Abstract
Background
Research is yet to investigate whether psychological interventions delivered early after diagnosis can benefit patients with head and neck cancer (HNC).
Purpose
The aim of this study was to investigate the effectiveness of a brief self-regulatory intervention (targeting illness perceptions and coping) at improving HNC patient health-related quality of life (HRQL).
Methods
A pilot randomized controlled trial was conducted, in which 64 patients were assigned to receive three sessions with a health psychologist in addition to standard care or standard care alone. Participants completed questionnaires assessing HRQL, general distress, and illness perceptions at baseline and again 3 and 6 months later.
Results
Compared to the control group, patients who received the intervention had increased treatment control perceptions at 3 months (p = .01), and increased social quality of life at 6 months (p = .01). The intervention was particularly helpful for patients exhibiting distress at baseline.
Conclusion
A brief psychological intervention following HNC diagnosis can improve patient perceptions of treatment and social quality of life over time. Such interventions could be targeted to patients who are distressed in order to confer the greatest benefit.
Trial Registration Number
12614000813684.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with head and neck cancer (HNC) must contend with not only a significant threat to mortality but also highly distressing symptoms and treatment. Changes in the ability to breathe, speak, swallow, and eat are commonly associated with the disease [1], as well as pain and disfigurement that is difficult to conceal [2]. These factors have an enduring effect on patient health-related quality of life (HRQL) [3], and have led to the suggestion that HNC is the most emotionally traumatic cancer to experience [4]. Patients report particularly low HRQL during and immediately after treatment as they manage severe side effects that impact all aspects of wellbeing [5].
The implications of HNC for patient HRQL, and the variation in this outcome among individual patients [1], suggest that interventions to maximize HRQL following treatment are needed. While psychological interventions have proven effective at improving HRQL in patients with other cancer types [6], there is limited evidence for their utility in patients with HNC. The most common forms of intervention evaluated for this group are psychoeducation and cognitive behavioral therapy [7], although few randomized controlled trials have been conducted [8,9,10] and rates of participant drop out are high. A recent Cochrane review concluded that shortcomings in the design and reporting of studies testing psychological interventions for HNC patients prevent any conclusions regarding their effectiveness [11].
Psychological interventions based on Leventhal’s [12] self-regulatory or common sense model of illness may be beneficial for patients with HNC. The common sense model proposes that when individuals are faced with a health threat they form parallel cognitive and emotional representations. Both sets of representations interact to generate unique coping behaviors to manage the health threat and its associated emotions. Continuous appraisal of the outcomes of these behaviors is proposed to occur which can lead to the modification of initial representations [13]. Cognitive representations include perceptions of the consequences, duration (timeline), symptoms or label (identity), causes, and controllability of an illness [14]. Emotional representations describe the emotional impact of an illness. Recent measures have also included assessments of overall illness understanding or coherence [15, 16].
Evidence to support the common sense model has been found across a diverse range of patient groups [17], including patients with HNC [18]. For example, perceiving a long timeline and many consequences of the disease at diagnosis has predicted lower HRQL 2 years later [19]. Similarly, long timeline perceptions have predicted HNC patient depression 6–8 months post-treatment [20]. Dempster et al. [21] showed that changes in perceptions of esophageal cancer over time were associated with changes in patient depression and anxiety, particularly perceptions of personal and treatment control. There is preliminary research to suggest that illness perceptions may also contribute to psychological wellbeing among individuals caring for patients with HNC. These caregivers can experience high levels of distress [22], including anxiety [23] and post-traumatic stress disorder symptoms [24]. One study found that illness perceptions and coping strategies explained between 35 and 49% of the variance in depression and anxiety reported by caregivers of patients with esophageal cancer [25]. More recently, caregiver perceptions of low treatment control and a strong illness identity at HNC diagnosis predicted greater post-traumatic stress 6 months later [26]. Collectively, these findings suggest that illness perceptions could be targeted in psychological interventions that aim to improve psychological outcomes among HNC patients and their caregivers.
Self-regulatory interventions aim to change illness perceptions and coping through the provision of individualized information and coping techniques. Self-regulatory interventions have proven effective at improving a broad range of outcomes in other patient populations, including myocardial infarction patients and their spouses [27, 28], as well as patients with acute coronary syndromes, coronary heart disease, renal disease, and diabetes [29,30,31,32]. Research suggests that such interventions may be successfully applied in both patients and caregivers [28, 33].
Only one study to date has tested a self-regulatory intervention for patients with HNC. In this randomized controlled trial, 90 outpatients previously treated for oral and oral pharyngeal cancer were assigned to receive six weekly sessions delivered by a trained nurse specialist or usual care [34]. The aim of the intervention was to explore illness beliefs and behaviors and develop relaxation skills in order to reduce fear of cancer recurrence and anxiety. Although patients who received the intervention exhibited less fear of recurrence and anxious pre-occupation, these results were not sustained over time. A potential explanation is that adherence to the intervention was low, with only 14 of 53 patients attending all six sessions. While the results of this study are promising, further research is needed. The intervention was delivered between 7 and 11 months post-treatment, although there is evidence that HNC patients would appreciate psychological support at time of diagnosis and during treatment [35]. Given that large reductions in HRQL are typically observed across this time, interventions delivered here may be of greater benefit than those delivered later in the disease trajectory. Participant drop out and difficulties with adherence to the intervention and other psychological interventions for patients with HNC [36], also suggest that brief and flexibly timed interventions may be most appropriate for this group. Finally, studies are yet to investigate whether self-regulatory interventions can improve HNC patient HRQL, an outcome for which there remains considerable unexplained variation [1].
