Abstract
Background
Little attention has been paid to within-person daily associations among light physical activity (PA), moderate-to-vigorous physical activity (MVPA), and sedentary behavior (SB) with subsequent bodily pain and fatigue. Daily reports of pain and fatigue are less likely to be affected by recall bias and to conflate days of high and low pain/fatigue into one overall score.
Purpose
The purpose of this study was to examine daily within-person associations between pain, fatigue, and physical health and ascertain whether such associations are moderated by individual differences in these variables.
Methods
Participants were 63 community-living older adults (female n = 43, mean age = 70.98 years). Questionnaires measured typical levels of PA, SB, bodily pain, fatigue, and physical health. Subsequently, on a daily basis over a 1-week period, participants’ levels of light PA, MVPA, and SB were measured using accelerometers. Participants completed a questionnaire rating their pain and fatigue at the end of each day.
Results
Multilevel modeling revealed positive within-person associations between daily light PA, daily MVPA, and pain, as well as negative within-person associations between daily SB and pain. For individuals with higher typical levels of fatigue, there was a negative association between daily light PA, MVPA, and fatigue. For individuals with better levels of physical health, there was also a negative association between daily MVPA and fatigue. For those with higher typical levels of fatigue and better levels of physical health, there was a positive association between daily SB and fatigue. No such interaction effects were found between high levels of typical pain and PA or SB.
Conclusions
Our findings indicate that efforts to promote daily PA in older adults might be more effective for those who report high typical levels of fatigue and physical health, compared to those who report high levels of daily physical pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
According to the United Nations [1], the number of older adults (≥60 years) worldwide is expected to increase from 901 million in 2015 to 1.4 billion by 2030. As adults age, they are more likely to experience negative health outcomes (e.g., heart disease, back pain) [2]. For example, evidence shows that many older adults in community settings suffer from bodily pain (63% in men, 91% in women) [3] and fatigue (15% in men, 29% in women) [4]. Bodily pain has been found to be negatively related to walking speed, balance, and physical functioning in older women in community settings [5]. With regard to fatigue, positive associations have been reported between this variable and negative health conditions (e.g., arthritis) in older adults [6].
It is well documented that lifestyle factors such as physical activity (PA) and sedentary behavior (SB) can play an important role in determining health-related quality of life in older adults [7]. Evidence shows a positive association between engaging in moderate-to-vigorous PA (MVPA) and improved physical health (e.g., decreased risk of mortality, stroke, type 2 diabetes) [8] and mental health (e.g., fewer depression symptoms) in older adults [9]. In light of recent literature that has identified a high prevalence of light PA in the general public [10], particularly in older adults, research has also examined the role of light PA in improved physical health. Previous studies have reported positive associations between the engagement in light PA and the reduction of coronary heart disease in adults and older men [11], as well as fewer depression symptoms in older adults [9].
In contrast, spending a large proportion of the day in SB among older adults (age 70–85 years; men 67.8%, women 66.3%) [12] can have a negative impact upon health. For example, Stamatakis et al. [13] found that engagement in self-reported SB was associated with a higher cholesterol ratio, BMI, and waist circumference in older adults. Taken together, this evidence indicates that lifestyle factors such as light PA, MVPA, and lower SB are important predictors of health. Evidence has also accumulated regarding the role of light PA, MVPA, and SB in predicting two important indices of health, namely, bodily pain, and fatigue.
Physical Activity, Sedentary Behavior, and Bodily Pain
Engagement in self-reported PA has been related to less back pain in older adults [14]. In line with this, PA is recommended as a treatment for chronic pain [15]. Additionally, higher levels of sitting time have been associated with worse bodily pain in community-living older adults [16]. However, the associations between pain and PA are complicated and seem to be influenced by the level at which these associations are investigated. For example, exploration of within-person associations in older adults revealed that daily levels of PA were a significant predictor of higher levels of daily pain in women, even though overall/typical PA was associated with lower levels of pain [17]. In line with this finding, there is also evidence that some older adults, who report that activity worsens their pain, also use exercise to manage their pain [18]. Interestingly, the interference of pain with activity was particularly evident in those with severe levels of pain [18], suggesting that typical pain could influence the association between daily pain and daily PA. Within-subject analyses can be used to explore the associations between daily pain and daily PA in more detail, while exploring the moderating influence of typical pain on these associations [17]. In addition, given the negative associations between physical health and pain [19] and between physical health and SB [20], as well as the positive associations between physical health and PA [21], it is also important to examine the moderating influence of physical health in the association between daily PA/SB and daily pain.
Daily self-reports are less likely to be affected by recall bias and to conflate days of high and low pain into one overall score of pain. Further, by separating within-person from between-person associations, it is possible to ascertain the degree to which variables correlate with each other within the same individual over time, without such correlations being influenced by between-person differences in the levels of these variables [22]. As noted by Curran et al. [23], virtually all theories in the psychological sciences postulate joint within- and between-person processes. Omitting either of these two components results in a disjunction between theory and statistical testing. From an applied perspective, understanding true within-person associations over time helps to develop more tailored interventions.
