Abstract
Objective
The aim of this study was to evaluate the potential usefulness of 18F-FDG PET/CT for detecting colorectal carcinoma and adenoma in asymptomatic adults.
Methods
614 subjects were enrolled in this retrospective study. They underwent both 18F-FDG PET/CT and colonoscopy in the same day as part of a cancer-screening program. Small focal FDG accumulation along the colorectum on 18F-FDG PET/CT images were compared with colonoscopy findings. Size of lesion was measured on colonoscopy and histology was determined by biopsy or polypectomy.
Results
In 614 18F-FDG PET/CT images, 27 foci of FDG uptakes were observed in the colorectal area in 25 subjects. The overall sensitivity and specificity of 18F-FDG PET/CT were 5.6 and 96.8 %, respectively, but sensitivity to detect lesions larger than or equal to 1 cm was 25.8 %. On the ROC analysis, the optimal cut-off value for differentiating premalignant and malignant lesions from other benign conditions was 5.0 (sensitivity = 50 %, specificity = 88 %, AUC = 0.643).
Conclusions
Colonoscopic evaluation could be recommended by presence of focal colonic FDG uptake on 18F-FDG PET/CT, especially when SUVmax is over 5.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is one of the most common malignancies in Korea. Westernization of diet and an aging society are two major reasons for the ever-increasing incidence of colorectal cancer [1].
The concept that most colorectal carcinomas develop from preformed adenomatous polyp is widely accepted, which is referred to as adenoma–carcinoma sequence [2, 3]. It is well-known that only a minority of these adenomas undergoes malignant transformation, and it can take an average of approximately, 10 years for an adenoma, particularly one smaller than 1 cm in diameter, to transform into invasive cancer [3]. Therefore, the main targets of screening programs are adenomas with advanced pathologic features, i.e., high-grade dysplasia or early carcinoma. Detection and removal of adenomatous polyps are crucial for prevention and a potential cure. Colonoscopy is used to detect and remove adenomatous polyps.
Positron emission tomography (PET) using 2′-[18F] fluoro-2′-deoxy-d-glucose (FDG) is well-accepted in the imaging workup of various malignancies. PET is recognized as a useful tool to manage colorectal cancer and was shown to have an additional value in the detection of recurrent colorectal cancer [4, 5]. The introduction of FDG PET/CT has paved the way for anatomic information regarding FDG uptake. Accordingly, PET/CT has been carried out, even for health check-up, and some cases have been reported in which FDG colonic uptake revealed colonic adenomas or carcinomas [6–11].
This retrospective study was aimed to determine the usefulness of 18F-FDG PET/CT scans compared with colonoscopy for the evaluation of colorectal (pre-) malignancy, such as adenomas and carcinomas in asymptomatic adults.
Materials and methods
Patient selection
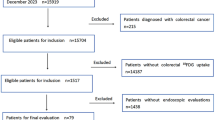
Subjects of this retrospective study were 614 asymptomatic adults (427 men, 187 women; mean age ± SD, 51.45 ± 7.65 years) who had undergone both 18F-FDG PET/CT and colonoscopy as part of our cancer-screening program between March 2010 and August 2011. Colonoscopy was performed after 18F-FDG PET/CT in the same day.
18F-FDG PET/CT imaging
The subjects fasted at least 6 h prior to the intravenous injection of 18F-FDG(0.12 mCi/kg). Blood glucose levels were checked in all subjects prior to the injection of 18F-FDG. A18F-FDG PET/CT was performed only when blood glucose levels did not exceed 150 mg/dL (8.3 mol/L). 18F-FDG PET/CT were acquired using Discovery LS PET/CT scanner (GE Medical Systems, Waukesha, WI). All studies were performed in three-dimensional mode with five to seven bed positions. The CT scan was performed immediately before the PET scan in the Discovery LS PET/CT scanner, using the multi-detector helical CT scanner. The imaging parameters were as follows: 140 kVp, 80 mA, 0.8 s per CT rotation, pitch of 6, and 22.5 mm/s table speed. The CT images were created in a matrix size of 512 × 512 but were reduced to a 128 × 128 matrix to correspond to the PET emission images. The emission data were acquired for 2.5 min in each bed position 60 min after the intravenous injection of 18F-FDG. The PET images were reconstructed using CT for attenuation correction with the OSEM algorithm (2 iterations, 16 subsets).
Colonoscopy
Experienced gastroenterologists in our total healthcare center performed all of the flexible endoscopic procedures. All abnormal colonic lesions were described and biopsied. The locations of the abnormal colonic lesions were classified into 6 segments: cecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. The size of the polyp or mass was measured and compared with the width of a forceps.
Imaging data analysis and correlation with colonoscopy
The 18F-FDG PET/CT images were reviewed by two experienced physicians in nuclear medicine. The readers analyzed the PET and fused images in both the axial and coronal planes without being informed of the endoscopic or surgical pathologic results. Any focal FDG uptake of colorectal area greater than what was seen in the normal hepatic parenchyma was considered intense focal bowel uptake. The attenuation-corrected PET component of the study was used to measure the maximum standardized uptake value (SUVmax) over the appropriate region of interest in the localized FDG activity. The specific localization of focal FDG activity in the colorectal area was compared to the site of endoscopic biopsy performed for histologic diagnosis. Contiguous diffuse FDG uptake in the intestine was not considered in this study because it is usually physiologic [12, 13].
