Abstract
Objective
Radical cystectomy with permanent urinary diversion is the gold standard treatment for invasive muscle bladder cancer. Hydronephrosis is common in these patients, but Ultrasound (US) or Computed Tomography Urography (CTU) scan are unable to discriminate obstructive from non-obstructive hydronephrosis. We used Diuresis Renography (DR) with F + 10 in seated position (sp) method in the identification of patients with a Uretero-ileal Anastomosis Stricture (UAS) who would benefit from surgical therapy.
Methods
We studied 39 asymptomatic patients, who underwent radical cystectomy and urinary diversion. Based on radiological findings (US, CTU) 44 kidneys were hydronephrotic. All patients underwent a 99mTc-MAG3 DR with F + 10(sp) method. We acquired a DR for 20 min with the patient in a seated position. Patient drank 400–500 mL of water at 5 min after tracer injection and received a 20 mg bolus of Furosemide at 10 min during dynamic acquisition. The indices Time to peak, diuretic half time, and 20 min/peak ratio have been evaluated. Retrograde pyelography confirmed UAS in all patients with DR obstructive findings. We repeated DR as follow-up in two subgroups of patients.
Results
DR with F + 10(sp) method showed obstructive findings in 36 out of 44 hydronephrotic kidneys. 6 patients showed non-obstructive findings. 32 patients showed obstructive findings (20 out of 32 developed UAS within 12 months after surgery). Fifteen pts underwent a surgical treatment of UAS. In 1 patient with equivocal findings, we observed an ileo-ureteral reflux.
Conclusions
The DR with F + 10(sp) method in the seated position has a lower uncertain diagnostic rate, compared to the radiological findings of US or CTU, in management of bladder cancer patients with urinary diversion. The semiquantitative indices diuretic half time and 20 min/peak ratio evaluated in a condition of favorable gravity reduce uncertain responses improving interobserver concordance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radical Cystectomy (RC) and subsequent Urinary Diversion (UD) is the gold standard treatment for muscle invasive and high-risk non-invasive Bladder Cancer (BC) [1]. After the demolitive surgery, urological reconstructive techniques are implemented to restore urinary continuity and provide an acceptable quality of life. UD includes several types of surgical procedures including continent or incontinent reservoirs and orthotopic or heterotopic derivations, involving several different techniques to reroute the normal flow of urine. These techniques include Bricker ileal conduit, orthotopic neobladder, and pouches. All kinds of diversions require the anastomosis of the ureter to a selected intestinal segment [2,3,4,5,6]. These procedures can be affected by surgical complications related to the bowel, conduit, reservoir, stoma, or Uretero-Ileal Anastomosis Stenosis (UAS) [7]. UAS represents the most common complication requiring reoperation after radical cystectomy [8]. UAS is usually asymptomatic and develops gradually, leading to an increase in pressure upstream to the anastomosis on the kidney, hydronephrosis, and progressive damage of renal function including loss of kidney unit and chronic renal failure. Hydronephrosis, or the dilation of the renal pelvis and calyces, is very frequent and can be seen by traditional radiological studies (such as ultrasonography, computed tomography urography, and/or magnetic resonance imaging) secondarily to UAS (obstructive hydronephrosis) as well as in the absence of stenosis as a direct effect of surgical reconfiguration or pre-existent conditions (non-obstructive hydronephrosis) [9]. Hydronephrosis is considered an indirect radiological sign of UAS. Unfortunately, traditional radiological studies, with or without contrast media, are unable to differentiate obstructive from non-obstructive hydronephrosis [10]. However, the European Association of Urology guidelines on Bladder Cancer (BC) recommend only periodical laboratory and clinical investigations and only morphological cross-sectional imaging, often not executable for renal impairment [11].
