Abstract
Background
Web and mobile technologies appear to hold promise for delivering evidence-informed and evidence-based intervention to cancer survivors and others living with trauma and other psychological concerns. Health-space.net was developed as a comprehensive online social networking and coping skills training program for cancer survivors living with distress.
Purpose
The purpose of this study was to evaluate the effects of a 12-week social networking intervention on distress, depression, anxiety, vigor, and fatigue in cancer survivors reporting high levels of cancer-related distress.
Methods
We recruited 347 participants from a local cancer registry and internet, and all were randomized to either a 12-week waiting list control group or to immediate access to the intervention. Intervention participants received secure access to the study website, which provided extensive social networking capabilities and coping skills training exercises facilitated by a professional facilitator.
Results
Across time, the prevalence of clinically significant depression symptoms declined from 67 to 34 % in both conditions. The health-space.net intervention had greater declines in fatigue than the waitlist control group, but the intervention did not improve outcomes for depression, trauma-related anxiety symptoms, or overall mood disturbance. For those with more severe levels of anxiety at baseline, greater engagement with the intervention was associated with higher levels of symptom reduction over time.
Conclusions
The intervention resulted in small but significant effects on fatigue but not other primary or secondary outcomes. Results suggest that this social networking intervention may be most effective for those who have distress that is not associated with high levels of anxiety symptoms or very poor overall psychological functioning.
Trial Registration Number
The trial was registered with the ClinicalTrials.gov database (ClinicalTrials.gov #NCT01976949).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Individuals diagnosed with cancer encounter many challenges, including physical impairments, fatigue, cognitive impairments, pain, mood disturbance, disruptions in social support, and financial strains [1]. Estimates of clinically significant distress in cancer survivors vary, but larger studies suggest high prevalence (35.1 % in Zabora et al. [2]; 37.8 % in Carlson et al. [3], 55 % in Grassi et al. [4]). Fortunately, a mature literature on face-to-face psychosocial interventions for cancer generally suggests that psychological interventions, particularly those that deliver active coping skills training, can improve outcomes in cancer survivors. Systematic reviews and meta-analyses demonstrate reliable intervention effects on quality of life [5,6,7], emotional functioning [5, 8], and functional adjustment ([5]; see Newell et al. [9] for more conservative conclusions). In its own review, the Institute of Medicine concluded that “there is statistically significant, clinically relevant evidence to support the effectiveness of psychotherapeutic interventions in helping to manage anxiety or depression in adults with cancer—across disease sites, treatments, and types of interventions (p. 75)” [1]. Cancer-related distress is both common and treatable.
The adoption of distress screening and management guidelines by the American College of Surgeons (ACoS) Commission on Cancer [10] requires that all accredited cancer centers screen for, and have a plan for managing, cancer-related distress. However, it has been difficult for many healthcare systems to fully address the large number of patients who present with clinically significant distress. Even when resources are available, there are many other barriers to accessing available services [1, 3, 11], including mental health stigma, patients’ level of disease progression [12], difficulty scheduling appointments with providers [13], distance and travel constraints [14, 15], inadequate numbers of psychosocial staff [16], and providers’ lack of awareness of existing resources [17]. Online interventions and other behavioral health technologies offer a particularly promising approach to overcoming at least some of these barriers and potentially supplementing clinic-based efforts to address cancer-related distress, and interest in online services (e.g., 63 % of approached patients) is at least as high as interest in face-to-face services among those with cancer [18, 19].
However, relatively few randomized, controlled studies have tested behavioral health technologies to address cancer-related distress. Extant trials have primarily targeted breast cancer patients, and results suggest that they are most effective for those experiencing significant distress or impairment in quality of life. Gustafson et al. [20] evaluated the effects of a 6-month, home-based computer intervention (CHESS) that included informational content, a discussion board, confidential answers from cancer experts, and decision-support services on 255 women with breast cancer. Although the intervention resulted in improved information competence, comfort with participation in healthcare, and confidence in their doctor, it had no significant effects on quality of life or social support. In a study targeted to breast cancer patients (N = 72) with elevated depressive symptoms, Winzelberg et al. [21] examined the effects of a 12-week facilitated intervention (Bosom Buddies). The intervention significantly improved depressive symptoms, stress, and post-traumatic symptoms, and effect sizes were moderately strong (.37–.54). Additionally, Owen et al. [18] examined the effects of a 12-week, self-guided intervention (Survive) for 62 women with early-stage breast cancer. No main effects of the intervention were observed, but effect sizes were moderate for improvements in overall quality of life (.30) and emotional well-being (.38). Baseline health status moderated the effects of the intervention, such that the intervention resulted in significantly improved health status among women with poor health status at baseline relative to those in the control group. Taken together, these studies suggest that web-based behavioral health technologies are more effective for those experiencing impairments in mood or quality of life.
