Abstract
Purpose
To prospectively evaluate the value of whole-body cancer screening with multiple modalities including FDG-PET in a healthy population.
Methods
The study was conducted in 1197 healthy individuals aged ≥ 35 years at enrollment between August 2003 and July 2004. All participants were scheduled to receive annual whole-body cancer screening five times (screening period) with subsequent long-term follow-up (follow-up period). The endpoints of the study were definitive cancer diagnosis, cancer-related death, and all-cause death.
Results
The follow-up rate was 99.8% for the screening period and 96.2% for the follow-up period. Forty-five cancers were confirmed during the screening period (August 2003 to July 2009), and 37 of the 45 were detected by the screening. Fourteen of the 45 were PET positive. Sixteen, 5, 4, 9 and 11 cancers were confirmed after the first, the second, the third, the fourth, and the fifth (took 2 years) screening, respectively. Eight participants died, of whom five died of cancer. The rate of cancer incidence (per 100,000) of 628.7 (95% confidence interval [CI] 445.0–812.4) was significantly high, and the rates of cancer mortality and all-cause mortality of 69.9 (95% CI 8.6–131.1) and 111.8 (95% CI 34.3–189.2), respectively, were significantly low, compared with the corresponding rates of 379.3, 138.2 and 354.2, respectively, in the age-rank- and sex-matched general population. During the follow-up period (August 2009 to July 2013), 37 cancers were confirmed and 30 of the 37 were detected. Seven participants died, of whom three died of cancer. The rate of cancer incidence was 809.6 (95% CI 548.7–1070.5). The rates of cancer mortality and all-cause mortality of 65.6 (95% CI 0–139.9) and 153.2 (95% CI 39.7–266.6), respectively, were significantly low compared with 190.1 and 462.3, respectively, in the general population.
Conclusion
Cancer detection by PET alone was limited. While the high cancer incidence was attributed to the extensive screening, the low cancer and all-cause mortality may indicate the potential value of this type of cancer screening. Cancer incidence increases with aging and it has been shown that continuous screening may reduce the risk caused by the cancer progression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer is the most common cause of death in Japan. Various preventive and control measures have been taken by the Japanese government against this disease. Owing to these control measures and the marked progress in diagnostic and therapeutic techniques, age-adjusted cancer mortality has been decreasing steadily, but the number of cancer cases and cancer-related deaths continue to increase due to the increasing life expectancy of the population [1]. In addition, even with the latest treatment techniques, patients with an advanced cancer at the time of diagnosis still have poor prognoses. Therefore, early detection by cancer screening is one of the most effective ways of reducing cancer mortality and morbidity.
While the value of imaging-based screening has been investigated and proven in various cancer settings [2,3,4], each screening examination is intended for cancers of a single organ. Positron emission tomography (PET) and positron emission tomography/computed tomography (PET/CT) with [18F]fluorodeoxyglucose (FDG) are widely accepted diagnostic tools for the management of oncology patients with various types of cancer, and these are also used in whole-body cancer screening programs for healthy individuals in Japan but not in Europe and the United States. Initially encouraged by the pioneering report [5], the utilization of whole-body cancer screening including FDG-PET became widespread from around 2003, resulting in a steep increase in PET facilities [6,7,8,9,10]. The Japanese Society of Nuclear Medicine and the Clinical PET Promoting Committee issued guidelines for FDG-PET cancer screening in 2004 (revised in 2007, 2011 and 2019), and Japanese nationwide surveys have been conducted and have provided basic data about the performance and the risk-benefits of the screening [7, 11,12,13]. Recent surveys have shown that about 15% of FDG-PET (and FDG-PET/CT) examinations are used for cancer screening every year [14]. However, there is still no evidence justifying the value of this type of cancer screening.
We started a prospective study in August 2003 to evaluate the performance and value of whole-body cancer screening in healthy individuals. We scheduled five annual cancer screenings with long-term follow-up for individuals in a single corporate health insurance society. The results of the first three annual screenings have already been reported [10]. While a wide variety of early-stage cancers were detected, the negative aspects of the screening, including the high detection rate of indolent cancers and false-positive screening results, were also noted, and the value of this screening approach remained to be verified.
The screening period of the study ended in July 2009, and the follow-up period is still underway. In this manuscript, we summarized the results of the 6-year screening period and a 4-year follow-up period as of the end of 2014 to evaluate the value of this kind of whole-body cancer screening.