If hydronephrosis is significant and obstruction is suspected, a nuclear imaging study such as a 99mTc-mercaptoacetyltriglicine (MAG3) scan is warranted. In these patients, traditional Diuresis Renography (DR) executed in the supine position, may give false positive or inconclusive responses. Currently, there is no widely accepted medical treatment for UAS although several procedures with potentially high surgical risks may be performed. At this time, more reliable methods for the diagnosis and management of urinary diversion are required to provide conservative and/or surgical treatments according to the patient’s needs. We propose, in our experience, the use of 99mTc-MAG3 Gravity-Assisted DR with F + 10(sp) method in a seated position [12] for the diagnosis of obstruction and monitoring urine drainage in patients with urinary diversion.
Materials and methods
Since June 2012, we studied 39 asymptomatic patients, 10 females/29 males, mean age of 69 years (range 48–81 years), who underwent RC and UD in a single center. The UD with an ileal conduit in 26 pts (Bricker trans-ileal ureterocutaneostomy), and ileal neobladder in 13 pts (Vescica Ileale Padovana technique). All pts involved in this study had US or CTU evidence of hydronephrosis and/or impairment of renal functional parameters. Based on radiological findings (US, CTU), 34 out of 39 pts had unilateral hydronephrosis, while 5 out of 39 pts had bilateral hydronephrosis (grade 2–3) at enrolment in this study. All 39 pts underwent to 99mTc-MAG3 DR with F + 10(sp) method. The patients were in a normal state of physiological hydration (non-fasting) and without diuretics or angiotensin-converting-enzyme inhibitors for 48 h prior to DR. We asked the pts to empty their bladder and we measured their blood pressure before starting the exam. If the systolic blood pressure was lower than 110 mm Hg, we asked the patient to eat a small meal before initiating.
In persistent hypotension status, blood pressure can be monitored throughout the test.
Only if strictly necessary, some minute following furosemide injection, an ice pack might be applied to the hand preventing a possible hypotension.
We acquired a DR using a dual-detector system with rectangular large view (Infinia-Xeleris III; GE Healthcare, Milwaukee), with a single head flexibility, allowing scan in all positions (seated, supine, upright, etc.). We used a gamma camera with a low-energy general-purpose collimator and selected the photopeak at 140 keV ± 10% energy window. We placed a detector in the vertical position with a tilt of 90°. We examined the patient in a seated position (sp), immobilized the shoulders, pelvis, and aligned the back facing the detector during dynamic acquisition. The arms were supported to prevent any movement. The field of view included the kidneys, heart, and bladder in the posterior view. We minimized the distance between the detector and the back of the patient to improve resolution and reduce scatter. After insertion of an intravenous catheter with an injection valve, we administered IV a dose of 150–200 MBq, volume 0.2–0.3 mL of 99mTc-MAG3 at time 0' followed by an injection of few milliliters of normal saline solution. We acquired a dynamic phase, with a frame rate of 2 s/frame for the first 60 frames, and 10 s/frame for 108 frames, using a 128 × 128 matrix, and zoom 1. At the 5th minute following tracer injection, the patient drank 400–500 mL of water. At the 10th minute during dynamic acquisition, we injected a bolus of 20 mg IV Furosemide. At the end of the dynamic acquisition, we acquired a series of late static images (preset time 60″, 256 × 256, zoom 1.0) at 20ʹ and 60ʹ before and after voiding, in both seated and supine position.
According to previously published works [12, 13] we evaluated the Renograms measuring the following semiquantitative indices of the renographic curves:
-
Split renal function %: based on the comparison of 1st–2nd minute background-corrected renal activity (normal value: 50 ± 10%). If split renal function was < 10%, the other indices of renal function were considered unreliable.
-
Time to peak (or Tmax): the time required to reach maximal activity on the renogram (normal value: 2–7 min).
-
Diuretic T1/2: the time elapsed between the administration of the diuretic (20 mg of Furosemide at 10th minute) and the half-time (normal value < 8 min).
-
20 min/peak ratio: the ratio between the average activity of the curves at 19–20 min and the peak activity (normal value < 0.25).