To be effective, online interventions must also be able to hold participants’ interest long enough to be able to deliver a sufficient dose of the treatment. Because attrition [22] is a substantial problem for many behavioral health technologies, it is critical to be able to provide interventions that are consistent with participants’ perceived needs and interests. For cancer survivors, social connections and interactions with peers are a primary motivator of participation in online interventions [23]. This may be one of the reasons why many of the most widely studied face-to-face interventions involve group interaction elements, such as support groups [24,25,26,27]. Interventions that marry evidence-based approaches from face-to-face interventions with social components that allow interactions between participants may be particularly effective at delivering online content. We have previously demonstrated that engaging with a social networking community in an online intervention for cancer survivors is associated with a fivefold increase in interaction with structured intervention elements, such as coping skills training exercises and psychoeducational content [28].
Other online interventions for cancer survivors have incorporated social elements with varying levels of quality, intensity, and success. Borosund et al. [29] and Ruland et al. [30] demonstrated that an internet-based messaging system to provide breast cancer patients with the ability to send questions to care providers and receive responses, a discussion forum for communicating with other patients, and a blogging tool resulted in significant, but quite small, improvements with respect to anxiety, depression, and symptom distress relative to a usual care control group. Use of the social tools, such as the discussion forum and blogs, was limited, such that the median number of posts per participant was zero in both the discussion forum and the blogs. An average of one advice message was sent, although participants did spend time reading what others had posted. Stanton et al. [31] found that providing breast cancer patients with a personal website and blog for communicating with friends and family members was successful in preventing increases over time in depressive symptoms, promoting positive mood, and increasing life appreciation. Additionally, the Cancer Support Community has a long history of providing professionally facilitated, weekly 90-min chat groups, which have demonstrated very promising levels of engagement, communication, and outcomes among mixed cancer types [32]. However, it has proved difficult to marry evidence-informed treatment materials (e.g., those from face-to-face interventions) with online intervention delivery. For example, Lepore et al. [33] tested pro-social internet support groups relative to standard internet support groups provided by the Cancer Support Community and found that encouraging women with early-stage breast cancer to engage in helping behaviors to other group members did not boost the effects of online support on depression and anxiety symptoms over time. Overall, online interventions in cancer survivors are promising, but studies are quite mixed with respect to how extensively they provide social networking features, attempt to treat cancer-related distress, or can be used in general cancer populations.
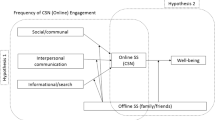
In the present study, we sought to address several limitations of the existing literature by developing and evaluating a comprehensive, social networking intervention for cancer survivors and targeting a broad range of survivors, all of whom were experiencing significant levels of psychological distress. We have previously developed an intervention for cancer-related distress, called “Survive,” using older web technologies, that demonstrated promising results, in terms of outcomes for those with significant impairments in quality of life, and engagement with an online, group-based format [18]. Survive is based on Folkman & Greer’s cancer-specific Model of Stress and Appraisal Coping [34] and incorporates two key elements of previously efficacious face-to-face interventions: supportive-expressive support group [24, 27] and coping skills training exercises [25, 26]. According to the Model of Stress and Appraisal Coping, those with cancer undergo two simultaneous processes specific to each of potentially many cancer-related stressors: (1) appraisal of the significance of the stressor to the individual and the resources available to the individual to handle the stressor and (2) efforts to cope with the stressor, using a combination of thoughts, behaviors, and emotions, that subsequently impact the stressor and/or the appraisals of the stressor [35]. According to this model, distress arises when efforts to cope with a stressor are followed by unfavorable outcomes.
Survive and health-space were both designed to increase the quantity and quality of stressor-specific coping efforts and promote meaning-based coping efforts for those stressors that are outside the control of the participant. Research in cancer survivors has consistently shown that avoidance-oriented coping efforts are related to more negative outcomes over time [36, 37], whereas adopting active-behavioral [38], active-cognitive [39], and active-emotional [40, 41] coping efforts are associated with improvements in mood and quality of life [42]. A number of trials have demonstrated positive outcomes associated with coping skills training exercises to reduce stress and improve mood, improve positive health-related coping behaviors, and to promote increased social engagement and support [21, 25,26,27].
Qualitative responses from participants in the pilot trial of Survive [18] suggested that participants expressed interest in having additional ways of connecting with one another, for simpler, more visually appealing coping skills training exercises and for materials that addressed the heterogeneous nature of cancer-related distress. In order to supplement the intervention, we conducted three major revisions to the Survive intervention (which was renamed “health-space”): (1) dramatically improving opportunities for social networking, by providing a weekly, 90-min professionally facilitated group chat, blogs, discussion board, and private mail, and (2) supplementing existing coping skills training exercises with additional content requested by previous participants, and (3) reducing reliance on text by condensing content and emphasizing its graphic design. These revisions have resulted in high levels of overall engagement (438 min per participant, total) in both social networking components of the intervention and coping skills training exercises [28].
The purpose of the present study was to pilot the effects of a web-based social networking and coping skills training intervention on cancer-related distress. Because distress is heterogeneous in presentation, we sought to test the effects of the intervention on several related patient-based outcomes, including cancer-related distress, depression, anxiety, psychological well-being, vigor, and fatigue. Accordingly, the present study had three aims. First, we sought to evaluate effect sizes and potential outcomes of a social networking intervention with respect to primary outcomes of psychological functioning, distress, depression, and anxiety and secondary outcomes of fatigue and vigor. Second, we sought to identify potential moderators of treatment efficacy in order to identify who benefitted most from the intervention. Third, we evaluated whether engagement, or dose of treatment, is associated with outcomes and whether the relationship between engagement and outcomes is stronger for those with more severe levels of distress.