Efforts to improve HRQL among patients with HNC are of particular importance because of the long-term impact of the disease on physical, social, and psychological wellbeing, and well-established associations between HNC patient HRQL and clinical outcomes, including disease-specific and overall survival [37]. The primary aim of this study was to determine whether a brief self-regulatory intervention based on the common sense model could improve HRQL in patients with HNC. We hypothesized that patients randomly assigned to receive the intervention would demonstrate positive changes in illness perceptions, HRQL, and levels of distress, approximately 3 and 6 months after diagnosis in comparison to patients assigned to standard care. A secondary aim was to assess whether the intervention could also produce positive changes in caregiver illness perceptions and distress levels.
Methods
Design
A pilot randomized controlled trial was tested utilizing a parallel design. Patients were randomly allocated to receive the self-regulation intervention or to standard care based on a 1:1 allocation ratio. Randomization was performed by a researcher independent of the study using a randomization table generated by computer software. The randomization sequence was concealed in sealed envelopes until patients consented to participate, at which point group allocation was assigned. While the researchers and psychologist responsible for delivering the intervention were not blind to group allocation, all medical care providers were blind to condition assignment.
Participants
Participants were a consecutive sample of patients diagnosed with a primary epithelial head and neck cancer (carcinoma in the pharynx, larynx, oral cavity, sinonasal cavity), or metastatic skin cancer in the head and neck region, and their caregivers, attending a multidisciplinary head and neck clinic meeting at Auckland City Hospital between August 2014 and July 2015. Patients were required to have received a diagnosis within 3 weeks prior to their clinic attendance, as well as a treatment plan of one or more treatments (surgery, radiotherapy, chemotherapy). Only adult patients were included in the study, with those aged between 18 and 90 years of age eligible to participate. Exclusion criteria were conditions that would interfere with participation (including severe substance dependence, active psychosis, cognitive impairment, or significant physical disability). Non-English speaking patients were also excluded, as well as those to be treated with palliative intent. Eligible caregivers included those identified by the patient as a spouse, family member, or close friend.
Power Calculation
The previous self-regulation intervention trial found an effect size of d = 0.7 for reducing anxious pre-occupation in patients with HNC [33]. Setting power at 0.80 and alpha at .05, G-power software [38] indicated that a sample of 68 patients would be needed to detect a similar effect. However, we aimed to recruit a total sample of 100 patients to account for participant attrition.
Procedure
The study was registered with the Australian New Zealand Clinical Trials Registry and ethical approval was obtained from the Health and Disability Ethics Committee and the Auckland District Health Board Research Review Committee. Patients were screened for eligibility by both an HNC nurse specialist and an otorhinolaryngologist. Eligible patients were approached after meeting the multidisciplinary team and provided with an information sheet about the study. Patients were asked for their permission to be contacted in the next week regarding participation. Those who gave permission were contacted by phone at this time point by the first author and verbally consenting individuals were posted a written consent form and baseline questionnaire. They were then randomly allocated to the intervention or standard care condition. Patients in the intervention group were contacted within the next week to organize their session times with the registered health psychologist responsible for delivering the intervention.
All participants were asked to complete questionnaires at baseline and again 3 and 6 months post-diagnosis. These were sent by mail with a return free-postage envelope and assessed demographics, HRQL, distress, and illness perceptions. Postage questionnaires allowed patients to complete questionnaires in the absence of the researchers, who may have inadvertently influenced responding. Participants were contacted by the researchers in order to ensure that questionnaires were completed within 2 weeks of each assessment point. Medical information was obtained from patient medical records.
Standard Care
Patients diagnosed with HNC are required to attend a multidisciplinary clinic meeting at which a diverse range of specialists confer to identify the most appropriate treatment plan. Once this plan has been determined, consultants are available to discuss details of diagnosis and treatment with patients. Patients to be treated with surgery are provided information sheets specific to their surgical procedure that detail what the surgery will involve, approximate length of hospital stay, and whether a tracheostomy is needed. These patients also attend a pre-operation anesthetic review with a nurse, who provides further information relating to the planned procedure. Patients to be treated with radiotherapy are presented with an information booklet on the day of their multidisciplinary clinic meeting which describes the duration and side effects of this treatment. They are also invited to attend a welcome meeting at the radiotherapy department where they can receive general information from radiation oncologists and become familiar with the department and staff. If chemotherapy is required this is mentioned at the initial multidisciplinary meeting but is discussed in more detail at a subsequent chemotherapy orientation run by nurses. All patients receive a clinic letter documenting and explaining the decision to treat. Referrals to the Cancer Society (a non-government organization that endeavors to reduce the impact of cancer on individuals and the community) are made with patient permission on occasion. Patients also have the contact details of HNC nurse specialists who may be contacted regarding any concerns that arise from time of diagnosis through to the completion of treatment.
Intervention
The intervention consisted of three 60-min face-to-face sessions with a health psychologist. The timing of these sessions was flexible and organized around patient medical appointments and treatment. The first session was arranged to take place prior to treatment commencement, the second toward the beginning of treatment, and the third session toward the end of treatment. A 30-min follow-up phone call also took place approximately 3 weeks after the final session. Intervention sessions took place at hospital or at patients’ homes, depending on their personal preference.