We used 99mTc-MAG3 with a modified Schlegel method not requiring blood sampling for determining the Effective Renal Plasma Flow (ERPF) for each kidney. It uses the renal counts 1–2 min after tracer injection and applies background subtraction as a ratio to the total amount of radioactivity injected intravenously with appropriate correction for kidney depth.
Two independent observers performed semiquantitative and qualitative evaluations of the dynamic data and post-voiding late static images in both seated and supine position. Differently from other invasive diagnostic approaches, DR does not require urinary catheterization and/or antibiotics following the procedure. In the kidneys with hydronephrosis and severe impaired function, a percutaneous nephrostomy tube was positioned before DR to preserve renal function. If present, the percutaneous nephrostomy was clamped during the dynamic phase of Renography.
A cine of raw data dynamic image with two locators is displayed, for assessing patient motion.
If no motion correction is required, the protocol is customized for automatic processing (GE,
Xeleris III).
We defined as a non-obstructive hydronephrosis a kidney with 20 min/Peak ratio < 0.25, and diuretic T1/2 < 8 min. The diagnostic work-up in pts with stenosis involved performing a retrograde cystography or a loop-graphy to exclude ileo-ureteral reflux. 6 out of 39 pts with non-obstructive findings repeated DR after a mean period of 12 months as follow-up.
A subgroup of 16 pts (15 pts who received surgical treatment for UAS and 1 pt with equivocal findings) repeated DR for three times, after a mean period of 12 and 22 months, to monitor open ureteral reimplantation for UAS. Overall, clinical mean follow-up was 30 months (range 17–70 months) (Table 1).
The DR with F + 10(sp) method is suggested by Italian Association of Nuclear Medicine in adult patients with suspected obstructive renal pathology [14]. This retrospective single-center study was approved by our institution’s review board. It followed the ethical guidelines of the Declaration of Helsinki and the written informed consent was waived. The authors (GT1, NF, SMR, and FPI) had access to the study data. No author has any conflict of interest to declare in relation to this study.
Results
We studied 39 BC pts, (10 females/29 males) with urinary diversion and radiologically detected hydronephrosis (Table 1). At enrolment, 34 out of 39 pts showed unilateral hydronephrosis, and 5 out of 39 pts showed bilateral hydronephrosis (grade 2–3). Based on radiological findings (US, CTU) we suspected 44 Kidneys to be obstructed (Table 2). All pts with suspected UAS underwent a baseline DR with 99mTc-MAG3 using F + 10(sp) method. All pts completed the test without requiring bladder catheterization. In pts with renal functional impairment, we placed a percutaneous nephrostomy followed by a retrograde pyelography prior to any surgical management. If present, the nephrostomy was clamped during the dynamic phase to evaluate the urine drainage in baseline condition.
We did not observe side effects as full bladder, disruption because of voiding or diuretic-induced hypotension.
The scintigraphy showed 68 detectable kidneys (split renal function > 10%) in 39 pts.
(3 kidneys had been removed for disease before test, whereas 7 kidneys were hydronephrotic with a severe impaired function and we positioned a percutaneous nephrostomy before DR to try to preserve renal function).
The baseline DR showed: normal, or Non-obstructive findings in 31 kidneys, equivocal findings in 1 kidney, and obstructive findings in 36 kidneys (Table 3). Retrograde pyelography confirmed DR diagnosis of UAS in 36 out of 44 Kidneys suspected as obstructed by US or CTU. Regarding the treatment of UAS, we performed 16 open ureteral reimplantation in 15 pts with good split renal function, confirmed by DR. Conversely, 10 pts underwent nephroureterectomy for significant impairment of renal function (split renal function < 10%); 3 pts with UAS refused surgery and were treated with pneumatic dilation of the stenosis; 1 pt was judged to be inoperable, due to significant co-morbidities and maintained the nephrostomy tube, and 3 pts died during follow-up. 1 patient with uncertain findings (due to a disagreement between two independent observers) had a partial ileo-ureteral reflux as confirmed by retrograde pielography. In the subgroup of 6 pts with non-obstructive hydronephrosis, we repeated DR after a mean period of 12 months (range 6–15 m) and did no observe significant changes (Table 4).