Methods
Participants
After human subjects approval was obtained, participants were recruited from July 2009 to June 2012 through two primary strategies: (1) a registry of patients treated at Loma Linda University and (2) targeted outreach to cancer-related websites and online forums. Individuals recruited through the Loma Linda tumor registry were mailed a letter describing the study and providing options for learning more about the study or opting out of future contact. Potential participants who did not opt out were contacted by phone, provided additional information, and, if interested, screened for eligibility. Additionally, messages were sent to moderators of cancer-related websites and forums (e.g., Facebook, Google groups) providing a brief description of the study and a link for more information. In order to be eligible to participate, respondents were required to be at least 18 years of age, have consistent internet access, be able to read and write in English, and have a minimum score of a 4 of 10 on the Distress Thermometer (indicating significant distress over the past week; [43]).
Procedures
At baseline, participants used the study website to complete the consent form and initial survey. Upon completion of the initial survey, participants were randomized (1:1 ratio) to receive either immediate access to the intervention (treatment condition) or a 12-week waitlist condition (waitlist control group; ClinicalTrials.gov #NCT01976949). Randomization conditions were automatically assigned by computer using a random number generator. Those in the treatment group were informed that the intervention would last 12 weeks, and each participant’s progression through the study was clearly indicated on the study homepage. Treatment group participants were admitted to the social networking website on a rolling basis. Participants were asked to complete a follow-up survey 12 weeks after being randomized, and waitlist control participants were provided with access to the social networking website immediately after completing the follow-up survey. Participants were provided with a $10 Amazon gift card for completing each survey but not for participation in the social networking website.
The Health-Space Intervention
Health-space is a 12-week, multicomponent distress management intervention. The study website ( health-space.net ) provided access to 20–25 participants and two trained facilitators at any point in time. Primary components of health-space.net were weekly guidance modules, a live weekly, facilitated chat, a discussion board, personal profiles, and web-based email (i.e., “webmail”) for use in communicating with other participants and study facilitators. Each week participants were offered a new guidance module topic, adapted from materials used in two previous trials of coping skills interventions ( [18, 44, 45]; see Table 1) and consistent with other evidence-based therapies for cancer-related distress [21, 25,26,27]. Each module provided brief, graphically rich educational materials and activities for participants, such as quizzes and exercises designed to encourage each participant to actively engage with each weekly guidance module. Because participants joined the group on a rolling basis, it was not necessary to have learned the information from a previous week in order to make use of subsequent guidance modules.
All participation was facilitated by doctoral-level clinical psychology students. Facilitators had a minimum of 1 year of clinical experience and received extensive ongoing training in managing web-based support groups and working with cancer survivors using a supportive-expressive facilitation model [24]. In a 90-min, facilitated weekly chat, a facilitator reviewed the weekly guidance module and facilitated conversation around that theme, as well as invited current concerns of group members for discussion and problem solving. Facilitators met weekly with other facilitators and two of the investigators to review chat transcripts and ensure fidelity to the intervention. A copy of the facilitation manual can be obtained here: https://health-space.net/lab/healthSpaceFacilitationManual.pdf.
The discussion board provided a way for members to stay connected to the facilitators and other group members and was actively monitored by the group facilitator and study investigators. Participants and facilitators were invited to post messages to the group at any time to solicit feedback, update other members about their current situation, or follow-up on activities that were assigned during the weekly chat session. A webmail feature was also included in health-space.net, where participants had the option to email the entire group or only specific participants or facilitators [28]. In order to promote group cohesion, participants were also encouraged to create a profile in which they could describe themselves and their experience with cancer and/or share photos.
Measures
Demographic and Medical Characteristics
Age, gender, ethnicity, and cancer type were obtained from the tumor registry when available or by self-report from those recruited via the internet. Participants reported their level of education (in years), annual household income, current employment, marital status, time since diagnosis, cancer stage, days per month activities were restricted due to cancer, and the frequency of internet use.