Materials and methods
Participants
The study was conducted in 1197 healthy individuals without a previous history of cancer aged ≥ 35 years at enrollment between August 2003 and July 2004. All participants were employees of Hamamatsu Photonics, KK and its affiliated companies (Hamamatsu, Shizuoka, Japan) and belonged to the Photonics Group Health Insurance Society. The society has been providing annual health check-ups for employees, including cancer screening tests like upper gastrointestinal barium study, fecal occult blood (FOB) testing, prostate-specific antigen (PSA) assessment, chest X-p and mammography for the applicant. In this study, all participants were offered five annual whole-body cancer screenings with multiple examinations including whole-body FDG-PET (screening period) and subsequent long-term follow-ups (follow-up period). The study protocol was approved by the ethics committee of the Hamamatsu Medical Photonics Foundation and all participants provided written informed consent.
Cancer screening
The whole-body cancer screening protocol included medical interviews pertaining to family and personal histories of diseases as well as smoking and dietary habits; imaging examinations by whole-body FDG-PET, chest and abdominal CT, and brain and pelvic magnetic resonance imaging; analyses of serum tumor markers including carcinoembryonic antigen, cancer antigen 19-9, squamous cell carcinoma antigen, and PSA for men and cancer antigen 125 for women; and FOB testing. Abdominal ultrasonography was included in the second screening. Barium upper gastrointestinal series (or upper gastrointestinal endoscopy) and mammography were also performed for applicants in the annual health check-ups for employees.
In the follow-up period, participants continued biannual whole-body cancer screening by their own will in addition to annual health check-up. After their retirement, they underwent cancer screening tests personally in their capacity.
Imaging modalities
FDG-PET studies were performed on a dedicated PET scanner with a long axial field of view of 50 cm (SHR-92000, Hamamatsu Photonics KK, Hamamatsu, Japan) [15, 16], and whole-body images from the top of the head to the upper part of the thigh were obtained by two-bed positions (6–7 min/scan). All participants fasted for 5 h before the study, and serum glucose levels were measured just before the FDG injection. The scan was started 60 min after injection of 3 MBq FDG/kg bodyweight (mean effective dose of 3.6 mSv). Attenuation correction was performed using a low radiation dose CT (120 kV, 10 mAs, effective dose lower than 0.5 mSv). We used a mat (BlueBAG, Medical Intelligence, Nagoya, Japan), individually formed in the CT, to reproduce the body position in the PET for attenuation correction. Diagnostic CT images without contrast enhancement of the chest and upper abdomen were obtained with reduced radiation dose (mean effective dose of 4 mSv). MRI were performed on a 1.5 T MR scanner without contrast enhancement, basically using T1- and T2-weighted fast spin echo sequences for imaging of the brain and the pelvis [10].
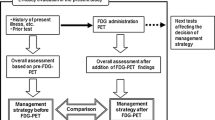
Assessment of screening results
At least two experienced radiologists of the Hamamatsu Medical Imaging Center interpreted the images according to the standard diagnostic procedure. For the interpretation of PET images, a finding of a focal area of increased uptake, regardless of the standard uptake value, was considered positive, but the final classification was modified by the finding of other imaging modalities when needed. Most processes for interpretation were similar to the diagnostic criteria appeared in the previous report [17]. We classified the findings as “suggestive” of malignancy, for which a further examination was needed, “possible” malignancy, for which a follow-up examination was recommended, and “negative” for malignancy, which included cases with benign diseases and those with no abnormality. The first two categories were deemed “positive” for malignancy. Positive FOB test results were categorized as “suggestive”. The tumor marker results were also categorized as “suggestive”, “possible”, and “negative”, according to the preset threshold values [10].
Outcome and follow-up evaluation
Participants with positive screening results were referred to a local hospital or followed up to obtain a definitive diagnosis. In those with negative screening results, the presence of cancer at the previous screening was ascertained at the next screening. We contacted each participant who did not undergo the next screening to check cancer occurrence after the screening. These procedures were repeated after each annual screening.
After the end of the screening period, the participants were continuously surveyed via questionnaires sent to each participant, health insurance society records, and the results of the optional whole-body cancer screening provided to participants biannually throughout the follow-up period.