In the subgroup of 16 pts, including 15 pts with ureteral reimplantation (1 pt bilaterally) and 1 pt with equivocal findings, we performed DR three times as follow-up after a median period of 12 and 22 months. We observed a progressive reduction in number of detectable kidneys (− 4 left kidneys, and − 1 right kidney), due to restenosis (Table 5).
Regarding the time of onset of UAS, we observed about 60% of UAS in first year after surgery (Table 6). Almost perfect agreement was observed between two independent observers. The % of agreement was: 98.5% and Cohen’s k: 0.97. Sensitivity, specificity, disease prevalence, positive and negative predictive value as well as accuracy are expressed as percentages in Table 7. A p value of < 0.05 was considered statistically significant.
Discussion
Radiological exams rely on the presence of hydronephrosis to diagnose UAS. Hydronephrosis is defined as the dilation of the renal pelvis and calyces with urine. It is a secondary condition that typically occurs when the urine collecting system swells due to an impaired urinary drainage with a progressive increase in hydrostatic pressure and glomerular damage. It can be physiologic or pathologic, acute, or chronic, unilateral, or bilateral. Preoperative hydronephrosis is a common finding in BC points. In addition, the overall degree of hydronephrosis increases significantly in first year following surgery, regardless of the outcome of the intervention [9].
Several risk factors have been reported in pts with urinary diversion [1,2,3,4]. UAS is the main risk factor associated with renal function decline [2,3,4,5,6,7,8,9]. The etiopathology is related to many factors, such as inflammatory, ischemia, previous radiotherapy, diabetes,
vasculopathy, etc.). UAS may occur gradually, and many pts do not develop any symptom. The suspect of UAS is generally occasional and may occur during a follow-up visit (radiological evidence of hydronephrosis). The incidence of UAS is between 2.7 and 14% of cases depending on the series [10,11,12,13,14,15,16,17,18]. UAS rate may be influenced by the duration and the systematicity of follow-up regimens with the non-standardized use of specific upper urinary tract imaging.
Standardized oncological follow-up recommend the execution of abdominal CT with contrast media and blood tests 6 months following radical cystectomy and urinary diversion. In pts who underwent urinary diversion, hydronephrosis was extremely frequent also in the absence of stenosis [19].
The creatinine value is not suitable to diagnose unilateral UAS, because the level depends on global function of each patient. The patients with unilateral UAS are asymptomatic and present normal serum creatinine levels if their contralateral kidneys are preserved intact.
Unfortunately, traditional non-invasive radiological studies (US, CTU, MRI), with or without contrast media, are not able to discriminate obstructive from non-obstructive hydronephrosis and are less reliable for diagnosing UAS and monitoring surgical treatments. When a patient with urinary diversion is studied in the supine position, an inadequate pressure gradient in the urinary system may cause a delayed urine drainage and dilation of the renal pelvis due to a modified anatomy, reduced tonicity of normal tissues and unfavorable gravity effect. As confirmed by a recent article describing the development of Upright Computed Tomography for whole-body scans, the seated position is most useful, because it favors gravity and its effect on the volume and shape of the organ according to the body’s position [20].
