Abstract
Purpose
To evaluate the contributory value of Fluorine-18 fluorodeoxyglucose (F-18 FDG) positron emission tomography/computed tomography (PET/CT) in the prediction of lymphovascular tumor invasion in patients with lung adenocarcinoma.
Materials and methods
We evaluated F-18 FDG-PET/CT images in 84 patients with histopathologically proven lung adenocarcinoma (37 men and 47 women, age range 39–83 years, mean age 67.0 ± 8.9 years). The maximum standardized uptake values (SUVmax) of the carcinomas were measured from the PET images. The Mann–Whitney U test was conducted to compare the median SUVmax between the tumor groups with and without lymphovascular invasion. In the subgroup patients with no lymph-node metastasis, we also compared the median SUVmax between the tumor groups with and without lymphatic invasion.
Results
The tumors with lymphovascular invasion had a significantly (P < 0.0001) greater median SUVmax than those without invasion. In the subgroup patients with no lymph-node metastasis, the median SUVmax was higher in tumors with lymphatic invasion than those without (P = 0.0004). The sensitivity, specificity, and area under the receiver operating characteristic curve for the detection of tumors with lymphovascular invasion were 89, 75 %, and 0.82, respectively, with a cutoff SUVmax value of 2.32.
Conclusion
The SUVmax of lung adenocarcinoma is a potential imaging biomarker for predicting tumor lymphovascular invasion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the most common cause of cancer-related death in men and women in the United States. For 2015, the American Cancer Society has estimated approximately 221,200 new cases and 158,040 deaths due to this disease [1]. Non-small cell lung cancer (NSCLC) accounts for approximately 80 % of all cases of primary lung cancers [2]. Surgical resection is the most effective treatment for resectable NSCLCs; however, the postoperative survival rate remains unsatisfactory, even when the tumor is resected in stage IA [3]. Previous studies demonstrated that pathological lymphovascular invasion is a poor prognostic factor for recurrence-free and overall survival in NSCLC patients [4–6].
Widely used in workups, fluorine-18 fluorodeoxyglucose (F-18 FDG)-positron emission tomography/computed tomography (PET/CT) contributes to the detection, differential diagnosis, staging and restaging, therapeutic decision-making, follow-up, and prediction of prognosis for most malignancies [7, 8]. The efficacy of F-18 FDG PET imaging is supported by the fact that cancer cells commonly exhibit increased glucose transporter (GLUT) expression [9] as well as higher levels of hexokinase and phosphofructokinase activity that promotes glycolysis [10]. The increase in glucose uptake across cancer cell membranes and/or increased glycolytic rates in cancer cells results in a subsequent increase in F-18 FDG uptake in tumors.
Previous studies have described the usefulness of F-18 FDG-PET/CT for evaluating of tumor staging, mediastinal lymph-node metastasis, prognostic value in the patients with lung cancer [11–13]. However, no published study has evaluated the association between F-18 FDG uptake and lymphovascular invasion. Lymphovascular invasion is one of the worse prognostic factor in the patients with stage IA NSCLC [14]. Generally, follow-up and surveillance without adjuvant therapy are recommended after complete resection; however, some cases which have worse prognosis need more careful follow-up and/or adjuvant therapy [15]. We postulate that imaging characteristics of F-18 FDG-PET/CT could be further exploited to help predict lymphovascular invasion in patients with NSCLC. Thus, the purpose of this study was to evaluate the contributory value of F-18 FDG uptake on PET/CT in the prediction of lymphovascular invasion in patients with lung adenocarcinoma.
Materials and methods
Patients
This retrospective study was approved by our institutional review board and written informed consent was waived. Between February 2012 and December 2013, 119 patients with histopathologically proven lung adenocarcinoma underwent F-18 FDG-PET/CT imaging for preoperative tumor staging. Thirty-five of the 119 patients were excluded because they lacked histopathological evaluation in terms of lymphovascular invasion. Thus, the remaining 84 patients (mean age 67.0 ± 8.9 years, age range 39–83 years), included 37 men (mean age 65.0 ± 8.9 years, age range 39–78 years) and 47 women (mean age 68.6 ± 8.6 years, age range 43–83 years) were including in our study. Ninety-one lung adenocarcinomas (maximal diameter range 3–65 mm, mean 18.1 ± 10.9 mm) were identified in these 84 patients.