The content of each intervention session was based on the common sense model [14]. Intervention participants completed a brief assessment of illness perceptions at the beginning of each session. Based on these assessments, individually tailored information about HNC was provided. Specifically, perceptions of consequences were addressed with information regarding the specific side effects associated with treatment (which may have been surgery, chemotherapy, radiotherapy, or a combination); perceptions of timeline were targeted with information regarding the likely duration of treatment and recovery and the associations these have with cancer stage; perceptions of personal control, concern, and emotional impact were addressed by describing and providing coping strategies to manage side effects of treatment, as well as strategies for the management of distress; treatment control perceptions were managed through the provision of information regarding how different treatment approaches are used to cure the disease; perceptions of illness identity were targeted with information regarding the specific symptoms associated with patient diagnosis; and coherence and causal perceptions were addressed with comprehensive information about HNC, including the types, causes, methods of diagnosis, stages, treatment, and likely side effects. This differed to the information provided to patients receiving standard care alone, which was not tailored to address existing perceptions.
The focus of the first intervention session was improving patient understanding of HNC and its treatment in order to encourage accurate and informed illness perceptions. This was largely achieved through the provision of information about the disease. The second session focused on the development of coping strategies that could be used to manage distress, symptoms of the disease, and treatment side effects. The psychologist and patient worked together to develop an action plan specifying when, where, how, and with whom coping strategies might be implemented. Coping strategies were targeted to an issue identified by the patient as problematic. For example, patients who identified stress as an issue were provided with relaxation techniques, patients experiencing distress were supported with cognitive restructuring, positive activity scheduling, and self-care techniques, and patients with challenging symptoms were provided with options for their management (e.g., techniques for the alleviation of a dry or sore mouth, difficulty swallowing, trouble speaking, and pain). Coping strategies were not discussed or developed among patients who received standard care. The final intervention session evaluated the effectiveness of coping strategies and prepared patients for what to expect following the completion of treatment. This session also addressed concerns about the future (including fear of cancer recurrence) and aimed to normalize these. In contrast, standard care did not include any discussion regarding common experiences post-treatment and how these might be addressed.
An educational manual of materials entitled “Head and Neck Cancer: A Guide for Patients and their Family Members” was developed as part of this study and provided to patients as a supplement to intervention sessions. This manual was divided into sections that included information on: head and neck cancer (types, causes, symptoms, and stages); treatment (surgery, chemotherapy, and radiotherapy); side effects; coping; managing relationships (with family members, children, friends, and health care professionals); and support available in the community. The information provided was more comprehensive than the material provided to patients receiving standard care. Standard care information addressed physical and practical considerations relevant to HNC, whereas the intervention manual also considered psychosocial aspects of the disease, providing specific suggestions regarding how these may be managed. Furthermore, the manual format allowed patients to access all information from a single source. This contrasts with standard care information which was distributed across several individual resources.
The health psychologist conducting sessions was required to engage in several practice sessions with individuals acting as patients prior to recruitment. Each practice session revolved around a unique HNC case (which was varied in relation to patient age, gender, cancer stage, and treatment type). Fidelity to intervention content was assessed by the first and second author who rated the extent to which the health psychologist successfully addressed issues relevant to each session. This included identifying and modifying inaccurate illness perceptions in session one, discussing coping and providing strategies for the management of distress and treatment side effects in session two, and assisting with patient concerns for the future in session three. Regular meetings were held over the course of the study between the researchers and the psychologist delivering the intervention.
Measures
The primary outcome was patient HRQL. Secondary outcomes were distress and illness perceptions.
Functional Assessment of Cancer Therapy—Head and Neck (FACT-H&N)
The FACT-H&N is a multi-dimensional questionnaire specifically designed to measure HRQL in patients with HNC [39]. There are four core subscales comprised of 27 items that index physical, social, emotional, and functional wellbeing. A supplementary scale consists of 12 items designed to assess head and neck specific wellbeing. The physical wellbeing subscale collects information related to patient experiences of symptoms (including fatigue, nausea, and treatment side effects) and whether these are limiting engagement in daily activities. The social subscale requires patients to rate their satisfaction with the support they receive from their family members and friends, as well as satisfaction with family communication about HNC, and feelings of closeness to others. The emotional subscale assesses patient feelings (such as sadness, worry, and hopelessness), the functional subscale assesses patient capacity to function across diverse settings (including work and home), and the head and neck specific subscale assesses the degree to which patients are impacted by the unique challenges of the disease, including eating, swallowing, breathing, and speech difficulties. Ratings on items for each domain are summed to form a total HRQL score, with higher scores indicative of better HRQL. The questionnaire has demonstrated validity, reliability, and sensitivity in HNC patient samples [39, 40]. Internal consistency was excellent in the present study, with α = .89 for total HRQL at baseline, α = .94 for total HRQL at 3 months, and α = .93 for total HRQL at 6 months.
General Health Questionnaire (GHQ-12)
The GHQ-12 is a brief, reliable, and sensitive measure for assessing symptoms of psychological distress [41]. Respondents are asked to rate the degree to which they agree with each item on a 4-point scale. The 12 items are summed to form a total score. Higher scores reflect higher distress, with scores greater than 15 indicating distress that is clinically significant. Reliability coefficients have been found to range from .78 to .95 in a number of studies [42] and the validity of the questionnaire is well established [41]. Alphas in the present study were .83, .90, and .90 at baseline, 3 months, and 6 months, respectively.
Brief Illness Perception Questionnaire (Brief IPQ)
The Brief IPQ is a nine item scale designed to efficiently measure individual perceptions of illness [15]. Each perception is assessed with one item rated on a 0–10 scale; five items assess cognitive representations (consequences, timeline, personal control, treatment control, and identity), two items assess emotional representations (concern and emotional impact), and one item assesses illness comprehensibility (coherence). The scale also includes an open-ended item where respondents are asked to rank the three most important causes of their illness. The Brief IPQ is widely used and has good psychometric properties [43].