Traditionally, DR was performed with pts in the supine position. The diagnosis was based on the findings of visual analysis of the renogram curve patterns. The supine position negatively influences the urine drainage and, especially in pts with a history of surgical management, may lead to false positive or uncertain DR findings [21]. Experts suggested several timings of Furosemide administrations (F − 15, F0, F + 2, F + 20). In all cases, the diagnosis based only on renogram pattern visual analysis may be inconclusive or subjective. To improve diagnosis, some authors suggested to calculate the Normalized Residual Activity (NORA) at the end of dynamic phase, after voiding and changing position [22,23,24]. Nevertheless, the interobserver concordance remained poor due to several timings in use, as confirmed by a multicenter survey. In a large collaborative study, regarding the inter-observer reproducibility in reporting on renal drainage in children with hydronephrosis, Tondeur et al. noted an important bias among the observers, resulting in rather poor inter-observer reproducibility. [25] The causes of discrepancy were the fact of including or neglecting the effect of micturition and change of patient's position, and the absence of a clear limit between partial and good drainage.
In 2009, a Technologist’s guide by EANM suggested the DR with F + 10(sp) as the preferred method in diagnosing an obstructive renal pathology. This guide underlined in all cases the importance of a scan in the orthostatic position at the end of DR because of the hydrostatic pressure and more realistic outcomes [26].
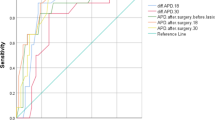
In 2013, the results of a comparison between DR with F + 10(sp) in the seated position vs. DR with F-15 in the supine position, applied consecutively in 7 days, were described in a group of pts with a suspected obstructive nephropathy. This paper demonstrated the many advantages of a test performed in the seated position [12]. The evaluation of renograms is based on the measure of semiquantitative indices, such as split renal function, time to peak, diuretic T1/2, and 20 min/peak ratio, rather than the visual analysis of renogram curve (Fig. 1). These indices, when performed in gravity favorable conditions, provide an objective measurement of renal function and urinary drainage, obtaining a reduction of uncertain responses and improving the interobserver agreement. Thanks to an optimal timing with an appropriate oral water intake (400 m) at 5th minute, and a reduced dose of Furosemide (20 mg, instead of 40 mg) at 10th minute during dynamic acquisition, the F + 10(sp) method obtained a higher diagnostic accuracy and a remarkable reduction of side effects, such as diuretic-induced hypotension and bladder fullness related problems, thus increasing patient compliance [27, 28].
In 2018, the F + 10(sp) method was included in Society of Nuclear Medicine and Molecular Imaging (SNMMI) Procedure Standard/European Association of Nuclear.
Medicine (EANM) Practice Guideline for Diuretic Renal Scintigraphy in Adults with a Suspected Upper Urinary Tract Obstruction v 1.0 [29]. The test has the potential to define urinary drainage more properly in gravity favorable conditions, improve accuracy and reduce side effects. For these reasons, we propose gravity-assisted DR for the monitoring of adult pts who underwent to surgical treatment of urinary tract.
In our experience, the semiquantitative indices, diuretic T1/2 and 20 min/peak ratio, demonstrated a high specificity in revealing UAS, as confirmed by a subsequent retrograde pyelography. The diuretic T1/2 and 20 min/Peak ratio of the left kidney seems to be slightly higher than the right kidney. In general, the performance of right kidney appears to be better than left (Table 2). As confirmed by other Authors, the distal portion of the left ureter is most likely at a higher risk for strictures due to its angulation [30].
The surgical management of the urinary tract (transposition of the left ureter, presence of an ileal conduit or orthotopic neobladder, may alter the normal anatomy and physiology, making the seated position essential during the exam to guarantee a regular urinary outflow. UAS is often clinically silent. An early UAS or unilateral damage may not substantially change the serum creatinine level. However, a slight increase in serum creatinine can be seen in the para-physiological reabsorption of urine from the intestinal segments used as reservoir. Early diagnosis and prompt treatment are required to prevent renal parenchymal loss and infection. Time of onset and the time to diagnosis of strictures may affect the therapeutic options for the sepoints. Considering the high rate of early UAS (< 6 months) and the functional limitations of traditional radiological imaging, it may be useful to perform DR during the first months following surgery.