Physical Activity, Sedentary Behavior, and Fatigue
Several studies have shown that fatigue is associated with restricted activities [24], lower levels of PA [25, 26], and more dependency in activities of daily living [27]. With regard to SB, it has been shown that sedentary adults report higher levels of fatigue compared to active adults [28, 29]. There is also evidence that exercise interventions can reduce fatigue in adults aged 55 years and older and that the improvements in fatigue are related to the improvements in PA [26]. Similar to the research on pain, however, the relation between fatigue and PA has been mainly examined at the between-person level. Nevertheless, feelings of fatigue can vary at the within-person (i.e., daily) level [30], and these within-person changes in fatigue are negatively related to changes in PA [31]. Interestingly, levels of typical fatigue have also been negatively related to diurnal PA patterns and physical health (chronic conditions) [32], suggesting that when exploring the associations between fatigue and PA at within-person level, typical levels of fatigue and physical health should be taken into account.
Purpose of the Study
Our aim was to examine the relation between daily (over a 7-day period) light PA, MVPA, and SB, and subsequent bodily pain and fatigue. We also investigated whether such associations were moderated by individuals’ typical levels of bodily pain, fatigue, and physical health. This is the first attempt to examine within-and between person associations of light PA, MVPA, and SB with subsequent bodily pain and fatigue in older adults. It was hypothesized that daily light PA and MVPA would predict lower levels of daily pain, whereas daily SB would predict higher levels of pain, but only for those with low levels of typical pain and high levels of physical health. In addition, it was hypothesized that daily light PA and MVPA would predict lower levels of fatigue, whereas daily SB would predict higher levels of fatigue, but only for those with low levels of typical fatigue and high levels of physical health.
Method
Participants
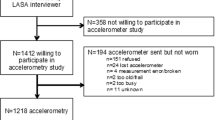
Older community-dwelling adults (n = 67) in the UK were recruited. Inclusion criteria were that participants did not use a walker or a wheelchair and were above the age of 60 years. Simulation studies (e.g., McNeish and Stapleton; Maas and Hox) [33, 34] indicate that N > 50 at level 2 (participants in our case) of a multilevel model provides adequate power for variance, standard error, and fixed effects estimates. A list of contacts was provided to the researchers from a database of about 1000 volunteers who were registered with a UK university as potential participants for studies on aging-related topics. Participants were sent invitation letters and/or e-mails. In total, 63 participants (n = 63, M age = 70.98 years, SD = 6.92, female = 68.3%) were included in the analysis, after four participants were excluded (not sufficient accelerometer wear time = 2, using a walker = 2) from the analysis. As can be seen in Table 1, the participants had an average body mass index (BMI; kg/m2) of 25.14 (SD = 3.47), were well educated (highest degree obtained = a post-graduate degree; 28.6%), and had a comfortable income (£20,000–£35,000 = 34.9%). The participants were mostly white and British (79.4%) and more than one third of the participants were co-habitating (65.1%) with their partner. Many participants (57.1%) reported having been diagnosed with a cardiovascular condition.
Procedures
Ethical approval for this study was granted by the Ethical Review Committee at a UK university. An introductory session about the study took place in an initial session in a lab or in a convenient place for the participant. The participants signed written consent forms. Their weight and height were then measured to calculate BMI (kg/m2) using a portable scale (TANITA BC-545N). Two participants refused to be measured, and their self-reported weight and height were recorded. At the beginning of the study, a set of questionnaires was distributed to the participants to provide pre-diary typical measures of the study variables, including demographics. Further, either a palmtop computer (Scroll Pocket Tablet PC) or a smartphone (ZTE Blade Q Mini Android Smartphone), depending on equipment availability, was given to the participants for the daily assessments. The devices were programmed to prompt a set of daily questions between 4 p.m. and 9 p.ms every day on a random basis. The devices had touch-.screens which participants had to tap to record an answer. If the participants did not respond to the first alarm, a second alarm was provided 2 min later. If there were no answers, the question was treated as missing (n= 45). Answers that were outside of the alarm range due to system errors were treated as missing (n = 1). The answers were stored within each participant’s device. At the end of the data collection, research staff downloaded the answers from the devices to a lab-based desktop computer. In addition to the touchscreen devices, an accelerometer was distributed to the participants to wear over 7 days during waking hours. Participants were instructed to wear the monitor on their right hip to avoid wearing the accelerometer during any water activities, and to record in a diary each time point when they started and stopped wearing the accelerometer.
Measures
Demographics
We asked participants to tick whether they were diagnosed with any cardiovascular disease over the past 12 months. We assessed the occurrence (have = 1, do not have = 0) of high cholesterol, heart disease, vascular disease, high blood pressure, and circulatory problems. In addition, gender (male = 0, female = 1) and marital status (living alone = 0, living with someone else = 1) were coded.