Satisfaction with Intervention
Participants in the intervention group were asked to answer four open-ended questions. These questions aimed to assess general satisfaction with sessions received, aspects of the intervention that were considered most beneficial, aspects of the intervention that could be improved, and whether the intervention could be recommended to other patients diagnosed with HNC.
Data Analysis
Analyses were performed using SPSS version 22 software. Analysis of covariance was used to investigate differences in change scores between groups (for both primary and secondary outcomes) at 3 and 6 month follow-ups, while controlling for baseline scores. Comparisons were made between patients assigned to the intervention and patients assigned to the control group (intention to treat), as well as between patients who received the entire intervention and those who did not (per-protocol analyses). Analyses were performed when including cancer stage and radiotherapy treatment as covariates because of their potential relationship with patient HRQL. Subgroup analyses were also performed to investigate the effects of baseline distress on intervention effectiveness; only patients scoring >10 on the GHQ-12 were included. Although scores >15 are considered the cutoff for clinical distress, only 11 patients met this criteria at diagnosis. In contrast, 33 patients scored >10. This cutoff was close to the mean score on the measure at baseline (M = 11.98, SD = 4.38), which has been proposed as a rough guide to the optimum threshold [44]. For all tests, a two-sided p value less than .05 was considered statistically significant. Missing data was addressed using the method of pairwise deletion.
Results
One hundred and seventy patients were screened for eligibility (Fig. 1). Of these patients, 139 met eligibility criteria and 64 consented to take part, resulting in a 46% participation rate. No significant differences were found between eligible patients who declined participation and those who consented with respect to gender (p = .60), cancer stage (p = .61), and radiotherapy status (p = .32). However, a greater proportion of consenting patients received more than one treatment (44/62) compared to non-consenting patients (37/74), X 2 (1, 136) = 6.158, p = .01, and a greater proportion of patients who declined to participate died in the 12 months following their diagnosis (14/75) compared to those who consented (1/64), X 2 (1, 139) = 10.494, p < .01. No further data were available for comparison between these groups.
Following randomization, two patients were excluded due to further tests revealing non-cancerous tumors (subsequent to their multidisciplinary clinic visit and provision of consent). Of the 31 patients assigned to the intervention group, 27 completed all intervention sessions, representative of a 13% attrition rate. Two patients attended one intervention session only and two patients did not attend any sessions. Patient demographic and medical characteristics are presented in Table 1.
Seven patients in the intervention group had a caregiver participate compared to 11 patients in the control group. Six of the caregivers in the intervention group were spouses of the patient (86%) and one was a family member (14%). In the control group, six caregivers were spouses (55%), three were family members (27%), and two were friends (18%). Six of the seven caregivers in the intervention group participated in every intervention session with the patient, while one caregiver in this group participated in no intervention sessions. Results regarding caregiver outcomes are not presented due to insufficient power.
With respect to the timing of intervention sessions, session 1 occurred on average 35 days after the multidisciplinary clinic meeting (M = 35.34, Mdn = 32, SD = 17.24, range = 72), session two occurred on average 76 days after the meeting (M = 76.22, Mdn = 70, SD = 23.51, range = 98), and the final session occurred an average of 120 days after the meeting (M = 120, Mdn = 112, SD = 49.44, range = 232). When excluding one participant who had to delay the timing of intervention sessions due to unforeseen circumstances, the average number of days between the initial clinic meeting and session two (M = 73.66, Mdn = 69, SD = 19.74, range = 66) and session three was reduced (M = 112.65, Mdn = 112, SD = 33.43, range = 163). To provide a context for these time frames, standards of service provision require that patients referred with a high suspicion of HNC receive their first cancer treatment within 62 days. Patients with a confirmed diagnosis of HNC receive their first treatment or alternative management within 31 days of the decision to treat.
Regarding missing data, all patients completed every item on each assessment measure at baseline (n = 59), with the exception of one participant who missed the timeline item of the Brief IPQ. At 3-month follow-up, all patients completed every item on each assessment measure (n = 54), with the exception of one participant who again missed the timeline item, and one participant who did not complete the physical HRQL items of the FACT-H&N. At 6-month follow-up (n = 54), complete data were obtained from all patients, excluding one participant who missed the timeline item, and one participant who missed items on the HNC-specific HRQL subscale.
Illness Perceptions
When performing intention to treat analyses, no significant differences in illness perceptions were found between patients assigned to the intervention (n = 29) and patients assigned to the control group (n = 25), at 3- and 6-month follow-up. Table 2 presents the mean change in illness perceptions from baseline to 3 and 6 months for patients who received the intervention (n = 27) and those who did not (n = 27) (per-protocol analyses). There was a significant difference in perceptions of treatment control at 3 months; patients who received the intervention had a slight increase in their perceptions of treatment control, while patients who did not receive the intervention had a decrease in treatment control perceptions. Table 2 also presents the mean change in illness perceptions across time for patients distressed at baseline who received the intervention (n = 17) and patients who did not (n = 16) (sub group analyses). The significant difference in perceptions of treatment control continued to be observed between groups at 3 months. There was also a significant difference in perceptions of concern at this time point, with patients who received the intervention reporting a greater decrease in concern relative to those who did not. This is representative of a very large effect. No other significant differences in illness perceptions were found between groups.