F-18 FDG-PET/CT imaging
Patients were instructed to fast for at least 5 h prior to F-18 FDG-PET/CT acquisition. Blood glucose levels measured before scanning were lower than 200 mg/dl in all patients. All imaging was performed with a 16-section PET/CT scanner (Biograph Sensation 16; Siemens Medical Solutions, Erlangen, Germany) that comprised a 16-section high-performance multi-detector low CT scanner with a lutetium oxyorthosilicate-based PET scanner. Sixty minutes after the administration of 200.0 MBq of F-18 FDG, whole-body CT, covering the vertex to the pelvis, was performed during breath holding at the midexpiration phase. The parameters were as follows: section width, 5 mm; table feed per rotation, 18 mm; time per table rotation, 0.5 s; tube voltage, 120 kVp; quality referenced mAs, 100mAs in CARE Dose 4D; and field of view, 70 cm. After CT scan, the emission scan was followed by a 2-min transmission scan per bed position in 3-D mode. Image of seven to nine bed positions (16.2 cm of axial field of view), 2 min each, were acquired. The attenuation-corrected PET images were reconstructed from the CT data using a 3-D ordered subset expectation maximization algorithm (8 subsets, 3 iterations).
PET image analysis
A nuclear medicine physician (with 8 years of experience in the interpretation of PET images), who was unaware of patient clinical information, retrospectively reviewed all F-18 FDG-PET/CT images on a commercially available dedicated Digital Imaging and Communications in Medicine (DICOM) viewer. First, lesion borders of the lung adenocarcinomas were identified on the axial CT images. Then, the nuclear medicine physician measured a maximum standardized uptake value (SUVmax) of the identified lung adenocarcinoma by drawing a region-of-interest (ROI) encompassing the entire lesion on the axial PET images.
Standard of reference
All histopathological specimens were obtained from surgery. The standard of reference was based on the histopathological evaluation using hematoxylin–eosin staining of tissues obtained from each patient. Lymphovascular invasion was reported when tumor cells were observed within lymphatic channels or veins on the histopathologic examination.
Statistical analysis
Statistical analyses except for stepwise logistic regression analysis were performed using MedCalc Software for Windows (version 13.1.1). Stepwise logistic regression analysis was performed SPSS software (version 21, IBM). Patient age, height, weight and gender were compared between the patient groups with and without lymphovascular invasion using the Mann–Whitney U and Chi-square tests, respectively. Before Mann–Whitney U test, F test was performed to evaluate equal variances. The median maximum diameter and SUVmax were compared between the tumor groups with and without lymphovascular invasion using Mann–Whitney U test. Stepwise logistic regression analysis was performed for the discrimination of tumors with lymphovascular invasion using the following parameters: patient age, gender, tumor maximum diameter, and tumor SUVmax. In a subgroup of patients who had no lymph-node metastasis, we also compared the patient age, height, weight and gender between the patient groups with or without lymphatic invasion, and compared tumor maximum diameter and SUVmax between the lesion groups with or without lymphatic invasion.
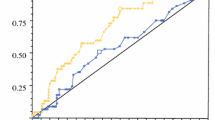
Receiver operating characteristic (ROC) curves were fitted to compute the sensitivity, specificity, and area under the ROC curve (AUC) in the detection of tumors with lymphovascular invasion. An optimal cutoff value that yielded the maximal sensitivity and specificity in the detection of tumors with lymphovascular invasion was determined using the ROC curves. In the subgroup patients with no lymph-node metastasis, we also computed the sensitivity, specificity, and AUC for the detection of tumors with lymphatic invasion. A P value less than 0.05 was considered to be significant.
The post hoc power analyses were performed in terms of the type II error and effect size using commercially available software (G*Power, version 3.1.2, University of Duesseldorf, Germany).
Results
Patient background factors and tumor characteristics
Table 1 summarizes both the patient demographics and histopathological findings of the 91 lung adenocarcinomas. First, the variances of each parameter between the two groups were assumed to be equal (P = 0.13–0.69). We did not find any significant differences in terms of age (P = 0.72), height (P = 0.77), weight (P = 0.69) or gender (P = 0.23) between the patient groups with (n = 27) and without (n = 64) lymphovascular invasion (Table 2). However, the tumors with lymphovascular invasion had statistically significantly greater maximal diameters (range 9.0–65.0, mean 23.6 ± 12.1) than those without invasion (range 3.0–45.0, mean 13.9 ± 9.7) (P = 0.0005) (Table 2).