Typical and Daily Bodily Pain
For typical pain, participants were asked to complete the two pain items from the Research and Development (RAND) 36-Item Health Survey [35] [i.e., “How much bodily pain have you had during the past 4 weeks?” ranging from 1 (none) to 6 (very severe), and “During the past 4 weeks, how much did pain interfere with your normal work (including both work outside the home and housework)?”, ranging from 1 (not at all) to 5 (extremely)]. The coefficient alpha (α) was 0.78 in a previous study [35] and α = 0.79 in the present study. Items were averaged for our analysis. To measure daily bodily pain, we asked one item: “How much bodily pain do you have right now?”, and responses were rated on a 1 (no pain) to 4 (severe pain) scale.
Typical and Daily Fatigue
The Multidimensional Fatigue Index (MFI-20) [36] was utilized to assess fatigue over the previous 4 weeks with a total of 20 items. The scale tapped five dimensions of fatigue: general fatigue (e.g., “I feel tired”), physical fatigue (e.g., “Physically, I feel able to only do a little”), reduced activity (e.g., “I think I do very little in a day), mental fatigue (e.g., “My thoughts easily wander”), and reduced motivation (e.g., “I do not feel like doing anything). Answers were rated on a 5-point scale from 1 (yes, that is true) to 5 (no, that is not true). Good internal reliability coefficients were found in a previous study (α range 0.75–0.94) [36] and in the present study (α range 0.67–0.83). Subscales were summed to calculate a total fatigue score. To assess daily fatigue, one item (“How much fatigue do you feel right now?”) was chosen from the MFI and was answered at each beep. Participants provided a rating from 1 (no fatigue) to 4 (severe fatigue).
Daily Physical Activity and Sedentary Behavior
Accelerometers were used to monitor PA and SB levels (model GT3X+ was worn by 47 participants, and model WGT3X-BT was worn by 16 participants). The two models have been shown to produce very similar results [37], and this was also the case in our study according to the results of one-way MANOVA (Pillai’s trace = 0.01, F (3, 59) = 0.19, p = 0.91; follow-up univariate ANOVAs: SB F (1, 61) = 0.19, p = 0.67; light PA F (1, 61) = 0.00, p = 0.98; and MVPA F (1, 61) = 0.1, p = 0.76). Hence, in our analysis, we combined the data from the two types of accelerometers. Participants who wore the accelerometer a minimum of 10 h a day for 5 days, including one weekend day over 7 days, were included in the analysis. Data were extracted using the ActiGraph software. The researcher programmed the monitor to accumulate movement data every 60 s. Non-wear time was classified as 90 min of consecutive non-activity counts (<100 counts) with 2 min of tolerance allowance [38].Based on the diary the participants recorded, we set a time filter to standardize wearing time (7:30 a.m. to 10:30 p.m.). For the purposes of our analysis, for each day and for each participant, we utilized the movement data accumulated from the morning until the time they answered the daily questions on bodily pain and fatigue. Hence, in our analysis, daily PA and SB were used as predictors of daily bodily pain and fatigue.
Counts per minute were processed to categorize the thresholds of activities [i.e., SB 0–99 counts per minute (cpm) [12], light PA 100–2019 cpm, moderate PA 2020–5998 cpm, and vigorous PA ≥5999 cpm] [39]. Moderate and vigorous intensities were summed to represent MVPA. Finally, each activity category (light PA, MVPA, and SB) was divided by the total wear days and then multiplied by 100 to represent the proportion of each activity category, in order to reduce inter-participant variability [10, 40]. These proportion scores were used in the main analysis.
Typical Health Status
The RAND 36-Item Health Survey was administered to measure physical health [35]. Participants were told: “The following questions are about activities you might do during a typical day. During the past 4 weeks, has your health limited you in these activities? If so, how much?” Rating scales varied depending on items (e.g., carrying groceries). Higher scores on the fours subscales represented better physical health [35]. Good internal consistency coefficients have been found in adults (mean age = 30.54, α = 0.89) [41], and this was also the case in the current study (α = 0.75).
Typical Physical Activity
Typical PA was assessed using the Physical Activity Scale for the Elderly (PASE) [42]. In total, 18 items were rated using 4-point scales (hours/week) (e.g., “How much time was spent on the activity over the last 7 days?”) and yes/no questions (e.g., “Have you performed ‘light housework’ over the last 7 days?”). The items captured seven dimensions of PA (e.g., walking, light sport/recreation). Items were multiplied by the number of hours the participants spent and were weighted and summed to obtain an overall score of PA [43]. People with higher scores were more physically active. Acceptable Cronbach’s alpha for reliability was 0.73 in a previous study with older adults [ 44 ], but somewhat lower in our study (α = 0.56).