Health-Related Quality of Life (HRQL)
Table 3 presents the mean change in HRQL from baseline to 3- and 6-month follow-up for patients in the intervention and control group, based on intention to treat analyses, per-protocol analyses, and subgroup analyses. When comparing patients assigned to the intervention (n = 29) and those assigned to the control group (n = 25), as well as patients who received the intervention (n = 27) with those who did not (n = 27), there was a significant difference in social HRQL at 6 months. Intervention participants had an increase in social HRQL from baseline to 6 months, while control participants had a decrease. This difference was also noted when comparing distressed patients who received the intervention (n = 17) with those who did not (n = 16). No other significant differences in HRQL were found between patients in the intervention and control group.
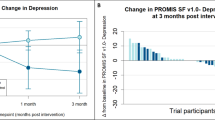
Distress
When comparing patients in the intervention and control group (using intention to treat, per-protocol analyses, and subgroup analyses), no significant differences in distress were found at 3- or 6-month follow-up.
Analyses on illness perceptions, HRQL, and distress were also performed when including gender and radiotherapy treatment as covariates due to significant differences between groups at baseline. This did not make a difference to the statistical significance of the results found.
Intervention Feedback
Twenty-five of 27 (93%) participants who completed open-ended questions about the intervention reported being satisfied with the sessions that they received; an example comment was, “Very satisfied. Just the right number of sessions during a trying time.” Aspects of the intervention that were considered most beneficial included discussing HNC (“Being able to talk about the issues of having cancer”) and treatment (“Getting one to talk about all aspects of treatment and feelings”), having someone to listen (“The positive reception and compassionate listening made the experience”), and learning coping strategies/stress reduction (“Thinking about coping strategies”, “Being stress free about my mortality”). The majority of patients suggested no changes to the intervention were necessary (75%), although one patient suggested that group sessions could be helpful, one patient would have liked more individual sessions, and two patients suggested that the intervention could be started earlier (“An earlier start as preparation for what is to follow”). Twenty five participants (93%) would recommend the intervention to others diagnosed with HNC.
Discussion
This is the first pilot randomized controlled trial to investigate the effectiveness of a brief psychological intervention targeting illness perceptions in newly-diagnosed patients with HNC. Results found that patients who received the intervention in addition to standard care had improved perceptions of treatment and social HRQL over time in comparison to patients who received standard care alone. Improvements in social HRQL continued to be observed when conducting intention to treat comparisons. These preliminary findings suggest that self-regulatory interventions based on the common sense model may have particular utility at improving social functioning following HNC diagnosis and treatment.
Further support for the intervention was found when restricting analyses to patients who exhibited distress at diagnosis. Distressed patients who received the intervention reported a decrease in perceptions of concern from baseline to 3 months, while perceptions of treatment control increased during this time. These participants also had a greater increase in social HRQL from baseline to 6 months compared to participants who received standard care alone. The importance of delivering psychological interventions to sufficiently distressed patients has been identified in the literature [7]. Not only does this increase power to detect intervention effects but also ensures that research findings are generalizable to clinical practice, where guidelines recommend psychological support specifically for patients experiencing heightened distress [45]. Other studies have found that after targeting psychological interventions to HNC patients experiencing distress, significant improvements in depression, anxiety, and post-traumatic stress [10], and smoking cessation [9] can be achieved. It is important to note that patients classified as distressed for the purpose of this study were experiencing a subclinical distress level. Therefore, the results may not be comparable to the results of other studies targeting patients with distress, and it is unclear whether the same benefits of the intervention would be observed among patients meeting clinical criteria. Nevertheless, there is evidence that treating subclinical distress can have positive implications in the long term, with psychological treatment of subclinical depression related to a reduced incidence of major depressive episodes 6 and 12 months later [46].
The self-regulatory intervention tested is the first to be provided at time of diagnosis and throughout treatment among patients with HNC. The low rates of participant drop out suggest that it is feasible to provide psychological support to patients during this time, particularly if the delivery of this support is flexible and coordinated around patient medical appointments and treatment side effects. Responses to open-ended questions regarding satisfaction with the intervention suggest that patients appreciated that the intervention was delivered soon after diagnosis, consistent with other research that HNC patients would like psychological support to manage this time [35]. Indeed, diagnosis and treatment are times at which patients with HNC report high levels of psychological distress (including depression and anxiety) [47], and reduced HRQL [1], suggesting that this may be the most beneficial time to intervene. Other studies have found that patients are dissatisfied with the amount of information they receive regarding the long-term impact of HNC and treatment [48] and that this can influence their subsequent experience of distress [49]. Therefore, psychological interventions provided early after diagnosis may be an effective way to provide information and prepare patients for what is ahead, with positive implications for psychological adjustment.
Providing psychological support early after diagnosis was found to benefit patient social HRQL in the present study. HRQL is a particularly important outcome in patients with HNC, for whom dry mouth, difficulty swallowing, speech difficulties, pain, and negative changes in appearance can be enduring problems following treatment [50]. Efforts to improve social HRQL among patients with HNC are essential considering that the social impact of the disease is of great importance to this population [51]. In a study of 62 patients surgically treated for laryngeal cancer, patients did not consider the permanent stoma and voice loss to be the most important contributors to their quality of life, but instead reported that work and family relationships were the domains with the poorest adjustment [51]. Furthermore, social functioning is an aspect of HRQL that is most negatively affected by HNC. Not only do common side effects such as facial disfigurement provoke a range of (frequently negative) reactions from others, but changes in patient self-esteem and sense of self can influence patient desire to engage in social interactions [52]. Other side effects, including difficulties with chewing, swallowing, and speaking, can make it very hard for patients to engage in regular social activities with their family and friends, and often negatively impact on communication. In fact, research has found that patients with HNC are at risk of social isolation and disrupted relationships given that the ability to eat and speak is what allows us to participate in a diverse range of social interactions [53]. Fortunately, social support can buffer the impact of HNC on overall HRQL; both HRQL and survival are better among patients who are married, those who do not live alone, and those who are employed [54]. Therefore, the improvements in social HRQL observed may have long-term benefits for overall health.