Statistical analysis
The endpoints of this study were definitive cancer diagnosis, cancer-related death, and all-cause death. The rates of cancer incidence, cancer mortality, and all-cause mortality (per 100,000) along with their respective 95% confidence intervals (CIs) in this study population were calculated as the number of cancer occurrences, cancer-related deaths, and all-cause deaths, respectively, divided by the number of person-years for 6 years of the screening period and for 4 years of the follow-up period. The corresponding values in the age-rank- and sex-matched general population were calculated for each year from 2003 to 2012 based on the Cancer Statistics in Japan [18] and Vital Statistics in Japan [19] and averaged for the screening and follow-up periods for comparison.
Results
Status at each screening and follow-up
The participants consisted of 838 men and 359 women with mean (± SD) age of 46.7 (± 7.7) years (Online Resource 1). The numbers of participants who underwent the second, third, fourth, and fifth cancer screenings were 1156 (96.6%), 1120 (93.6%), 1071 (89.5%), and 1034 (86.4%), respectively. The screening was performed annually, but the completion of the fifth screening took 2 years (August 2007 to July 2009). In the screening period, summarized as of the end of 2010, 1187 participants (99.2%) were confirmed as being alive and eight (0.7%) were dead; the current status of two participants (0.2%) was unknown. The follow-up rate was 99.8%.
In the follow-up period, summarized as of the end of 2014, 922 participants (77.0%) remained in the companies and were confirmed to be alive and 15 (1.2%) were dead. Of the remaining 260 (21.7%) who left the companies, 214 (17.9%) were reported to be alive and seven of them had developed cancer. The follow-up rate was 96.2%.
Cancer incidence and detection
Forty-five malignant tumors were confirmed in the screening period as of the end of 2010: 16 after the first, 5 after the second, 4 after the third, 9 after the fourth and 11 after the fifth screening (Table 1). Thirty-seven of the 45 cancers (82%) were detected by the screening: 28 of the 37 by the whole-body cancer screening and 9 by the annual health check-up or by the cancer screening performed in their personal capacity. Twenty-one of the 28 showed positive results in the initial screening, including a considerable number of indolent cancers. Fourteen of the 45 were PET positive. Seven of the 45 were diagnosed after symptom development. Details regarding cancer detection were not known in one participant. The rate of cancer incidence was 628.7 (95% [CI] 445.0–812.4), and the 95% CI was above the corresponding rate of 379.3 in the age-rank- and sex-matched general population (Online Resource 2), indicating a significantly higher cancer incidence (p < 0.05).
Thirty-seven malignant tumors were confirmed in the follow-up period as of the end of 2014 (Table 2): 16 in the first 2 years and 21 in the second 2 years. Thirty of the 37 (81%) were detected by the screening. The annual cancer incidence rates gradually increased (Fig. 1), but the rate of 809.6 (95% CI 548.7–1070.5) in this period was not significantly different from the corresponding rate of 591.1 in the age-rank- and sex-matched general population.
Changes of cancer incidence rates (with standard errors) in the study population and those in the age-rank- and sex-matched general population during the study period. Gradual increases in the cancer incidence rates in this study population and the general population seem to be a consequence of aging
Although there were many positive test results because of multiple testing (Online Resource 3), all other cases with positive results were diagnosed as having no or benign diseases or followed up uneventfully throughout the study period.
Cancer-related death and all-cause death
In the screening period, eight participants died, of which five died due to cancer (Table 3). The rates of cancer mortality and all-cause mortality were 69.9 (95% CI 8.6–131.1) and 111.8 (95% CI 34.3–189.2), respectively, and the 95% CIs were below the corresponding rates of 138.2 and 354.2, respectively, in the age-rank- and sex-matched general population, indicating significantly lower cancer and all-cause mortality (p < 0.05).
In the follow-up period, seven participants died, of which three died due to cancer (Table 3). The rates of cancer mortality and all-cause mortality were 65.6 (95% CI 0–139.9) and 153.2 (95% CI 39.7–266.6), respectively, and the 95% CIs were below the corresponding rates of 190.1 and 462.3, respectively, in the age-rank- and sex-matched general population, indicating significantly lower cancer and all-cause mortality (p < 0.05).
Discussion
In this prospective study, a total of 82 malignant tumors across a wide variety of organs were confirmed in the 1197 participants during the 10-year study period. Sixty-seven of the 82 tumors (82%) were detected by the screening tests, and most of them were at the early stages. The detectability of PET alone is limited in several types of cancer and only one-third of cancers were PET positive. Complementary screening tests are combined to reduce false-negative and false-positive screening results, but nearly 20% of cancers were not detected even with the combination of the screening tests. Eight cancers (10%) were very aggressive and these participants died of cancer. Even with extensive annual screening, it was difficult to detect all the cancers at early stages.