Typical Sedentary Behavior
Typical sedentary time was assessed with seven items from the Measure of Older adults’ Sedentary Time (MOST) [45]. The survey asked the participants to record their total sedentary time (hours and minutes) over the previous 7 days (e.g., watching television). Items were summed with higher scores representing higher levels of SB. Test-retest reliability was found to be acceptable (intraclass correlation coefficient = 0.52, 95% confidence interval = 0.27–0.70) in older adults [45]. The Cronbach’s alpha coefficient is not applicable for this scale.
Data Analysis
Linear mixed models (IBM SPSS, version 22) were tested to examine within- and between-person associations between light PA, MVPA, and SB with bodily pain and fatigue. We ran four models in total. In the first two, light PA and MVPA predicted bodily pain and fatigue respectively, and in the other two models SB predicted pain and fatigue respectively. Within-person predictors (level 1; daily light PA, daily MVPA, and daily SB) were person-mean centered. At level 2, the average of daily light PA, daily MVPA, and daily SB over the 7 days were entered as predictors. By including the predictor average scores over the 7-day period at level 2, the level 1 within-person associations were not conflated by between-person differences [22]. In addition, we tested the cross-level interactions between each of the level 1 predictors with typical pain (when predicting daily pain), with typical fatigue (when predicting daily fatigue), and with physical health (when predicting daily pain and fatigue). BMI, age, presence/absence of cardiovascular disease, gender, and co-habitating were also entered at level 2 as covariates. Level 2 predictors were uncentered [46]. All level 1 and 2 predictors, apart from the categorical ones, were converted into Z scores to obtain β coefficients from the analysis. R 1 2 was estimated as an effect size, representing the amount of variance at level 1 explained by the predictors, compared to the variance explained by a model with only the intercept [47].
Results
Participants completed 341 (77.3%) out of 441 (over 7 days) daily questions on bodily pain and fatigue. The percentage of missing cases for the pre-diary survey was around 3.2%. The skewness scores for the dependent variables of bodily pain (1.89) and fatigue (0.93) were within an acceptable range (skewness ±2) [48]. Daily light PA and SB were highly correlated (r = −0.83, p < 0.01) as is often the case in the literature; hence, separate models for light PA and SB were run.
Table 2 shows that the participants wore accelerometers for almost 10 h (594.13 min) before they answered the daily questions. The participants spent most of their time in SB (58.58%) and light PA (35.80%), with a lower proportion of MVPA (5.62%). According to R 1 2, models 1 and 2 (Table 3) predicted 52.8% (bodily pain) and 21.0% (fatigue) of the variance at level 1. Also, models 3 and 4 (Table 4) accounted for 54.8% (bodily pain) and 19.1% (fatigue) of the variance.
Daily Light PA, MVPA, and Daily SB Predicting Bodily Pain
Table 3 shows the standardized coefficients (β) and standard errors for level 1 and level 2 predictors of bodily pain. Engagement in daily light PA (β = 0.151, p = 0.009), daily MVPA (β = 0.110, p = 0.023), and higher levels of typical pain (β = 0.543, p<0.001) positively predicted bodily pain experienced at the daily level. No other significant associations were found. Typical bodily pain and physical health did not significantly moderate the associations between daily light PA, MVPA, and bodily pain. Table 4 shows that typical pain (β = 0.515, p < 0.001) and daily SB (β = −0.182, p = 0.003) over the 7 days predicted bodily pain at the daily level. No other associations were significant.
Daily Light PA, MVPA, and SB Predicting Fatigue
Table 3 depicts that daily light PA and MVPA did not significantly predict fatigue. However, a number of significant interactions emerged. Those interactions were further probed via simple slope analyses, for which we report unstandardized coefficients. Specifically, for individuals with lower levels of typical fatigue, there was a positive association between daily light PA and daily fatigue (β = 3.28, p < 0.001), whereas for those with higher levels of typical fatigue, this association was negative (β = −3.22, p = 0.001). For those with lower levels of typical fatigue, there was also a positive association between daily MVPA and daily fatigue (β = 3.49, p < 0.001), whereas for those with higher levels of typical fatigue, this association was negative (β = −3.41, p < 0.001). For individuals with lower typical levels of physical health, there was a positive association between daily MVPA and fatigue (β = 2.93, p = 0.027), whereas for those with higher levels of typical physical health, this association was negative (β = −2.85, p = 0.034). Typical levels of physical health did not significantly interact with light PA to predict daily fatigue. With regard to main effects, typical fatigue (β = 0.263, p = 0.031) and cardiovascular disorder (β = 0.483, p = 0.014) were also significantly associated with daily fatigue.
Simple slope analyses were also conducted to probe significant interactions in Table 4. Specifically, for individuals with lower typical levels of fatigue, there was a negative association between daily SB and fatigue (β = −4.612, p < 0.000), whereas for those with higher levels of typical fatigue, this association was positive (β = 4.513, p < 0.000). For individuals with lower typical levels of physical health, there was a negative association between daily SB and fatigue (β = −3.779, p = 0.019), whereas for those with higher levels of typical physical health, this association was positive (β = 3.680, p = 0.022). With regard to main effects, typical fatigue (β = 0.274, p = 0.026) and the presence of cardiovascular diseases (β = 0.489, p = 0.013) also predicted daily fatigue.