Primary and Secondary Outcomes
Because cancer-related distress is multifactorial, we sought to measure several distinct markers of distress. Primary outcomes were distress, psychological functioning, depression, and trauma-related anxiety symptoms. Secondary outcomes were fatigue and vigor. All outcome measures were given at baseline and again after 12 weeks. The Distress Thermometer [44] asked participants to rate their level of distress on a 0–10 scale, with larger numbers indicating more distress. A cutoff score of 4 or higher has been demonstrated to provide the optimal balance between sensitivity and specificity for identifying significant clinical concerns in those with cancer [46, 47]. Overall psychological functioning was also measured with the Outcomes Questionnaire-45 (OQ-45; [48]), which consists of 45 five-point Likert items and has received extensive psychometric validation as a component of patient-based outcome monitoring [49]. The OQ-45 exhibited excellent internal consistency in the current sample (α = .92). Total mood disturbance was measured with the Profile of Mood States (POMS-SF; [50]). The POMS-SF required participants to identify, on a 5-point Likert scale, the extent to which they have experienced each of 37 distinct mood states in the previous week, ranging from “not at all” to “extremely.” The total mood disturbance score (α = .91) was used in this study, as were the POMS subscales for fatigue (five items, α = .90; [50]) and vigor (six items, α = .91; [50]). Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D; [51]), which is a 20-item measure that asks respondents to indicate how often they have experienced symptoms of depression within the past week, on a 4-point Likert scale, ranging from “rarely or none of the time” to “most or all of the time.” The CES-D is reliable (α = .92) and has been validated within cancer populations [50, 52]. Trauma-related anxiety symptoms were measured with the Impact of Events Scale-Revised (IES-R). The IES-R is a 22-item, Likert-type scale that measures intrusive and avoidant symptoms of cancer-related thoughts and stimuli [53]. This scale is sensitive to the effects of psychosocial intervention and has good internal consistency (Cronbach’s α = .79–.92; [40]).
Measures of Behavioral Engagement
Engagement was measured objectively via server-side scripting that provided time spent using the intervention and time spent using specific parts of the intervention, specifically structured intervention content (i.e., weekly coping modules) and social networking components (i.e., personal pages, blog, chat, email). Lengthy periods of inactivity (>30 min) were not included in totals of time spent using the intervention.
Statistical Analysis
The study was powered to detect a small effect size of .13 using repeated measures general linear modeling. Linear mixed modeling, whereby T1 and T2 outcome measures were nested within subjects, was used to evaluate changes over time and to accommodate missing data at T2. Because of significant positive skew for annual household income, positive outliers were removed (n = 14) for analyses involving income. Of the 235 subjects who completed T2, only 212 had complete data for OQ-45 at both T1 and T2 due to inadvertent late inclusion of the measure. In order to evaluate whether those with worse levels of psychological functioning at baseline benefited more from treatment, interaction terms were created using mean-centered indicators of baseline psychological functioning and group assignment. Any significant interactions were decomposed using methods recommended by Aiken and West [54]. Briefly, each significant interaction was visualized by identifying three “slices” of the continuous level of baseline psychological functioning: at the mean and 1 SD above or 1 SD below the mean.
Results
Recruitment and Attrition of Study Participants
Of the 2263 patients identified from the cancer registry, 49.9 % (n = 1130) were successfully reached and informed about the nature of the study. Just over 60 % (n = 683) of these were excluded from further consideration due to lack of interest (n = 220), lack of comfort using the internet (n = 140), difficulty with English (n = 56), being too sick (n = 42), or other unspecified reasons (n = 227). The remaining 40 % (n = 447) agreed to be screened for eligibility to participate in the trial. Internet recruitment resulted in screening of 756 unique visitors to the study website (see Fig. 1). It was not possible to determine the number of individuals who visited the study website but did not choose to be screened for eligibility.
Screenshot of the health-space.net home page
Across both recruitment arms, 1203 individuals were screened for eligibility, and 55.9 % (n = 706) were deemed to be eligible to join the trial. Of these, 49.2 % (n = 347) completed the baseline assessment and were randomized. Within the internet recruitment arm, distress was similar in those who completed the baseline assessment (M = 6.7, SD = 1.6) and those who did not (M = 6.5, SD = 1.6). Similarly, among those recruited from the cancer registry, distress did not differ between baseline completers (M = 5.7, SD = 2.6) and noncompleters (M = 5.9, SD = 2.2). Approximately one-third of randomized participants were lost to attrition, with 67.7 % (n = 235) completing the 12-week follow-up assessment. The relationship between recruitment source and attrition across time approached statistical significance, with 75 % of registry-recruited participants completing the 3-month follow-up relative to 64 % of internet-recruited participants, χ 2(1) = 3.80, p = .051. Attrition patterns did not differ between those assigned to the treatment condition and those assigned to the waitlist control.
Baseline Equivalence Between Treatment and Control Groups
Demographic and medical characteristics of the treatment and control groups are provided in Table 2. Randomization successfully resulted in no baseline differences between treatment and control groups with respect to age, gender, marital status, ethnicity, education, income, cancer type, cancer severity, or time since diagnosis. Similarly, recruitment source (65.2 % recruited via internet), frequency of internet use (M = 6.3 days/week), and previous online (35.2 %) or face-to-face support group (42.9 %) use did not differ between the two groups at baseline. As shown in Table 3, treatment and control groups did not differ at baseline with respect to any of the primary outcomes of interest: overall psychological functioning, depressive symptoms, anxiety, vigor, or fatigue. Based on OQ-45 scores, 59.4 % of participants met criteria for clinically significant psychological dysfunction. Similarly, 67.6 % of participants met the CES-D cutoff suggestive of clinical depression.
Effect of Treatment on Outcomes at 12 Weeks
Both the treatment group and the control groups showed improvements over time in each of the five outcome domains: psychological functioning, depressive symptoms, anxiety, vigor, and fatigue (see Table 3). The degree of improvement from baseline to 12 weeks did not significantly differ between the two groups for overall psychological functioning, depression, anxiety, or vigor. However, there was a time × treatment group interaction for fatigue, demonstrating that fatigue declined significantly more in the treatment group relative to the control group, t (238) = 2.0, p = .04.