In the initial screening, we encountered a considerable number of cancers which may be indolent and harmless for a long period of time without affecting cancer mortality. Of the 28 cancers detected in the 6-year screening period, 21 showed abnormal findings in the initial screening, and more than half—likely comprising most of thyroid and lung cancers—seemed to be indolent. Most of these cancers pooled in the population were dredged up by the initial screening and this may be one of the reasons for high cancer incidence in this study.
Cancer incidence was very high in the initial screening but reduced in the following screenings. However, it gradually increased again. This increase can be attributed to increasing age (Fig. 1). Among people in their 40 s and 50 s, a 5-year increase in age can lead to a doubling of cancer incidence [18]. Although a considerable number of interval cancers were detected annually by the screening, cancer incidence may not have decreased owing to or masked by, the rise in the rates of cancer development with increasing age. Therefore, continuous and periodical cancer screening is necessary to avoid the risk caused by cancer progression.
In contrast with cancer incidence, cancer mortality in this study population was significantly lower than that in the age-rank- and sex-matched general population not only in the screening period but also in the follow-up period. After the end of the screening period, most participants continued to receive annual health check-ups, and about 60% of them willingly continued to undergo biannual whole-body cancer screening. While the higher cancer incidence can be attributed simply to the greater detection of cancers by the extensive screening, the lower cancer mortality indicates the potential value of this cancer screening approach.
In the homogeneous group of participants in this study who received annual health check-ups, the effect of a selection bias on cancer mortality should be also considered. The types of cancers detected in this study somewhat differed from those in the other studies and in general applicants for whole-body cancer screening of our center [20]; there was no colon cancer at all and all lung cancers were FDG-PET negative in the first three screenings [10]. We checked the records of the Photonics Group Health Insurance Society for over a period of 5 years before the start of this study (from 1998 to 2002) and found that the rate of cancer incidence was significantly high (Online Resource 4). Although no significant difference was observed in the rate of cancer mortality, the late effect of cancer detections through annual health check-ups for many years seems to contribute on the decrease of cancer mortality in this study.
In addition to cancer mortality, all-cause mortality was also significantly low in this population. The use of multimodal whole-body screening allows the detection of not only cancers but also many other diseases, including lifestyle-related conditions. In our study, participants were provided personal optimal lifestyle-related guidance based on the screening results, including imaging tests. The repeated guidance provided over the course of the study, in addition to the annual health check-ups, may have helped increase health-related awareness and reduce all-cause mortality.
We encountered many indolent cancers in the initial screening. The issue of overdiagnosis is important but difficult to cope with, because the malignant potential of each tumor is not known at the time of diagnosis [21]. It is also difficult to predict if early cancer detection by cancer screening helps improve everyone’s survival. Since the presence of such cases in the extensive screening programs is inevitable, it is important to properly address this issue by sharing information that can reduce unnecessary further examinations and treatments. Also important is that patients are appropriately informed of the nature and the magnitude of the trade-off involved with early cancer detection.
Reducing false positive rate is also important because false positive results trigger unnecessary medical expenses for further examination, which impact both individuals and the public health care system and cause psychological stress in patients [10]. In the repeated screening, false positives in imaging studies decrease considerably (reduced by 80% in this study), but those in non-imaging studies are stable (Online Resource 3). As the results, the allover positive rate was 22% in the initial screening but decreased to 10–15% in the second to the fifth screening in this study. Regarding the initial screening, as discussed well in the previous article [10], false-positive findings can be reduced and the positive predictive value improve by the modification of diagnostic criteria and the improvement of diagnostic skills through the practice. These were also shown in another population through the period from 2004 to 2008 [22].
As to limitations of this study, the study population was small, and the number of cancers and cancer-related deaths observed were limited, which could result in statistical instability and decrease the reliability of the results. However, comparable findings in the two sequential “screening” and “follow-up” periods may help increase the reliability of the results. A randomized controlled trial is the only way to verify the reduction in cancer mortality by screening, but it seems impractical to conduct the trial in the future because of huge costs for many expensive imaging tests and difficulties for randomization in a situation of Japan where this type of cancer screening including FDG-PET (and PET/CT) is widely recognized. We could not conduct the trial because randomization was not acceptable in the health insurance society to avoid inequality among employees.