DR with 99mTc-MAG3 avoids iodine or gadolinium-based agent contrast risks on the renal impaired population [31]. It is also well tolerated in pts with high serum creatinine levels and limits the need of invasive techniques. DR does not require urinary catheterization and antibiotics following procedure, thus avoiding the overuse of antibiotics in points at risk of developing antimicrobial resistance. Regarding the management of the ureteral stenosis, according to literature, we preferred an open approach with ureteral reimplantation when feasible due to the poor long-term results of endoscopic management [32,33,34].
Preoperative patient information, patient selection, surgical techniques, and careful post-operative follow-up are the cornerstones to achieve good long-term results in BC pts with UD. DR provides a more reliable discrimination of upper urinary tract obstruction adding basic information to conventional studies (US, CTU, Rx pyelography), improving diagnosis and providing functional and dynamic results. Thanks to gravity’s effect, the seated position may allow for a more accurate discrimination between obstructive and non-obstructive hydronephrosis.
The semiquantitative indices, such as diuretic T1/2, 20 min/peak ratio, offer an objective evaluation of urine drainage and improve interobserver concordance [35]. A better timing and reduction in Furosemide dosage (20 mg) avoid side effects and increase patient compliance. Moreover, the seated position allows to highlight a possible renal ptosis [36].
Conclusion
An earlier diagnosis of UAS is essential to avoid further renal impairment and other serious complications, especially in the first few months following RC, when only oncological follow-ups are usually scheduled. In patients with urinary diversion, the imaging performed in supine position is insufficient to correctly evaluate urine drainage. On the other hand, DR carefully selects candidates for surgery, avoiding unnecessary treatment in the subgroup of non-obstructed hydronephrosis. In BC pts the capacity of neobladder may be reduced. Using F + 10(sp) method, a lower dose of Furosemide (20 mg) and a shorter interval between diuretic administration (10 min) and the end of dynamic phase (20 min) improved patient compliance avoiding full bladder related problems, without need of bladder catheterization. The evaluation of semiquantitative indices diuretic half time and 20 min/peak ratio measured in a condition of favorable gravity may reduce uncertain responses due to supine position, improving interobserver concordance.
References
Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001;19(3):666–75. https://doi.org/10.1200/JCO.2001.19.3.666.
Gerharz EW, Hautmann RE, Abol-Enein H, Hafez K, et al. Urinary diversion. Urology. 2008;72(1):231–2.
Bricker EM. Bladder substitution after pelvic evisceration 1950. J Urol. 2002;167:1140–6.
Gore JL, Saigal CS, Hanley JM, Schonlau M, Litwin MS. Urologic diseases in America project variations in reconstruction after radical cystectomy. Cancer. 2006;107(4):729–37.
Lee RK, Abol-Enein H, Artibani W, Bochner B, Dalbagni G, Daneshmand S, et al. Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int. 2014;113(1):11–23. https://doi.org/10.1111/bju.12121.
Hautmann RE, Abol-Enein H, Lee CT, Mansson W, Mills RD, Penson DF, et al. Urinary diversion: how experts divert. Urology. 2015;85(1):233–8. https://doi.org/10.1016/j.urology.2014.06.075.
Amini E, Djaladat H. Long-term complications of urinary diversion. Curr Opin Urol. 2015;25(6):570–7. https://doi.org/10.1097/MOU.0000000000000222.
Ahmed YE, Hussein AA, May PR, Ahmad B, Ali T, Durrani A, et al. Natural history, predictors and management of ureteroenteric strictures after robot assisted radical cystectomy. J Urol. 2017;198(3):567–74. https://doi.org/10.1016/j.juro.2017.02.3339.
Narita T, Hatakeyama S, Koie T, Hosogoe S, Matsumoto T, Soma O, et al. Presence of transient hydronephrosis immediately after surgery has a limited influence on renal function 1 year after ileal neobladder construction. BMC Urol. 2017;17(1):72.