Although all participants reported distress when screened for eligibility, 84.4 % remained distressed at the baseline assessment. By the 12-week follow-up, 65.1 % remained distressed, and the treatment groups did not differ significantly. Clinical cutpoints were also available for depressive symptoms. At baseline, 67.7 % (n = 235) met the clinically suggestive cutoff (67 % in the treatment group, 68 % in the waitlist control group). By the 12-week follow-up, only 34.3 % (n = 199) remained depressed (31 % in the treatment group compared to 38 % in the waitlist control group), but the between-group difference was not statistically significant (p = .15).
Moderators of Treatment Outcomes
Next, we sought to evaluate whether initial symptom severity moderated the effect of treatment group on change in symptoms across time. A significant baseline psychological functioning × treatment group interaction was observed, t (212) = 2.2, p = .03. Higher psychological functioning at baseline was associated with larger effects of treatment, and the effect of treatment was increasingly attenuated at lower levels of psychological functioning. Significant moderator effects were also observed for baseline levels of anxiety, t (240) = 2.0, p = .04. The treatment was significantly more effective at reducing anxiety for those who reported lower anxiety at baseline than for more highly anxious participants. The effects of treatment on vigor, fatigue, and depression were not significantly moderated by their baseline levels (see Table 3).
Effects of Engagement on Outcomes
To examine the effects of engagement with the intervention on subsequent outcomes in those assigned to the treatment condition (n = 176), three markers of intervention engagement were identified: total time spent using the intervention (in seconds) and total time spent interacting with the structured content of the intervention (i.e., coping modules). Analyses demonstrated no significant main effects on any dependent variable. However, the effects of engagement on outcomes were moderated by level of baseline symptoms for both psychological functioning and anxiety. Total time spent using the intervention approached significance, with time of engagement being more strongly associated with changes in psychological functioning as baseline symptoms increased, F (1, 105) = 3.91, p = .051, and more consistently posting content to the group was significantly more strongly related to changes in psychological functioning as baseline symptoms increased, F (1, 105) = 4.68, p = .033. Total time spent using the intervention was also more strongly associated with changes in anxiety as baseline anxiety symptoms increased, F (1, 115) = 8.74, p = .004 (see Fig. 2). Similarly, more consistently posting content to the group was more strongly related to decreases in anxiety at higher levels of baseline anxiety, F (1, 115) = 7.93, p = .006. There were no significant baseline symptom × engagement interactions for depression, vigor, or fatigue.
Discussion
The health-space social networking intervention for cancer-related distress was not associated with significant overall improvements in distress, psychological functioning, depression, anxiety, or vigor. Although the health-space intervention did not work as well as expected, results from this trial suggest that (1) the intervention is associated with strong levels of engagement [55], (2) health-space seems to have small effects on fatigue in those with significant distress, and (3) has its strongest effect on those with distress and worse psychological functioning and/or trauma-related anxiety. Among those who did have worse psychological functioning or worse trauma-related anxiety, greater improvements over time were associated with being more strongly engaged with the intervention (Fig. 3).
Surprisingly, both the treatment and waitlist control groups improved significantly over time in each of the observed outcomes. We have identified four potential explanations: regression to the mean, natural recovery, therapeutic mechanisms inherent to the study procedures, or use of other treatments or interventions. Regression to the mean seems an unlikely explanation given that significant distress is common in cancer survivors, and the sample was not particularly extreme with respect to distress. Natural recovery is certainly a possibility, given known variability in day-to-day distress ratings, and it may be that the process of completing a battery of psychologically sensitive questions and promising intervention access was sufficient to instill hope and other psychological benefits. Finally, it may be that the many different kinds of support services widely available on the internet made it possible for waitlist participants to seek and obtain the types of services needed to reduce distress. Although we did not have data to test this hypothesis, follow-up interviews [23] suggested that the vast majority of participants were relatively naïve to internet support services and did not report using competing services. Future trials of internet-based interventions should include more extensive measures of use of other types of support services, such as Facebook, Patients Like Me, etc.
The intervention did appear to have a significant, but small, effect on fatigue, and the effect size was slightly higher than that reported in a previous meta-analysis [56]. Participants in the health-space.net intervention were actively encouraged to engage in supportive-expressive interactions with other participants and to become more active and engaged in relationships, social activities, and physical activity, and these micro-interventions are consistent with mechanisms of action of other successful non-pharmacologic interventions for fatigue [57]. Given that fatigue has consistently been documented as the most prevalent unmet need for many cancer survivors [58, 59] and that ours was a sample of relatively long-term survivors (four years, on average), it is encouraging that a low-cost, internet-based intervention may be able to improve symptoms of fatigue. We have previously demonstrated that social networking may be most desirable when cancer survivors are able to communicate with other survivors who have faced similar cancer, treatment, and psychosocial challenges [23], and it may be that a fatigue-specific social networking intervention could result in more pronounced effects.