Another concern may be radiation exposure caused by PET and CT. Although we used an FDG dose that was 20% lower and a CT radiation dose that was less than half of the average doses reported in the nationwide survey [12], recent advancements in both PET and CT technologies will enable further reduction of radiation exposure and may make it acceptably low for general use in the near future [23,24,25]. At present, it is important to ensure that individuals who undergo screening are adequately informed of the merits as well as the demerits associated with cancer screening. To reduce radiation exposure, biannual whole-body cancer screening may be performed without an apparent increase of the risk by the cancer progression, if complemented by population-based cancer screening every other year.
The issue of cost-effectiveness should be also clarified, but an expensive multimodal imaging-based screening does not seem to be suitable for general use at present. In a tentative analysis by the collaboration of our center and the health insurance society, the direct medical costs of cancer cases were less in the participant group than in the non-participant group, but the costs of the imaging tests were substantial, and socio-economic gains by extending the lifespans of employees through cancer screening were not easy to incorporate. Therefore, such cancer screening programs should be used for personal screening as performed in Japan but could be cost-effectively employed in populations at high risk for cancer, if such populations can be appropriately identified by less expensive prescreening tests.
In conclusion, cancer detection by PET alone was limited. While the high cancer incidence can be attributed to the extensive screening, the low cancer mortality and all-cause mortality suggest the potential value of this type of cancer screening. Interval cancers increase with aging and it has been shown that continuous and periodical cancer screenings may reduce the risk caused by the cancer progression. Continuing follow-ups of this study population will help to further elucidate how this type of whole-body cancer screening affect cancer and all-cause mortality.
References
Ministry of Health, Labour and Welfare, Japan. Vital statistics in Japan. 2018. https://ganjoho.jp/data/reg_stat/statistics/brochure/2018/cancer_statistics_2018.pdf. Accessed 22 Sept 2019.
National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. https://doi.org/10.1056/NEJMoa1102873.
Ohuchi N, Suzuki A, Sobue T, Kawai M, Yamamoto S, Zheng YF, et al. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-cancer Randomized Trial (J-START): a randomized controlled trial. Lancet. 2016;387:341–8. https://doi.org/10.1016/S0140-6736(15)00774-6.
Regge D, Iussich G, Segnan N, Correale L, Hassan C, Arrigoni A, et al. Comparing CT colonography and flexible sigmoidoscopy: a randomised trial within a population-based screening programme. Gut. 2017;66:1434–40. https://doi.org/10.1136/gutjnl-2015-311278.
Yasuda S, Ide M, Fujii H, Nakahara T, Mochizuki Y, Takahashi W, et al. Application of positron emission tomography imaging to cancer screening. Br J Cancer. 2000;83:1607–11. https://doi.org/10.1054/bjoc.2000.1496.
Kojima S, Zhou B, Teramukai S, Hara A, Kosaka N, Matsuo Y, et al. Cancer screening of healthy volunteers using whole-body 18F-FDG-PET scans: the Nishidai clinic study. Eur J Cancer. 2007;43:1842–8. https://doi.org/10.1016/j.ejca.2007.05.010.
Minamimoto R, Senda M, Uno K, Jinnouchi S, Iinuma T, Ito K, et al. Performance profile of FDG-PET and PET/CT for cancer screening on the basis of a Japanese Nationwide Survey. Ann Nucl Med. 2007;21:481–98. https://doi.org/10.1007/s12149-007-0061-8.
Ono K, Ochiai R, Yoshida T, Kitagawa M, Omagari J, Kobayashi H, et al. The detection rates and tumor clinical/pathological stages of whole-body FDG-PET cancer screening. Ann Nucl Med. 2007;21:65–72.
Terauchi T, Murano T, Daisaki H, Kanou D, Shoda H, Kakinuma R, et al. Evaluation of whole-body cancer screening using 18F–2-deoxy-2-fluoro-d-glucose positron emission tomography: preliminary report. Ann Nucl Med. 2008;22:379–85. https://doi.org/10.1007/s12149-008-0130-7.
Nishizawa S, Kojima S, Teramukai S, Inubushi M, Kodama H, Maeda Y, et al. Prospective evaluation of whole-body cancer screening with multiple modalities including [18F]fluorodeoxyglucose positron emission tomography in a healthy population: a preliminary report. J Clin Oncol. 2009;27:1767–73. https://doi.org/10.1200/JCO.2008.18.2238.