Correlation between tumor SUVmax and histopathological lymphovascular invasion
We next evaluated the SUVmax of tumors from the different groups. The tumors with lymphovascular invasion had significantly greater median SUVmax values (range 1.4–18.5, mean 6.3 ± 4.1) than those without (range 0.4–11.0, mean 2.0 ± 2.0) (P < 0.0001) (Figs. 1, 2, 3). Stepwise logistic regression analysis demonstrated that only the tumor SUVmax could be used to discriminate between tumors with and without lymphovascular invasion (P = 0.001) (Table 3). In the detection of tumors with lymphovascular invasion, a cutoff SUVmax of 2.32 yielded the sensitivity, specificity, and AUC of 89, 78 %, and 0.88, respectively (Table 4). The post hoc power analysis showed that we had 67.1 % power to detect a 5 % difference between the tumors with and without lymphovascular invasion.
Box plot showing the tumor SUVmax for tumors with and without lymphovascular (LV) invasion. The median SUVmax of the tumors with lymphovascular invasion was significantly greater than those without invasion (P < 0.0001). Boundaries of boxes closest to zero are the 25th percentile, lines in boxes are the medians, boundaries of boxes farthest from zero are the 75th percentile, error bars are the smallest and largest values in 1.5 box lengths of 25th and 75th percentiles, and dots indicate the outliers, and significant difference found by the Mann–Whitney U test (P < 0.0001)
Correlation between tumor SUVmax and lymphatic invasion in subgroup patients
In a subgroup of 62 patients with 70 tumors (maximal diameter range 3–45 mm, mean 15.8 mm ± 9.1 mm) that manifested no lymph-node metastasis, 7 tumors had histopathological lymphatic invasion whereas 63 tumors had no invasion. We found no significant difference in the maximum tumor diameter of tumors between these two groups (P = 0.35). We did find that the tumors with lymphatic invasion had a significantly greater median SUVmax (range 1.6–11.0, mean 5.9 ± 3.2) than those without (range 0.4–11.0, mean 1.8 ± 1.6) (P = 0.0004) (Figs. 4, 5, 6). Again, stepwise logistic regression analysis demonstrated that the only parameter that could differentiate between tumors with and without lymphatic invasion was the tumor SUVmax (P = 0.024) (Table 3). In the detection of tumors with lymphatic invasion, a cutoff SUVmax of 3.26 yielded the sensitivity, specificity, and AUC of 86, 89 %, and 0.91, respectively (Table 4).
Box plot showing the SUVmax for 70 tumors with no lymph-node metastasis. The median SUVmax of tumors with lymphatic invasion was significantly greater than that without (P = 0.0004). Boundaries of boxes closest to zero are the 25th percentile, lines in boxes are the medians, boundaries of boxes farthest from zero are the 75th percentile, error bars are the smallest and largest values in 1.5 box lengths of 25th and 75th percentiles, and dots indicate the outliers, and significant difference found by the Mann–Whitney U test (P = 0.0004)
Discussion
F-18 FDG-PET/CT is a functional imaging modality to detect various malignant tumors on the basis of increased glucose uptake. It appears that a correlation exists between the degree of F-18 FDG uptake and tumor aggressiveness for various malignancies [16–18]. Indeed, previous studies demonstrated the usefulness of F-18 FDG-PET/CT to predict the prognosis of patients with NSCLC [19, 20].
There are several prognostic factors associated with NSCLC patients, including lymph-node metastasis that is the most commonly recognized prognostic factor for poor outcome. For patients without lymph-node metastasis who are in stage IA NSCLC, Goldstein et al. [14] demonstrated that the lymphovascular invasion was the strongest poor prognostic factor. Funai et al. [21] reported that the patients with lymphovascular invasion (5-year survival rate: 71 %) had a significantly worse prognosis than those without (5-year survival rate: 95 %). Moreover, in patients with no lymph-node metastasis, the patients with lymphatic invasion (overall survival: 85 %) had a significantly worse prognosis than those without (overall survival: 97 %) [6]. Thus, the presence of lymphovascular or lymphatic invasion appears to serve as an important prognostic factor for distant metastases and decreased long-term survival.