Discussion
In this study, we examined daily associations between objectively assessed light PA, MVPA, and SB, and subsequent bodily pain and fatigue in a sample of older adults. Further, we explored whether these within-person associations were moderated by between-person differences in typical bodily pain, fatigue, and physical health.
Predictors of Bodily Pain
We expected that daily light PA and MVPA (and SB) would be negative (positive) predictors of daily pain, but only for those with low levels of typical pain and better levels of health. Contrary to our hypothesis, the within-person associations of daily light PA and MVPA with daily bodily pain were positive, in that more engagement in daily light PA and MVPA predicted more subsequent bodily pain. However, this finding is in line with a previous study in which a positive within-person association was found between PA and pain in a sample of older adults [17]. With respect to daily SB and bodily pain, the analysis showed that more engagement in daily SB was associated with less subsequent bodily pain in older adults. This finding is aligned with our results pertaining to PA and pain.
Even though engagement in PA might predict higher levels of bodily pain in the short term in older adults, it is well established that regular PA can maintain and improve health in older adults [49, 50]. In fact, there are studies showing a negative as opposed to a positive association between PA and pain (e.g., Cecchi et al. [14]). Given these apparently inconsistent findings regarding the associations between PA and pain, more research is needed to explore the temporal effects of PA on pain in more detail. Future studies may need to utilize more frequent measurement points (e.g., hourly). Given some reports that feelings of pain can fluctuate throughout the day [50], it is possible that PA/SB might predict pain in different ways depending on the time of the day. It would also be interesting to explore the impact of the type of activity on the associations between PA and pain. For example, lifting heavy objects and gardening could have differential effects on the relationship between pain and PA.
Finally, typical physical health did not moderate the associations between pain and PA or SB. It should be acknowledged though that the overall perceived physical health of the participants was good (i.e., 81 out of 100). Therefore, in order to explore this hypothesis in the future, it is important to include a sample with a greater variation in perceived physical health.
Predictors of Fatigue
We expected that daily light PA and MVPA (and SB) would be negative (positive) predictors of daily fatigue, but only for those with low levels of typical fatigue and better levels of physical health. The results partially supported our hypotheses. There were no significant within- and between-person associations between light PA, MVPA, SB and subsequent fatigue. Other studies have generally reported modest negative associations between fatigue and PA [25, 51]. Such modest and/or non-significant associations could be due to the possibility that the relations between PA, SB, and fatigue are dependent on individuals’ levels of health and their general levels of fatigue.
Better typical levels of physical health moderated the association between daily MVPA and fatigue and between SB and fatigue. As hypothesized, those who engaged in more MVPA and less SB reported less fatigue, but this was the case only for individuals with better perceived health. In contrast, for those with worse perceived health, engagement in more MVPA and less SB was detrimental as it resulted in more daily fatigue. Interestingly, physical health did not moderate the association between light PA and fatigue. These findings suggest that intensive forms of PA should be reserved for those in better physical health, while those in lower physical health should initially be prescribed light PA. Given that physical health did not influence the associations between light PA and fatigue, perhaps light PA would be the most suitable type of PA to start an intervention to reduce fatigue for older adults. Increasing light PA might not only benefit levels of fatigue and physical health, but it is also a feasible target for older adults who are not active.
Contrary to our hypothesis, the expected negative (positive) association between daily light PA (SB) and subsequent daily fatigue were evident only for those individuals with high (as opposed to low) typical fatigue levels. The current findings suggest that those with higher typical levels of fatigue might benefit more in terms of their daily fatigue levels from moving more and sitting less than those with lower levels of typical fatigue. Even though exercise interventions have been shown to reduce the levels of fatigue [52], even in clinical populations with high levels of fatigue such as rheumatoid arthritis [53] and multiple sclerosis [54], to our knowledge, little attention has been paid to the moderating role of typical levels of fatigue on these benefits. Therefore, the possibility that those with higher levels of typical fatigue might benefit more from being physically active in terms of their daily fatigue should be investigated in future intervention studies. Our findings also highlight the need to focus PA-promoting interventions in older adults on individuals who report high levels of fatigue and perhaps experience chronic fatigue. Given that higher levels of light PA were associated with lower levels of fatigue in those with higher levels of typical fatigue, perhaps PA-promoting interventions for this particular population should focus on light PA. As mentioned above, this is likely to be a feasible target for people who are not physically active, and such type of activity can help to increase overall health [55, 56].