Hashim H, Woose CJ. Ureteropelvic junction obstruction. Eur Urol Suppl. 2012;11:25–32. https://doi.org/10.1016/j.eursup.2012.01.004 (ISSN 1569-9056).
EAU guideline. https://uroweb.org/guideline/bladder-cancer-muscle-invasive-and-metastatic/. Accessed 06 July 2021.
Tartaglione G, D’Addessi A, De Waure C, Pagan M, Raccioppi M, Sacco E, et al. 99mTc-MAG3 diureticrenography in diagnosis of obstructive nephropathy in adults: a comparison between F-15 and a new procedure F+10(sp) in seated position. Clin Nucl Med. 2013;38(6):432–6. https://doi.org/10.1097/RLU.0b013e31828da3f5.
Esteves FP, Taylor A, Manatunga A, Folks RD, Krishnan M, Garcia EV. 99mTc- MAG3 renography: normal values for MAG3 clearance and curve parameters, excretory parameters, and residual urine volume. AJR Am J Roentgenol. 2006;187(6):W610–7. https://doi.org/10.2214/AJR.05.1550.
AIMN. Raccomandazioni procedurali in nefro-urologia: https://www.aimn.it/documenti/lineeguida/8_RP_AIMN_nefro-urologia.pdf. Accessed 06 July 2021.
Lobo N, Dupré S, Sahai A, Thurairaja R, Khan MS. Getting out of a tight spot: an overview of ureteroenteric anastomotic strictures. Nat Rev Urol. 2016;13(8):447–55. https://doi.org/10.1038/nrurol.2016.104.
Oh JJ, Byun SS, Jeong CW, Kwak C, Kim HH, Ku JH. Association Between preoperative hydronephrosis and prognosis after radical cystectomy among patients with bladder cancer: a systemic review and meta-analysis. Front Oncol. 2019;9:158.
Pantuck AJ, Han KR, Perrotti M, Weiss RE, Cummings KB. Ureteroenteric anastomosis in continent urinary diversion: long-term results and complications of direct versus non-refluxing techniques. J Urol. 2000;163(2):450–5. https://doi.org/10.1016/s0022-5347(05)67898-6.
Shah SH, Movassaghi K, Skinner D, Dalag L, Miranda G, Cai J, et al. Ureteroenteric strictures after open radical cystectomyand urinary diversion: the university of southern california experience. Urology. 2015;86(1):87–91. https://doi.org/10.1016/j.urology.2015.03.014.
De Nunzio C, Cindolo L, Leonardo C, Antonelli A, Ceruti C, Franco G, et al. Analysis of radical cystectomy and urinary diversion complications with the Clavien classification system in an Italian real-life cohort. Eur J Surg Oncol. 2013;39(7):792–8. https://doi.org/10.1016/j.ejso.2013.03.008.
Jinzaki M, Yamada Y, Nagura T, Nakahara T, Yokoyama Y, Narita K, et al. Development of upright computed tomography with area detector for whole- body scans: phantom study, efficacy on workflow, effect of gravity on human body, and potential clinical impact. Invest Radiol. 2020;55(2):73–83. https://doi.org/10.1097/RLI.0000000000000603.
Loran OB, Mudraia IS, David’iants AA, Zaĭtsev AV. Urodynamics of upper urinary tracts after intestinal plastic surgery on urinary bladder (experimental study)]. Urologiia. 1999;4:17–21.
Gordon I, Piepsz A, Sixt R. Auspices of paediatric committee of european association of nuclear medicine guidelines for standard and diuretic renogram in children. Eur J Nucl Med Mol Imaging. 2011;38(6):1175–88. https://doi.org/10.1007/s00259-011-1811-3.
Rossleigh MA, Leighton DM, Farnsworth RH. Diuresis renography The need for an additional view after gravity-assisted drainage. Clin Nucl Med. 1993;18(3):210–3.