On average, the intervention appeared to have the most effect for those who entered the study with significant distress, but relatively higher levels of psychological functioning or lower levels of trauma-related anxiety. Given that all participants reported clinically meaningful levels of distress at baseline, it is important to note that “low” distress in this sample still represents significant psychosocial distress. These results are consistent with a stepped-care model of intervention [60] and suggest that more intensive, ideally face-to-face, interventions may be required for those cancer survivors with the highest levels of psychosocial distress. Additionally, the relationship between baseline distress and symptom improvement was moderated by engagement with the treatment. Those with high levels of distress or anxiety who were highly engaged with the intervention experienced more pronounced reductions in symptoms, whereas those who engaged at lower levels did not improve as much, and greater engagement was not associated with benefit for those with lower levels of distress or anxiety. Thus, those with lower (but still pronounced) distress are more likely to benefit, but those with more severe distress may also benefit when their engagement is high. Understanding the factors that encourage more consistent engagement with technology-based interventions is likely to be useful for increasing efficacy of these types of interventions. Social networking appears to be particularly promising for driving engagement and clearly accounts for a large proportion of overall time spent using the intervention [55]. Interviews with users who spent relatively little time with the intervention also suggest that more extensive efforts to tailor content to specific subsets of users could improve the effective dose of intervention provided to each user [23] and thereby have the potential to further improve effect sizes.
Regarding study limitations, as is true of many technology-based interventions [22], the sample was not particularly diverse with respect to gender, ethnicity, and educational attainment, and engagement was rather limited. Participants were encouraged to spend at least 1–2 h per week using the intervention, for a total of 12–24 h of engagement, but total average engagement across the 12 weeks of intervention was 7.3 h. Although these rates of engagement compare favorably with a number of other e-health interventions [55], there are notable examples of online interventions in cancer survivors that yield higher levels of involvement [61]. For example, in an online health behavior change intervention, Surviving and Thriving with Cancer, Bantum et al. [62] demonstrated very high levels of user participation, at least with respect to posting content. Because of differences in intervention content and procedures, in addition to differences in how engagement is measured across interventions, it is very difficult to evaluate which intervention elements are most critical for improving effect sizes. Studies that are able to decompose intervention elements and evaluate effects on engagement and outcomes would be particularly beneficial [63]. Additionally, although this intervention was designed for those with clinically significant levels of distress, for some, distress levels dropped between initial screening and randomization, and even the waitlist group reported significant reductions in distress over time. For those with transient distress, very brief interventions that can be immediately accessed might be a better fit, and this study is not able to address whether participants sought out other forms of web-based support. The study also relied exclusively on self-report measures without long-term (i.e., 12 months) follow-up, so little can be said with respect to the influence of psychiatric history, changes in psychiatric status (e.g., proportion meeting diagnostic criteria for a DSM-5 condition), or long-term maintenance of positive effects on fatigue. Finally, although we saw treating mixed cancer types as a way to reach the broadest representative sample of distress among cancer survivors, participants clearly expressed a desire to connect with “others like me” [23], and having a more homogenous sample with respect to cancer types and treatment trajectories may have resulted in stronger engagement and/or outcomes.
Technology-based interventions are clearly not for everyone, as demonstrated by the 60 % of those on the cancer registry who were approached but declined to be screened, and we would argue that behavioral technologies should only be one element of treatment planning efforts for those experiencing clinically significant distress. Our results show promise for reducing some prominent symptoms of distress, such as fatigue, particularly for those with low-grade distress and those who engage in more consistent use of the intervention. Certainly, a replication would be required to increase our confidence in these findings, but we believe the results are strong enough to warrant some degree of optimism about these kinds of interventions. Given high levels of engagement, subsequent efforts to use technology-based approaches for delivering distress-focused interventions to cancer survivors could certainly build upon this or a similar social networking framework to deliver other types of evidence-based interventions.
References
Institute of Medicine. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, D.C.: National Academies Press; 2007.
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncol. 2001; 10: 19–28.
Carlson LE, Angen M, Cullum J, et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004; 90: 2297–2304.
Grassi L, Johansen C, Annunziata MA, et al. Screening for distress in cancer patients: A multicenter, nationwide study in Italy. Cancer. 2013; 119: 1714–21.
Meyer TJ, Mark MM. Effects of psychosocial interventions with adult cancer patients: A meta-analysis of randomized experiments. Health Psychol. 1995; 14: 101–8.
Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: Meta-analysis of 37 published controlled outcome studies. Pat Educ Counsel. 2003; 50: 179–86.
Edwards AGK, Hailey S, Maxwell M. Psychological interventions for women with metastatic breast cancer (review). Cochrane Library. 2007; 4: 1–28.
Jacobsen P, Donovan K, Swaine Z, Watson I. Management of anxiety and depression in adult cancer patients: Toward an evidence-based approach. In Oncology: An Evidence-Based Approach. A. Chang, P. Ganz, D. Hayes, T. Kinsella, H. Pass, J. Schiller, R. Stone, V. Strecher (Eds.). New York: Springer-Verlag; 2006. p. 1552–1579.