Our findings can be compared to those reported by other studies that have aimed to provide information and coping strategies to patients with HNC, although these have used less robust methods. In a study by Semple and colleagues [55], 54 successfully treated HNC patients screening positive for distress self-selected to participate in a problem-focused intervention or to usual care. Patients who received the intervention demonstrated improvements in depression and anxiety from baseline to 3 months, as well as improved social functioning and quality of life compared to patients in the usual care group. However, self-selection may have biased these results. Similarly, a non-randomized study found that a short-term psychoeducational coping strategies intervention improved physical and social functioning, global quality of life, fatigue, and depressive symptoms in HNC patients 1–36 months post-treatment [56]. The present study adds to the literature by using a randomized controlled design. It provides support for the ability of a psychological intervention to improve social HRQL in patients with HNC, although results for other outcomes were not as strong.
Overall HRQL and distress were not improved in patients who received the intervention, an unexpected finding. It may be that social HRQL is more amenable to change than overall HRQL which incorporates physical and head and neck specific functioning—these domains are likely to be strongly influenced by medical factors, including cancer stage, treatment type, and symptom severity. With respect to patients’ emotional experience of the disease, it is possible that the intervention was too brief to change or impact distress levels. It may also be that patients who were most distressed at the time of diagnosis (and who had the greatest room for improvement in depression and anxiety) were less likely to take part than other patients. Indeed, the participation rate of the present study was 46%, consistent with low rates of participation in other intervention studies involving patients with HNC [9, 36] and male cancer patients more generally [57]. Therefore, it is possible that a significant proportion of patients may not engage in an intervention involving sessions with a psychologist were it to be incorporated into clinical practice.
The rate of caregiver participation in the study was particularly low. This is likely because the majority of patients who volunteered were single. It may be that these patients perceived a greater need for psychological support than those who were already supported by a spouse. Nevertheless, caregivers who were assigned to the intervention group demonstrated good adherence to the sessions suggesting that they had a desire to be involved and to receive support. This is consistent with other findings demonstrating that caregivers of patients with HNC perceive a need for psychological assistance [58]. Despite the study being underpowered to examine caregiver outcomes, it is plausible that their inclusion in the intervention sessions may have contributed to positive changes in social HRQL among patients. Specifically, changes may reflect an increase in the similarity of patient and caregiver perceptions in response to the intervention, which has previously been related to better HNC patient HRQL [59].
Patient adherence to the intervention was high. This is worth highlighting given that a number of previous studies examining interventions for patients with HNC have had high rates of participant drop out, particularly those which have required participants to attend multiple sessions within a pre-specified time frame. These interventions may not benefit the majority of HNC patients because the burden of participation is too great. This is particularly so during treatment where survival is of primary concern among patients and their family members. The findings of this randomized controlled trial suggest that an intervention consisting of three face-to-face sessions with a health psychologist poses minimal patient burden. Furthermore, such a brief and relatively simple intervention may be practically incorporated into clinical practice, presenting an opportunity to improve HNC patient psychological outcomes.
While strengths of this study include the use of a randomized controlled design and high acceptability of the intervention among recipients, there are several important limitations to consider. First, no active control group was used. Therefore, it is difficult to determine whether improvements observed in patients who received the intervention are attributable to the content of the sessions or are instead a result of non-specific factors, such as the therapeutic relationship. Furthermore, the study was not restricted to patients experiencing distress. Consequently, a number of participants who were well-adjusted received the intervention, diluting power to detect significant effects. Statistical power was also limited by the small sample size overall in this pilot study. Based on a power calculation, the desired sample size was 68 patients, yet only 54 were included in the final analyses. As a result, it is possible that the results obtained may not reflect what would have been observed had the goal sample size been achieved. It is also difficult to determine whether the results would generalize to the wider HNC patient population. Differences between the intervention and control group were noted at baseline, however controlling for these variables did not change the statistical significance of the results. Although there was very little missing data, it is important to acknowledge that missing responses to questionnaire items may have altered the study findings. Additionally, investigations of the impact of the intervention on caregiver adjustment were not performed, due to the low rate of caregiver participation. Finally, the researchers were not blind to group condition which can result in biased estimates of treatment effects. However, questionnaires were completed in the absence of the researchers and the psychologist who delivered the intervention was not involved in data collection.
The results demonstrate that it is feasible to deliver a brief intervention to patients with HNC early after diagnosis and during treatment, and that this can improve patient perceptions of treatment control and concern (particularly among those who are distressed) and improve social HRQL. Larger replication studies targeted to patients experiencing high levels of distress at HNC diagnosis are needed.
References
Howren MB, Christensen AJ, Karnell LH, Funk GF. Psychological factors associated with head and neck cancer treatment and survivorship: Evidence and opportunities for behavioral medicine. J Consult Clin Psychol. 2013;81:299–317.
List MA, Bilir SP. Functional outcomes in head and neck cancer. Semin Radiat Oncol. 2004;14:178–189.