Limitations and Future Research Directions
We must acknowledge some limitations of the present study. The standardized coefficients associated with the main effects of daily SB, light PA and MVPA were small. However, such effects are in line with our research in the pain and fatigue literatures utilizing objective assessments of PA [ 25, 51 ]. Given that our participants were generally inactive, 1 SD increases in daily SB, light PA, and MVPA represent substantial deviations from the sample’s mean scores on those variables. It should be also considered that objective PA and self-reported pain and fatigue do not share common method variance, as is the case with self-reported PA. Another limitation of the study is that due to its short duration (7 days), we do not know the extent to which our findings would generalize over a longer period of time (e.g., 2 or 3 months). A measurement burst approach [57] in which diaries are administered on multiple occasions (e.g., 3 weeks over a year) would allow for a test of seasonal effects (e.g., due to the weather). Assessing multiple activities and rates of fatigue and pain throughout the same day can also offer a more comprehensive understanding of the dynamic nature of the relations between these two variables, PA and SB. In addition, objectively assessed PA cannot readily differentiate between different modes of activity (e.g., lifting heavy objects vs. playing with children) which can predict variations in perceptions of pain and fatigue. Another limitation of the study was that the sample was rather ethnically homogenous, relatively educated, relatively healthy (e.g., low bodily pain and fatigue scores), quite wealthy, and thus not wholly representative of the general population of older adults in the UK. Future studies should aim to recruit older adults from more diverse backgrounds. Further, another limitation was that we used self-reported measures of health. In future investigations, it might be informative to replicate our study using objective assessments of physical health (e.g., field-based tests of gait speed or hand grip strength).
Notwithstanding the limitations above, this study has several strengths. This is the first study to examine within-person associations between light PA, MVPA, SB, and subsequent daily pain and fatigue in older adults. We were able to establish support for such within-person associations which were not confounded by individual differences in PA and SB. In addition, advancing past research, we specifically measured light PA because in older adults, a high proportion of time is spent engaging in this type of PA [10, 58]. Indeed, we found that engagement in daily light PA represented 35.80% of the daily activity up to the measurement of pain and fatigue, a much higher percentage than that for MVPA (5.62%). We measured levels of PA and SB both objectively and via self-reports. In contrast, most of the previous studies have only used self-reports of PA and/or SB in predicting bodily pain and fatigue. By using smart devices for EMA, we were able to obtain real-time reports of pain and fatigue. Future studies in this field could build on our findings to develop targeted PA interventions for individuals with varying levels of fatigue and pain. Such interventions could use modern technology (e.g., smartphones) to target beliefs, barriers, and benefits of being more physically active and less sedentary.
References
United Nations. World population ageing 2015.; 2015. http://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf.
World Health Organization. 10 facts on ageing and health. http://www.who.int/features/factfiles/ageing/en/. Published 2016.
Bergh I, Steen G, Waern M, et al. Pain and its relation to cognitive function and depressive symptoms: a Swedish population study of 70-year-old men and women. J Pain Symptom Manag 2003;26(4):903–912. doi:10.1016/S0885-3924(03)00329-4.
Vestergaard S, Nayfield SG, Patel K V, et al. Fatigue in a representative population of older persons and its association with functional impairment, functional limitation, and disability. J Gerontol 2009;64A(1):76–82. doi:10.1093/gerona/gln017.
Sampaio RAC, Sewo Sampaio PY, Uchida MC, et al. Walking speed and balance performance are associated with short-form 8 bodily pain domain in Brazilian older female. J Clin Gerontol Geriatr 2015;6(3):89–94. doi:10.1016/j.jcgg.2015.02.005.
Williamson RJ, Purcell S, Sterne A, et al. The relationship of fatigue to mental and physical health in a community sample. Soc Psychiatry Psychiatr Epidemiol 2005;40(2):126–132. doi:10.1007/s00127-005-0858-5.
Vogel T, Brechat P-H., Leprêtre P-M., et al. Health benefits of physical activity in older patients: a review. Int J Clin Pract 2009;63(2):303–320. doi:10.1111/j.1742-1241.2008.01957.x.
World Health Organization. Global strategy on diet, physical activity and health-physical activity and older adults. http://www.who.int/dietphysicalactivity/factsheet_olderadults/en/. Published 2016.
Loprinzi PD. Objectively measured light and moderate-to-vigorous physical activity is associated with lower depression levels among older US adults. Aging Ment Health 2013;17(7):801–805. doi:10.1080/13607863.2013.801066.
Owen N, Sparling PB, Healy GN, et al. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc 2010;85(12):1138–1141. doi:10.4065/mcp.2010.0444.
Sesso HD, Paffenbarger RS, Lee I-M. Physical activity and coronary heart disease in men: the Harvard Alumni Health Study. Circulation 2000;102(9):975–980. doi:10.1161/01.CIR.102.9.975.
Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol 2008;167(7):875–881. doi:10.1093/aje/kwm390.
Stamatakis E, Davis M, Stathi A, Hamer M. Associations between multiple indicators of objectively-measured and self-reported sedentary behaviour and cardiometabolic risk in older adults. Prev Med (Baltim) 2012;54(1):82–87. doi:10.1016/j.ypmed.2011.10.009.