The tumor cells are often exposed to hypoxic states due to radiation therapy or other cancer treatments. The increases in malignant progression and treatments resistance are common manifestations of hypoxia-induced proteomic and genomic changes within the tumor cells. One of the major promoters of tumor cell adaptation to hypoxic states is the transcription hypoxia-inducible transcription factor (HIF-1). HIF-1 activates not only GLUT-1 and hexokinase to increase F-18 FDG uptake, but also vascular endothelial growth factor, other processes essential to tumor cell survival, propagation, and spread [22, 23]. We believe that tumor glucose metabolism is related to the local invasion or metastatic potential. In our results, the tumors with lymphovascular or lymphatic invasion presented with greater SUVmax than those without invasion. Moreover, in stepwise logistic analysis, the SUVmax was the only significant parameter to discriminate tumors with lymphovascular or lymphatic invasion. Our data suggested the SUVmax cutoff value of 2.32 appears to be a valuable index in the detection of tumors with lymphovascular invasion. This cutoff value was comparable with that published in a previous study: Higuchi et al. [24] reported that the SUVmax cutoff value of 2.5 could be used to predict for 5-year disease-free survival.
Our study had several limitations. First, this study was a retrospective study with a relatively small sample size. Further clinical studies with larger sample sizes may be necessary to validate our quantitative data. Second, we evaluated only lung adenocarcinoma. It will be helpful to consider and evaluate other histological subtypes of NSCLC. Finally, we administered 200.0 MBq of F-18 FDG in all patients regardless of patient height or weight, however, patient height and/or weight were statistically comparable in variance between the two groups. So, we believe that the results were little affected by the difference of F-18 FDG dose.
In summary, our study demonstrated a significant association between the SUVmax of lung adenocarcinoma and tumor lymphovascular invasion. The SUVmax appears to be a potential imaging biomarker for predicting the presence of tumor lymphovascular invasion in patients with lung adenocarcinoma.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5–29.
Poleri C, Morero JL, Nieva B, Vazquez MF, Rodriguez C, de Titto E, et al. Risk of recurrence in patients with surgically resected stage I non-small cell lung carcinoma: histopathologic and immunohistochemical analysis. Chest. 2003;123(6):1858–67.
Sawabata N, Asamura H, Goya T, Mori M, Nakanishi Y, Eguchi K, et al. Japanese Lung Cancer Registry Study: first prospective enrollment of a large number of surgical and nonsurgical cases in 2002. J Thorac Oncol. 2010;5(9):1369–75.
Shiono S, Abiko M, Sato T. Positron emission tomography/computed tomography and lymphovascular invasion predict recurrence in stage I lung cancers. J Thorac Oncol. 2011;6(1):43–7.
Giraud P, Antoine M, Larrouy A, Milleron B, Callard P, De Rycke Y, et al. Evaluation of microscopic tumor extension in non-small-cell lung cancer for three-dimensional conformal radiotherapy planning. Int J Radiat Oncol Biol Phys. 2000;48(4):1015–24.
Mimae T, Tsutani Y, Miyata Y, Yoshiya T, Ibuki Y, Kushitani K, et al. Role of lymphatic invasion in the prognosis of patients with clinical node-negative and pathologic node-positive lung adenocarcinoma. J Thorac Cardiovasc Surg. 2014;147(6):1820–6.
Scott AM. Current status of positron emission tomography in oncology. Intern Med J. 2001;31(1):27–36.
Hustinx R, Benard F, Alavi A. Whole-body FDG-PET imaging in the management of patients with cancer. Semin Nucl Med. 2002;32(1):35–46.
Flier JS, Mueckler MM, Usher P, Lodish HF. Elevated levels of glucose transport and transporter messenger RNA are induced by ras or src oncogenes. Science. 1987;235(4795):1492–5.
Monakhov NK, Neistadt EL, Shavlovskil MM, Shvartsman AL, Neifakh SA. Physicochemical properties and isoenzyme composition of hexokinase from normal and malignant human tissues. J Natl Cancer Inst. 1978;61(1):27–34.
