86.
Gilbert AR, Pinget C, Bovet P, Cornuz J, Shamlaye C, Paccaud F. The cost effectiveness of pharmacological smoking cessation therapies in developing countries: a case study in the Seychelles. Tob Control. 2004;13(2):190–5.
Murray CJL, Lauer JA, Hutubessy, Niessen L, Tomijima N, Lawes CM, et al. Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular-disease risk. Lancet. 2003;361(9359):717–25.
Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis. J Am Coll Cardiol. 2009;54:1249–55.
Compliance with Ethics Guidelines
Conflict of Interest
Aashish Contractor, Monika Arora, Kiran Saluja and Bidyut K Sarkar have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Physical Activity
Rights and permissions
About this article
Cite this article
Contractor, A., Sarkar, B.K., Arora, M. et al. Addressing Cardiovascular Disease Burden in low and Middle Income Countries (LMICs). Curr Cardiovasc Risk Rep 8, 405 (2014). https://doi.org/10.1007/s12170-014-0405-6
Published:
DOI: https://doi.org/10.1007/s12170-014-0405-6