Cecchi F, Debolini P, Lova RM, et al. Epidemiology of back pain in a representative cohort of Italian persons 65 years of age and older: the InCHIANTI study. Spine (Phila Pa 1976) 2006;31(10):1149–1155. doi:10.1097/01.brs.0000216606.24142.e1.
Connelly P. Guidance on the management of pain in older people. Age Ageing 2013;42:i1-i57. doi:10.1093/ageing/afs200.
Balboa-Castillo T, León-Muñoz LM, Graciani A, Rodríguez-Artalejo F, Guallar-Castillón P. Longitudinal association of physical activity and sedentary behavior during leisure time with health-related quality of life in community-dwelling older adults. Health Qual Life Outcomes 2011;9(1):47. doi:10.1186/1477-7525-9-47.
Ho A, Ashe MC, DeLongis A, Graf P, Khan KM, Hoppmann CA. Gender differences in pain-physical activity linkages among older adults: lessons learned from daily life approaches. Pain Res Manag 2016:9. doi:10.1155/2016/1931590.
Brown ST, Kirkpatrick MK, Swanson MS, McKenzie IL. Pain experience of the elderly. Pain Manag Nurs 2011;12(4):190–196. doi:10.1016/j.pmn.2010.05.004.
Reyes-Gibby CC, Aday L, Cleeland C. Impact of pain on self-rated health in the community-dwelling older adults. Pain 2002;95(1):75–82. doi:10.1016/S0304-3959(01)00375-X.
Rezende LFM de, Rodrigues Lopes M, Rey-López JP, Matsudo VKR, Luiz O do C. Sedentary behavior and health outcomes: an overview of systematic reviews. Lucia A, ed. PLoS One. 2014;9(8):e105620. doi:10.1371/journal.pone.0105620.
Haider S, Luger E, Kapan A, et al. Associations between daily physical activity, handgrip strength, muscle mass, physical performance and quality of life in prefrail and frail community-dwelling older adults. Qual Life Res 2016;25(12):3129–3138. doi:10.1007/s11136-016-1349-8.
Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Vol 1. Sage; 2002.
Curran PJ, Howard AL, Bainter SA, Lane ST, McGinley JS. The separation of between-person and within-person components of individual change over time: a latent curve model with structured residuals. J Consult Clin Psychol 2014;82(5):879–894. doi:10.1037/a0035297.
Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313. doi:10.7326/0003-4819-135-5-200109040-00007.
Egerton T, Chastin SFM, Stensvold D, Helbostad JL. Fatigue may contribute to reduced physical activity among older people: an observational study. Journals Gerontol Ser A Biol Sci Med Sci 2016;71(5):670–676. doi:10.1093/gerona/glv150.
Nicklas BJ, Beavers DP, Mihalko SL, Miller GD, Loeser RF, Messier SP. Relationship of objectively-measured habitual physical activity to chronic inflammation and fatigue in middle-aged and older adults. Journals Gerontol Ser A Biol Sci Med Sci 2016;71(11):1437–1443. doi:10.1093/gerona/glw131.
Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. J Gerontol A Biol Sci Med Sci 2010;65(8):887–895. doi:10.1093/gerona/glq064.
Ellingson LD, Kuffel AE, Vack NJ, Cook DB. Active and sedentary behaviors influence feelings of energy and fatigue in women. Med Sci Sports Exerc 2014;46(1):192–200. doi:10.1249/MSS.0b013e3182a036ab.
Wennberg P, Boraxbekk C-J, Wheeler M, et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open. 2016;6(2):e009630. doi:10.1136/bmjopen-2015-009630.
Ravesloot C, Ward B, Hargrove T, et al. Why stay home? Temporal association of pain, fatigue and depression with being at home Disabil Health J 2016;9(2):218–225. doi:10.1016/j.dhjo.2015.10.010.
Murphy SL, Kratz AL, Williams DA, Geisser ME. The association between symptoms, pain coping strategies, and physical activity among people with symptomatic knee and hip osteoarthritis. Front Psychol. 2012;3(SEP).
Egerton T, Helbostad JL, Stensvold D, Chastin SFM. Fatigue alters the pattern of physical activity behavior in older adults: observational analysis of data from the generation 100 study. J Aging Phys Act 2016;24(4):633–641. doi:10.1123/japa.2015-0237.
McNeish DM, Stapleton LM. The effect of small sample size on two-level model estimates: a review and illustration. Educ Psychol Rev 2016;28(2):295–314. doi:10.1007/s10648-014-9287-x.
Maas CJM, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology 2005;1(3):86–92. doi:10.1027/1614-2241.1.3.86.
Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item health survey 1.0. Health Econ 1993;2(3):217–227. doi:10.1002/hec.4730020305.