Lv YL, Yuan DM, Wang K, Miao XH, Qian Q, Wei SZ, et al. Diagnostic performance of integrated positron emission tomography/computed tomography for mediastinal lymph node staging in non-small cell lung cancer: a bivariate systematic review and meta-analysis. J Thorac Oncol. 2011;6(8):1350–8.
Paul NS, Ley S, Metser U. Optimal imaging protocols for lung cancer staging: cT, PET, MR imaging, and the role of imaging. Radiol Clin North Am. 2012;50(5):935–49.
Agarwal M, Brahmanday G, Bajaj SK, Ravikrishnan KP, Wong CY. Revisiting the prognostic value of preoperative (18)F-fluoro-2-deoxyglucose ((18)F-FDG) positron emission tomography (PET) in early-stage (I & II) non-small cell lung cancers (NSCLC). Eur J Nucl Med Mol Imaging. 2010;37(4):691–8.
Goldstein NS, Mani A, Chmielewski G, Welsh R, Pursel S. Prognostic factors in T1 N0 M0 adenocarcinomas and bronchioloalveolar carcinomas of the lung. Am J Clin Pathol. 1999;112(3):391–402.
Yang F, Chen K, Liao Y, Li X, Sun K, Bao D, et al. Risk factors of recurrence for resected T1aN0M0 invasive lung adenocarcinoma: a clinicopathologic study of 177 patients. World J Surg Oncol. 2014;12:285.
Marom EM, McAdams HP, Erasmus JJ, Goodman PC, Culhane DK, Coleman RE, et al. Staging non-small cell lung cancer with whole-body PET. Radiology. 1999;212(3):803–9.
Garin E, Le Jeune F, Devillers A, Cuggia M, de Lajarte-Thirouard AS, Bouriel C, et al. Predictive value of 18F-FDG PET and somatostatin receptor scintigraphy in patients with metastatic endocrine tumors. J Nucl Med. 2009;50(6):858–64.
Kitagawa Y, Sano K, Nishizawa S, Nakamura M, Ogasawara T, Sadato N, et al. FDG-PET for prediction of tumour aggressiveness and response to intra-arterial chemotherapy and radiotherapy in head and neck cancer. Eur J Nucl Med Mol Imaging. 2003;30(1):63–71.
Paesmans M, Berghmans T, Dusart M, Garcia C, Hossein-Foucher C, Lafitte JJ, et al. Primary tumor standardized uptake value measured on fluorodeoxyglucose positron emission tomography is of prognostic value for survival in non-small cell lung cancer: update of a systematic review and meta-analysis by the European Lung Cancer Working Party for the International Association for the Study of Lung Cancer Staging Project. J Thorac Oncol. 2010;5(5):612–9.
Berghmans T, Dusart M, Paesmans M, Hossein-Foucher C, Buvat I, Castaigne C, et al. Primary tumor standardized uptake value (SUVmax) measured on fluorodeoxyglucose positron emission tomography (FDG-PET) is of prognostic value for survival in non-small cell lung cancer (NSCLC): a systematic review and meta-analysis (MA) by the European Lung Cancer Working Party for the IASLC Lung Cancer Staging Project. J Thorac Oncol. 2008;3(1):6–12.
Funai K, Sugimura H, Morita T, Shundo Y, Shimizu K, Shiiya N. Lymphatic vessel invasion is a significant prognostic indicator in stage IA lung adenocarcinoma. Ann Surg Oncol. 2011;18(10):2968–72.
Vaupel P, Briest S, Hockel M. Hypoxia in breast cancer: pathogenesis, characterization and biological/therapeutic implications. Wien Med Wochenschr. 2002;152(13–14):334–42.
Hockel M, Vaupel P. Tumor hypoxia: definitions and current clinical, biologic, and molecular aspects. J Natl Cancer Inst. 2001;93(4):266–76.
Higuchi M, Hasegawa T, Osugi J, Suzuki H, Gotoh M. Prognostic Impact of FDG-PET in surgically treated pathological stage i lung adenocarcinoma. Ann Thorac Cardiovasc Surg. 2014;20(3):185–91.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noda, Y., Goshima, S., Kanematsu, M. et al. F-18 FDG uptake on positron emission tomography as a predictor for lymphovascular invasion in patients with lung adenocarcinoma. Ann Nucl Med 30, 11–17 (2016). https://doi.org/10.1007/s12149-015-1023-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-015-1023-1