Piepsz A, Tondeur M, Ham H. NORA: a simple and reliable parameter for estimating renal output with or without frusemide challenge. Nucl Med Commun. 2000;21(4):317–23. https://doi.org/10.1097/00006231-200004000-0000.
Tondeur M, De Palma D, Roca I, Piepsz A, Ham H. Inter-observer reproducibility in reporting on renal drainage in children with hydronephrosis: a large collaborative study. Eur J Nucl Med Mol Imaging. 2008;35(3):644–54. https://doi.org/10.1007/s00259-007-0641-9.
EANM. Dynamic renal imaging in obstructive renal pathology. https://www.eanm.org/content-eanm/uploads/2016/11/tech_dynamic.pdf. Accessed 06 July 2021.
Taylor AT. Radionuclides in nephrourology, Part 2: pitfalls and diagnostic applications. J Nucl Med. 2014;55(5):786–98. https://doi.org/10.2967/jnumed.113.133454.
Tartaglione G, Townsend DM, Bassi PF, Delgado Bolton RC, Giammarile F, Rubello D. Diuresis renography in equivocal urinary tract obstruction. A historical perspective. Biomed Pharmacother. 2019;116: 108981. https://doi.org/10.1016/j.biopha.2019.108981Accessed15September2020.
Taylor AT, Brandon DC, De Palma D, Blaufox MD, Durand E, Erbas B, et al. SNMMI procedure standard/eanm practice guideline for diuretic renal scintigraphy in adults with suspected upper urinary tract obstruction. Semin Nucl Med. 2018;48(4):377–90.
Catalá V, Solà M, Samaniego J, Martí T, Huguet J, Palou J, et al. CT findings in urinary diversion after radical cystectomy: postsurgical anatomy and complications. Radiographics. 2009;29(2):461–76. https://doi.org/10.1148/rg.292085146.
Perazella MA. Gadolinium-contrast toxicity in patients with kidney disease: nephrotoxicity and nephrogenic systemic fibrosis. Curr Drug Saf. 2008;3(1):67–75. https://doi.org/10.2174/157488608783333989.
Schöndorf D, Meierhans-Ruf S, Kiss B, Giannarini G, Thalmann GN, Studer UE, et al. Uretero ileal strictures after urinary diversion with an ileal segment-is there a place for endourological treatment at all? J Urol. 2013;190(2):585–90. https://doi.org/10.1016/j.juro.2013.02.039.
Katherine AA, Emily AV, Gillian S, Ali F, Daniel DS, Machele SD, et al. Predictors of benign uretero-enteric anastomotic strictures after radical cystectomy and urinary diversion. Urology. 2018. https://doi.org/10.1016/j.urology.2018.06.024.
van de Putte FEE, de Wall LL, van Werkhoven E, Heldeweg EA, Bex A, van der Poel HG, et al. Endo-urological techniques for benign uretero-ileal strictures have poor efficacy and affect renal function. Urol Int. 2018;100(1):18–24.
Tartaglione G, Foschi N, Recupero SM, Ieria FP, Tarantino G, Bassi P. Advantages of gravity-assisted diuretic renogram: F + 10 (seated position) method. Nucl Med Commun. 2021;42(6):602–10. https://doi.org/10.1097/MNM.0000000000001378.
Barber NJ, Thompson PM. Nephroptosis and nephropexy–hung up on the past? Eur Urol. 2004;46(4):428–33. https://doi.org/10.1016/j.eururo.2004.03.023.
Acknowledgements
None of the authors has a conflict of interest relatively to the topic of this article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a conflict of interest relatively to the topic of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tartaglione, G., Foschi, N., Ragonese, M. et al. A gravity-assisted approach to the management of urinary diversion: 99mTc-MAG3 diuresis renography with F + 10(sp) method. Ann Nucl Med 35, 1127–1135 (2021). https://doi.org/10.1007/s12149-021-01648-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-021-01648-x