Newell SA, Sanson-Fisher RW, Savolainen NJ. Systematic review of psychological therapies for cancer patients: Overview and recommendations for future research. JNCI. 2002; 94: 558–84.
Wagner LI, Spiegel D, Pearman T. Using the science of psychological care to implement the new American College of Surgeons Commission on Cancer distress screening standard. J Nat Comp Cancer Network. 2013; 11: 214–21.
Hewitt M, Rowland J. Mental health service use among adult cancer survivors: Analyses of the National Health Interview Survey. J Clin Oncol. 2002; 20: 4581–90.
Gustafson DH, Wise M, McTavish F, et al. Development and pilot evaluation of a computer-based support system for women with breast cancer. J Psychosoc Oncol. 1993; 11: 69–93.
Cunningham AJ, Edmonds CVI, Jenkins GP, et al. A randomized controlled trial of the effects of group psychological therapy on survival in women with metastatic breast cancer. Psycho-Oncol. 1998; 7: 508–17.
Owen JE, Klapow JC, Roth DL, et al. Improving the effectiveness of adjuvant psychological treatment: The feasibility of providing online support. Psycho-Oncol. 2004; 13: 281–92.
Fukui S, Kugaya A, Kamiya M, et al. Participation in a psychosocial group intervention among Japanese women with primary breast cancer and its associated factors. Psycho-Oncol. 2001; 10: 419–27.
Jacobsen PB, Meade CD, Stein KD, et al. Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol. 2002; 20: 2851–62.
Institute of Medicine National Research Council. Meeting Psychosocial Needs of Women with Breast Cancer. Washington, D.C.: National Academies Press; 2004.
Owen JE, Klapow JC, Roth DL, et al. Randomized pilot of a self-guided internet coping group for women with early-stage breast cancer. Annals of Behavioral Medicine. 2005; 30: 54–64.
Sanders SL, Bantum EO, Owen JE, Thornton AA, Stanton AL. Supportive care needs in patients with lung cancer. Psycho-Oncology. 2010; 19: 480–90.
Gustafson DH, Hawkins R, Pingree S, et al. Effect of computer support on younger women with breast cancer. Journal of General Internal Medicine. 2001; 16: 435–445.
Winzelberg AJ, Classen C, Alpers GW, et al. Evaluation of an internet support group for women with primary breast cancer. Cancer. 2003; 97: 1164–1173.
Eysenbach G. The law of attrition. Journal of Medical Internet Research. 2005; 7: e11.
Gorlick A, Bantum EO, Owen JE. Internet-based interventions for cancer-related distress: Exploring the experiences of those whose needs are not met. Psycho-Oncology. 2014; 23: 452–8.
Spiegel D, Classen C. Group Therapy for Cancer Patients: A Research-Based Handbook of Psychosocial Care. New York: Basic Books; 2000.
Fawzy FI, Canada AL, Fawzy NW. Effects of a brief, structured psychiatric intervention on survival and recurrence at 10-year follow-up. Archives of General Psychiatry. 2003; 60: 100–103.
Andersen BL, Yang HC, Farrar WB, et al. Psychologic intervention improves survival for breast cancer patients. Cancer. 2008; 113: 3450–3458.
Penedo FJ, Dahn JR, Molton I, et al. Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer. 2003; 100: 192–200.
Owen JE, Curran M, Bantum EO, et al. Characterizing social networks and communication channels in a web-based peer support intervention. Cyberpsychology, Behavior, and Social-Networking. 2016; 19: 388–96.
Borosund E, Cvancarova M, Moore SM, Ekstedt M, Ruland CM. Comparing effects in regular practice of e-communication and web-based self-management support among breast cancer patients: Preliminary results from a randomized controlled trial. J Med Internet Res. 2014; 16: e295.
Ruland CM, Andersen T, Jeneson A, Grimsbo GH, Borosund E, Ellison MC. Effects of an internet support system to assist cancer patients in reducing symptom distress: A randomized controlled trial. Cancer Nursing. 2013; 36: 6–17.
Stanton AL, Thompson EH, Crespi CM, Link JS, Waisman JR. Project connect online: Randomized trial of an internet-based program to chronicle the cancer experience and facilitate communication. J Clin Oncol. 2013; 31: 3411–17.
Lieberman M, Golant M, Giese-Davis J, et al. Electronic support groups for breast carcinoma: A clinical trial of effectiveness. Cancer. 2003; 97: 920–5.
Lepore SJ, Buzaglo JS, Lieberman MA, Golant M, Greener JR, Davey A. Comparing standard versus prosocial internet support groups for patients with breast cancer: A randomized controlled trial of the helper therapy principle. J Clin Oncol. 2014; 32: 4081–6.
Folkman S, Greer S. In the the face of serious illness: When theory, research, and practice inform each other. Psycho-Oncology. 2000; 9: 11–19.
Lazarus RS, Folkman S. Stress, Appraisal, and Coping . New York: Springer; 1984.
Stanton AL, Snider PR. Coping with breast cancer diagnosis: A prospective study. Health Psychology. 1993; 12: 16–23.
Stanton AL, Danoff-Burg S, Sworowski LA, et al. Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients. Journal of Clinical Oncology 2002; 20: 4160–8.