Smets EMA, Garssen B, Bonke B, De M, Haes JCJ. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res 1995;39(3 SRC):315–325. doi:10.1016/0022-3999(94)00125-o.
Miller J. Cross-generation accuracy. 2015. http://actigraphcorp.com/wp-content/uploads/2015/04/cross-generation-accuracy.pdf.
Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc 2012;44(10):2009–2016. doi:10.1249/mss.0b013e318258cb36.
Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40(1):181–188. doi:10.1249/mss.0b013e31815a51b3.
Bélanger M, Townsend N, Foster C. Age-related differences in physical activity profiles of English adults. Prev Med (Baltim) 2011;52(3):247–249. doi:10.1016/j.ypmed.2011.02.008.
Padden DL, Connors RA, Agazio JG. Stress, coping, and well-being in military spouses during deployment separation. West J Nurs Res 2011;33(2):247–267. doi:10.1177/0193945910371319.
Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 1999;52(7):643–651. doi:10.1016/S0895-4356(99)00049-9.
Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol 1993;46(2):153–162. doi:10.1016/0895-4356(93)90053-4.
Loland N. Reliability of the physical activity scale for the elderly (PASE). Eur J Sport Sci 2002;2(5):1–12. doi:10.1080/17461390200072504.
Gardiner PA, Clark BK, Healy GN, Eakin EG, Winkler EAH, Owen N. Measuring older adults’ sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc 2011;43(11):2127–2133. doi:10.1249/MSS.0b013e31821b94f7.
Bolger N, Laurenceau J. Intensive Longitudinal Methods. New York: Guilford Press; 2013.
Hox J, Moerbeek M, Schoot R van de. Multilevel Analysis: Techniques and Applications. 2nd ed. New York: Routledge; 2010.
Gravetter F, Wallnau LB. Statistics for the Behavioral Sciences.Cengage Learning; 2016.
World Health Organization. Global Recommendations on Physical Activity for Health. 2011. http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf.
Focht B, Ewing V, Gauvin L, Rejeski W. The unique and transient impact of acute exercise on pain perception in older, overweight, or obese adults with knee osteoarthritis. Ann Behav Med 2002;24(3):201–210.
Mahieu MA, Ahn GE, Chmiel JS, et al. Fatigue, patient reported outcomes, and objective measurement of physical activity in systemic lupus erythematosus. Lupus 2016;25(11):1190–1199. doi:10.1177/0961203316631632.
Puetz TW, O’Connor PJ, Dishman RK. Effects of chronic exercise on feelings of energy and fatigue: a quantitative synthesis. Psychol Bull 2006;132(6):866–876. doi:10.1037/0033-2909.132.6.866.
Rongen-van Dartel SAA, Repping-Wuts H, Flendrie M, et al. Effect of aerobic exercise training on fatigue in rheumatoid arthritis: a meta-analysis. Arthritis Care Res (Hoboken) 2015;67(8):1054–1062. doi:10.1002/acr.22561.
Pilutti LA, Greenlee TA, Motl RW, Nickrent MS, Petruzzello SJ. Effects of exercise training on fatigue in multiple sclerosis. Psychosom Med 2013;75(6):575–580. doi:10.1097/PSY.0b013e31829b4525.
Manns PJ, Dunstan DW, Owen N, et al. Addressing the nonexercise part of the activity continuum: a more realistic and achievable approach to activity programming for adults with mobility disability? Phys Ther 2012;92(4):614–625. doi:10.2522/ptj.20110284.
Matthews CE, Moore SC, Sampson J, et al. Mortality benefits for replacing sitting time with different physical activities. Med Sci Sports Exerc 2015;47(9):1833–1840. doi:10.1249/MSS.0000000000000621.
Sliwinski MJ. Measurement-burst designs for social health research. Soc Personal Psychol Compass 2008;2(1):245–261. doi:10.1111/j.1751-9004.2007.00043.x.
Gando Y, Yamamoto K, Murakami H, et al. Longer time spent in light physical activity is associated with reduced arterial stiffness in older adults. Hypertension 2010;56(3):540–546. doi:10.1161/HYPERTENSIONAHA.110.156331.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval for this study was granted by the Ethical Review Committee at a UK university.
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards
Saengryeol Park, Cecilie Thøgersen-Ntoumani, Jet J. C. S. Veldhuijzen van Zanten, and Nikos Ntoumanis declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional/national) and with the Helsinki Declaration of 1975, as revised in 2000.
Additional information
This research was supported by the National Institute for International Education of South Korea (Grant Number: 2011-43).
About this article
Cite this article
Park, S., Thøgersen-Ntoumani, C., Veldhuijzen van Zanten, J.J.C.S. et al. The Role of Physical Activity and Sedentary Behavior in Predicting Daily Pain and Fatigue in Older Adults: a Diary Study. ann. behav. med. (2017). https://doi.org/10.1007/s12160-017-9921-1
Published:
DOI: https://doi.org/10.1007/s12160-017-9921-1