Mehanna HM, Morton, RP. Deterioration in quality-of-life of late (10-year) survivors of head and neck cancer. Clin Otolaryngol. 2006;31:204–211.
Bjorklund M, Sarvimaki A, Berg A. Living with head and neck cancer: A profile of captivity. J Nurs Healthc Chronic Illn. 2010;2:22–31.
Hammerlid E, Silander E, Hornestam L, Sullivan M. Health-related quality of life three years after diagnosis of head and neck cancer—a longitudinal study. Head Neck. 2001;23:113–125.
Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: Meta analysis of 37 published controlled outcome studies. Patient Educ Couns. 2003;50:179–186.
Luckett T, Britton B, Clover K, Rankin NM. Evidence for interventions to improve psychological outcomes in people with head and neck cancer: A systematic review of the literature. Support Care Cancer. 2011;19:871–881.
Katz MR, Irish JC, Devins GM. Development and pilot testing of a psychoeducational intervention for oral cancer patients. Psychooncology. 2004;13:642–653.
Duffy SA, Ronis DL, Valenstein, et al. A tailored smoking, alcohol, and depression intervention for head and neck cancer patients. Cancer Epidemiol Biomark Prev. 2006;15:2203–2208.
Kangas M, Milross C, Taylor A, Bryant RA. A pilot randomized controlled trial of a brief early intervention for reducing posttraumatic stress disorder, anxiety and depressive symptoms in newly diagnosed head and neck cancer patients. Psychoonology. 2013;22:1665–1673.
Semple C, Parahoo K, Norman A, McCaughan E, Humphris G, Mills M. Psychosocial interventions for patients with head and neck cancer. Cochrane Database Syst Rev. 2013;8:CD009441.
Leventhal H, Meyer D, Nerenz DR. The common sense representation of illness danger. In: Rachman S, ed. Contributions to Medical Psychology. Vol. 2. New York: Pergamon Press, 1980:17–30.
Wearden A, Peters S. Therapeutic techniques for interventions based on Leventhal’s common sense model. Br J Health Psychol. 2008;13:189–193.
Leventhal H, Nerenz DR, Steele DJ. Illness representation and coping with health threats. In: Baum A, Taylor SE, Singer JE, eds. Handbook of Psychology and Health. Hillsdale (NJ): Lawrence Erlbaum Associates, 1984:219–252.
Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–637.
Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron L, Buick D. The revised illness perception questionnaire (IPQ-R). Psychol Health. 2002;17:1–16.
Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health 2003;18:141–184.
Richardson AE, Morton R, Broadbent E. Caregivers’ illness perceptions contribute to quality of life in head and neck cancer patients at diagnosis. J Psychosoc Oncol. 2015;33:414–432.
Scharloo M, Baatenbur de Jong RJ, Langeveld TP, van Velzen-Verkaik E, Doorn-op den Akker MM, Kaptein AA. Illness cognitions in head and neck squamous cell carcinoma: Predicting quality of life outcome. Support Care Cancer. 2010;18:1137–1145.
Llewellyn CD, McGurk M, Weinman J. Illness and treatment beliefs in head and neck cancer: Is Leventhal’s common sense model a useful framework for determining changes in outcomes over time? J Psychosom Res. 2007;63:17–26.
Dempster M, McCorry NK, Brennan E, Donnelly M, Murray LJ, Johnston BT. Do changes in illness perceptions predict changes in psychological distress among oesophageal cancer survivors? J Health Psychol. 2011;16:500–509.
Longacre ML, Ridge JA, Burtness BA, Galloway TJ, Fang CY. Psychological functioning of caregivers for head and neck cancer patients. Oral Oncol. 2012;48:18–25.
Hodges LJ, Humphris GM. Fear of recurrence and psychological distress in head and neck cancer patients and their carers. Psychooncology. 2009;18:841–848.
Posluszny DM, Dougall AL, Johnson JT, et al. Posttraumatic stress disorder symptoms in newly diagnosed patients with head and neck cancer and their partners. Head Neck. 2015;37:1282–1289.
Dempster M, McCorry NK, Brennan E, Donnelly M, Murray LJ, Johnston BT. Psychological distress among family carers of oesophageal cancer survivors: The role of illness cognitions and coping. Psychooncology. 2011;20:698–705.
Richardson AE, Morton RP, Broadbent EA. Illness perceptions and coping predict post-traumatic stress in caregivers of patients with head and neck cancer. Support Care Cancer. 2016;24:4443–4450.
Petrie KJ, Cameron LD, Ellis CJ, Buick D, Weinman J. Changing illness perceptions after myocardial infarction: An early intervention randomized controlled trial. Psychosom Med. 2002;64:580–586.
Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Further development of an illness perception intervention for myocardial infarction patients: A randomized controlled trial. J Psychosom Res. 2009;67:17–23.
Cossette S, Frasure-Smith N, Dupuis J, Juneau M, Guertin M. Randomized controlled trial of tailored nursing interventions to improve cardiac rehabilitation enrollment. Nurs Res. 2012;61:111–120.
Goulding L, Furze G, Birks Y. Randomized controlled trials of interventions to change maladaptive illness beliefs in people with coronary heart disease: Systematic review. J Adv Nurs. 2010;66:946–961.
Karamandiou C, Weinman J, Horne R. Improving haemodialysis patients understanding of phosphate-binding medication: A pilot study of a psycho-educational intervention designed to change patients perceptions of the problem and treatment. Br J Health Psychol. 2008;31:205–214.
Keogh KM, Smith SM, White P, et al. Psychological family intervention for poorly controlled type 2 diabetes. Am J Manag Care. 2011;17:105–113.
Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Can an illness perception intervention reduce illness anxiety in spouses of myocardial infarction patients? A randomized controlled trial. J Psychosom Res. 2009;67:11–15.
Humphris GM, Rogers SN. AFTER and beyond: Cancer recurrence fears and a test of an intervention in oropharyngeal patients. Soc Sci Dent. 2012;2:29–38.
Richardson AE, Morton R, Broadbent E. Psychological support needs of patients with head and neck cancer and their caregivers: A qualitative study. Psychol Health. 2015;30:1288–1305.
Ostroff J, Ross S, Steinglass P, Ronis-Tobin V, Singh B. Interest and barriers to participation in multiple family groups among head and neck cancer survivors and their primary family caregivers. Fam Process. 2004;43:195–208.
van Nieuwenhuizen AJ, Buffart LM, Brug J, Leemans CR, Verdonck-de Leeuw IM. The association between health related quality of life and survival in patients with head and neck cancer: A systematic review. Oral Oncol. 2015;51:1–11.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191.
Cella DF, Tulsky DS, Gray G, et al. The functional assessment of cancer therapy scale: Development and validation of the general measure. J Clin Oncol. 1993;11:570–579.
List MA, D’Antonio LL, Cella DF, et al. The performance status scale for head and neck cancer patients and the functional assessment of cancer therapy-head and neck (FACT-H&N) scale: A study of utility and validity. Cancer. 1996;77:2294–2301.
Goldberg D. General Health Questionnaire (GHQ-12). Windsor: NFER-Nelson, 1992.
Jackson C. The general health questionnaire. Occup Med. 2007;57:79.
Broadbent E, Wilkes C, Koschwanez H, Weinman J, Norton S, Petrie KJ. A systematic review and meta-analysis of the brief illness perception questionnaire. Psychol Health. 2015;30:1361–1385.
Goldberg DP, Oldehinkel T, Ormel J. Why GHQ threshold varies from one place to another. Psychol Med. 1998;28:915–921.
National Comprehensive Cancer Network. NCCN practice guidelines for the management of psychosocial distress. Oncology. 1999;13:113–147.
Cuijpers P, Koole SL, van Dijke A, Roca M, Li J, Reynolds CF. Psychotherapy for subclinical depression: Meta-analysis. Br J Psychiatry. 2014;205:268–274.
Haisfield-Wolfe ME, McGuire DB, Soeken K, Geiger-Brown J, de Forge BR. Prevalence and correlates of depression among patients with head and neck cancer: A systematic review of implications for research. Oncol Nurs Forum. 2009;36:E107–125.
Ziegler L, Newell R, Stafford N, Lewin R. A literature review of head and neck cancer patients information needs, experiences and views regarding decision-making. Eur J Cancer Care. 2004;13:119–126.
Llewellyn CD, McGurk M, Weinman J. How satisfied are head and neck cancer (HNC) patients with the information they receive pre-treatment? Results from the satisfaction with cancer information profile (SCIP). Oral Oncol. 2006;42:726–734.
Abendstein H, Nordgren M, Boysen M, et al. Quality of life and head and neck cancer: A 5 year prospective study. Laryngoscope. 2005;115:2183–2192.
Ramirez MJ, Ferriol EE, Domenech FG, Llatas MC, Suarez-Varela MM, Martinez RL. Psychosocial adjustment in patients surgically treated for laryngeal cancer. Otolaryngol Head Neck Surg. 2003;129:92–97.
Callahan C. Facial disfigurement and sense of self in head and neck cancer. Soc Work Health Care. 2004;40:73–87.
Gamba A, Romano M, Grosso IM, et al. Psychosocial adjustment of patients surgically treated for head and neck cancer. Head Neck. 1992;14:218–223.
Babin E, Sigston E, Hitier M, Dehesdin D, Marie JP, Choussy O. Quality of life in head and neck cancers patients: Predictive factors, functional and psychosocial outcome. Eur Arch Otorhinolaryngol. 2008;265:265–270.
Semple CJ, Dunwoody L, Kernohan WG, McCaughan E. Development and evaluation of a problem-focused psychosocial intervention for patients with head and neck cancer. Support Care Cancer. 2009;17:379–388.
Allison PJ, Edgar L, Nicolau B, Archer J, Black M, Hier M. Results of a feasibility study for a psycho-educational intervention in head and neck cancer. Psychooncology. 2004;13:482–485.
Berglund G, Petersson LM, Eriksson KC, et al. “Between Men”: A psychosocial rehabilitation programme for men with prostate cancer. Acta Oncol. 2007;46:83–89.
Baghi M, Wagenblast J, Hambek M, et al. Demands on caring relatives of head and neck cancer patients. Laryngoscope. 2007;117:712–716.
Richardson AE, Morton RP, Broadbent EA. Changes over time in head and neck cancer patients’ and caregivers’ illness perceptions and relationships with quality of life. Psychol Health. 2016;31:1203–1219.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study was funded by grants from the Oakley Mental Health Research Foundation (project 3705915) and the Maurice and Phyllis Paykel Trust (project 3706007).
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards
Authors Richardson, Tennant, Morton and Broadbent declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
About this article
Cite this article
Richardson, A.E., Tennant, G., Morton, R.P. et al. A Self-Regulatory Intervention for Patients with Head and Neck Cancer: Pilot Randomized Trial. ann. behav. med. 51, 629–641 (2017). https://doi.org/10.1007/s12160-017-9885-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-017-9885-1