Allen SM, Shah AC, Nezu AM et al. A problem-solving approach to stress reduction among younger women with breast carcinoma: A randomized controlled trial. Cancer. 2002; 94: 3089–100.
Lee V, Robin Cohen S, Edgar L, et al. Meaning-making intervention during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Social Science & Medicine. 2006; 62: 3133–45.
Owen JE, Giese-Davis J, Cordova M, et al. Self-report and linguistic indicators of emotional expression in narratives as predictors of adjustment to cancer. Journal of Behavioral Medicine. 2006; 29: 335–45.
Austenfeld JL, Stanton AL. Coping through emotional approach: A new look at emotion, coping, and health-related outcomes. Journal of Personality. 2004; 72: 1335–63.
Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: Scale construction and validation. Journal of Personality & Social Psychology. 2000; 78: 1150–69.
Donovan KA, Grassi L, McGinty HL, Jacobsen PB. Validation of the distress thermometer worldwide: State of the science. Psycho-Oncology. 2014; 23: 241–50.
Vilela LD, Nicolau B, Mahmud S, Edgar L, Hier M, Black M et al. Comparison of psychosocial outcomes in head and neck cancer patients receiving a coping strategies intervention and control subjects receiving no intervention. J Otaolaryngol. 2006; 35: 88–96.
Watts S, Edgar L. Nucare, a coping skills training intervention for oncology patients and families: Participants’ motivations and expectations. Can Oncol Nurs J. 2004; 14: 84–95.
Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005; 103: 1494–1502.
Ransom S, Jacobsen PB, Booth-Jones M. Validation of the distress thermometer with bone marrow transplant patients. Psycho-Oncology. 2006; 15: 604–612.
Lambert MJ, Morton JJ, Hatfield D, et al. Administration and Scoring Manual for the Outcome Questionnaire-45. Orem, UT: American Professional Credentialing Services; 2004.
Vermeersch DA, Lambert MJ, Burlingame GM. Outcome questionnaire: Item sensitivity to change. J Pers Assess. 2000; 74: 242–61.
Baker F, Denniston M, Zabora J, Polland A, Dudley WN. A POMS short form for cancer patients: Psychometric and structural evaluation. Psycho-Oncology. 2002; 11: 273–281.
Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977; 3: 385–401.
Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). Journal of Psychosomatic Research. 1999; 46: 437–443.
Weiss D, Marmar C. The impact of event scale-revised. In: Wilson J, Keane T (eds). Assessing Psychological Trauma and PTSD. New York: Guildford; 1997.
Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks: Sage Publications; 1991.
Owen JE, Bantum EO, Criswell K, Bazzo J, Gorlick A, Stanton AL. Representativeness of two sampling procedures for an internet intervention targeting cancer-related distress: A comparison of convenience and registry samples. J Behav Med. 2014; 37: 630–41.
Duijts SF, Faber MM, Oldenburg HS, van Beurden M, Aaronson NK. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors: A meta-analysis. Psycho-Oncology. 2011; 20: 115–26.
Kangas M, Bovbjerg DH, Montgomery GH. Cancer-related fatigue: A systematic and meta-analytic review of non-pharmacologic therapies for cancer patients. Psych Bull. 2008; 134: 700–41.
McGarry S, Ward C, Garrod R, Marsden J. An exploratory study into the unmet supportive care needs of breast cancer patients. European Journal of Cancer Care. 2013; 22: 673–83.
Hall A, Campbell HS, Sanson-Fisher R, Lynagh M, D’Este C, Burkhalter R, Carey M. Unmet needs of Australian and Canadian haematological cancer survivors: A cross-sectional international comparative study. Psycho-Oncology. 2013; 22: 2032–8.
Hutchison SD, Steginga SK, Dunn J. The tiered model of psychosocial intervention in cancer: A community-based approach. Psycho-Oncology. 2006; 15: 541–6.
Titov N, Dear BF, Ali S, Zou JB, Lorian CN, Johnston L et al. Internet-delivered cognitive behavior therapy for older adults with symptoms of depression: A randomized controlled trial. Behav Therapy. 2015; 46: 193–2005.
Bantum EO, Albright CA, White KK, Berenberg JL, Layi G, Ritter PL, Laurent D, Plant K, Lorig K. Surviving and thriving with cancer using a web-based health behavior change intervention: Randomized controlled trial. J Med Internet Res. 2014; 16: e2.
Ben-Zeev D, Schueller SM, Begale M, Duffecy J, Kane JM, Mohr DC. Strategies for mHealth research: Lessons from 3 mobile intervention studies. Administration & Policy in Mental Health. 2015; 42: 157–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Jason E. Owen, Erin O’Carroll Bantum, Ian S. Pagano, and Annette Stanton declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Funding Source
NCI #1R03CA137391-01A1
Disclaimer
The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
About this article
Cite this article
Owen, J.E., O’Carroll Bantum, E., Pagano, I.S. et al. Randomized Trial of a Social Networking Intervention for Cancer-Related Distress. ann. behav. med. 51, 661–672 (2017). https://doi.org/10.1007/s12160-017-9890-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-017-9890-4