Minamimoto R, Senda M, Terauchi T, Jinnouchi S, Inoue T, Iinuma T, et al. Analysis of various malignant neoplasms detected by FDG-PET cancer screening program: based on a Japanese Nationwide survey. Ann Nucl Med. 2011;25:45–54. https://doi.org/10.1007/s12149-010-0428-0.
Nurano T, Minamimoto R, Senda M, Uno K, Jinnouchi S, Fukuda H, et al. Radiation exposure and risk-benefit analysis in cancer screening using FDG-PET: results of Japanese nationwide survey. Ann Nucl Med. 2011;25:657–66. https://doi.org/10.1007/s12149-011-0511-1.
Minamimoto R, Senda M, Jinnouchi S, Terauchi T, Yoshida T, Murano T, et al. The current status of an FDG-PET cancer screening program in Japan, based on a 4-year (2006–2009) nationwide survey. Ann Nucl Med. 2013;27:46–57. https://doi.org/10.1007/s12149-012-0660-x.
Isotope news [in Japanese]. 2019. https://www.jrias.or.jp/books/catalog.html, recent document in https://www.jrias.or.jp/books/pdf/201802_SHIRYO_KAMIYA.pdf. Accessed 22 Sept 2019.
Watanabe M, Shimizu K, Omura T, Sato N, Takahashi M, Kosugi T, et al. A high-throughput whole-body PET scanner using flat panel PS-PMTs. IEEE Trans Nucl Sci. 2004;51:796–800.
Tanaka E, Kudo H. Subset-dependent relaxation in block-iterative algorithms for image reconstruction in emission tomography. Phys Med Biol. 2003;48:1405–22.
Minamimoto R, Senada M, Jinnouchi S, Yoshida T, Nakashima R, Nishizawa S, et al. Assessment of diagnostic criteria for FDG-PET cancer screening program according to the interpretation of FDG-PET and combined examination [in Japanese]. Kaku Igaku. 2009;46:73–93.
National Cancer Center. Cancer Statistics in Japan [in Japanese]. 2019. https://ganjoho.jp/reg_stat/statistics/dl/index.html. Accessed 22 Sept 2019.
Ministry of Health, Labour and Welfare, Japan. Vital statistics in Japan [in Japanese]. 2019. https://www.mhlw.go.jp/toukei/list/81-1a.html. Accessed 22 Sept 2019.
Nishizawa S, Okada H. PET cancer screening with multiple imaging modalities: current status and prospects (in Japanese). Jpn J Clin Radiol. 2017;62:645–53.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102:605–13. https://doi.org/10.1093/jnci/djq099.
Nishizawa S, Kodama H, Maeda Y, Okada H. Whole-body cancer screening with multiple modalities including FDG-PET: a summary of 5 year’s practice for general asymptomatic individuals. Eur J Nucl Med Mol Imaging. 2009;36(suppl 2):S356. https://doi.org/10.1007/s00259-011-1910-1.
Cherry SR, Jones T, Karp JS, Qi J, Moses WW, Badawi RD. Total-body PET: maximizing sensitivity to create new opportunities for clinical research and patient care. J Nucl Med. 2018;59:3–12. https://doi.org/10.2967/jnumed.116.184028.
Zhang X, Xie Z, Berg E, Judenhofer MS, Liu W, Xu T, et al. Total-body dynamic reconstruction and parametric imaging on the uEXPLORER. J Nucl Med. 2019. https://doi.org/10.2967/jnumed.119.230565(Epub ahead of print).
Zhang H, Wang J, Zeng D, Tao X, Ma J. Regularization strategies in statistical image reconstruction of low-dose x-ray CT: a review. Med Phys. 2018;45:e886–e907. https://doi.org/10.1002/mp.13123.
Acknowledgements
We thank all the collaborated staff of this research in the Hamamatsu Medical Imaging Center, Hamamatsu Photonics KK and the Photonics Group Health Insurance Society.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no potential conflicts of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nishizawa, S., Kojima, S., Okada, H. et al. Ten-year prospective evaluation of whole-body cancer screening with multiple modalities including [18F]fluorodeoxyglucose positron emission tomography in a healthy population. Ann Nucl Med 34, 358–368 (2020). https://doi.org/10.1007/s12149-020-01456-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-020-01456-9