In our study, the histopathologic diagnoses were grouped as primary carcinoma; premalignant lesions, which included adenoma with varying degrees of dysplasia; and benign lesions, such as hyperplastic polyps. A 18F-FDG PET/CT result was considered true-positive when a FDG focus and a colonoscopic or surgical abnormality were situated in the same location, and pathologic result of this lesion was adenocarcinoma or adenoma (Fig. 1). False-positive results included benign condition such as diverticulitis and physiologic bowel uptake, which was defined as focal FDG uptake without a matching colonoscopic abnormality. When a mucosal lesion of any size was detected at endoscopy with no corresponding focal FDG uptake, the 18F-FDG PET/CT result was interpreted as false-negative (Fig. 2).
Statistical analysis
FDG uptake of 18F-FDG PET/CT was analyzed for sensitivity, specificity, accuracy, and positive and negative predictive values. MedCalc Version 7 was used to determine the optimal cut-off values for differentiating (pre-) malignant lesions from other benign lesions on the ROC analysis. Comparison between true and false positive FDG uptake was analyzed by Student’s t test. Also, comparison between true positive lesions and false negative lesions on their size was analyzed by Student’s t test. A p value <0.05 was considered statistically significant.
Ethics statement
This study was performed after obtaining approval from the Institutional Review Board of Kangbuk Samsung Hospital (IRB No. KBC12004). This study was waived of informed consent from the board.
Results
614 asymptomatic adults (427 men, 187 women; mean age ± SD, 51.45 ± 7.65 years) had undergone both 18F-FDG PET/CT and colonoscopy in the same day. 435 of 614 subjects were negative on 18F-FDG PET/CT and colonoscopy. 154 out of 614 subjects (248 lesions: 170 tubular adenoma with low grade dysplasia, 51 hyperplastic polyp, 11 polypoid colonic mucosal tissue, 8 chronic non-specific colitis, 2 carcinoid tumor and 6 others, size: 0.49 ± 0.31 cm) were negative on 18F-FDG PET/CT and positive on colonoscopy. 25 out of 614 subjects (27 focal uptakes) were positive on 18F-FDG PET/CT. Results of the 25 subjects with positive finding of 18F-FDG PET/CT (27 focal uptakes) were summarized on Table 1. The number of true positive was 10 out of 27 focal uptakes (size: 1.8 ± 1.7 cm; 2 adenocarcinoma, 1 tubulovillous adenoma, 7 tubular adenoma with low grade dysplasia). The number of false positive was 17 out of 27 focal uptakes (15 physiologic bowel uptake, 2 diverticulitis). The mean size of colonoscopic lesions was larger in lesions with true positive uptake than those with false negative lesions (1.8 ± 1.7 vs. 0.49 ± 0.31 cm, p < 0.0001). The mean SUVmax of adenocarcinoma and adenoma were higher than those of physiologic bowel uptake and diverticulitis (8.3 ± 6.8 vs. 4.4 ± 1.6, p = 0.032).
Tables 2, 3, 4 and 5 compare the 18F-FDG PET/CT results with the findings of endoscopy. 18F-FDG PET/CT had sensitivity of 5.6 %, specificity of 96.8 % and accuracy of 73.6 %. The positive predictive value of 18F-FDG PET/CT was 37.0 %, and the negative predictive value, 75.1 %. But, in the lesions ≥1 cm, sensitivity, specificity and accuracy of 18F-FDG PET/CT were 25.8, 96.8 and 92.9 %, respectively. The positive predictive value of 18F-FDG PET/CT was 32.0 %, and the negative predictive value, 95.7 %. In the lesions <1 cm, sensitivity, specificity and accuracy of 18F-FDG PET/CT were 1.3, 96.8 and 68.5 %, respectively. The positive predictive value of 18F-FDG PET/CT was 10.5 %, and the negative predictive value, 77.7 %.
On the ROC analysis, the optimal cut-off values for differentiating (pre-) malignant lesions from other benign lesions was SUVmax > 5.0 (sensitivity = 50 %, specificity = 88 %, AUC = 0.643, 95 % Confidence Interval 0.429–0.823, Fig. 3).
Discussion
The purpose of this retrospective study was to evaluate the potential usefulness of 18F-FDG PET/CT compared with colonoscopy for detecting colonic (pre-) malignancy, such as adenomas and carcinomas in asymptomatic adults.
The overall sensitivity and specificity of 18F-FDG PET/CT for detecting colonic carcinoma and adenoma were 5.6 and 96.8 %, respectively. Although overall sensitivity was very low, all of carcinoma (n = 2) and tubulovillous adenoma (n = 1), and 7 of 184 tubular adenoma with low grade dysplasia were detected on FDG PET/CT. Also, in the lesions ≥1 cm, sensitivity of 18F-FDG PET/CT increased by 25.8 %.
Unlike our study, several previous studies revealed that the sensitivity of FDG PET for detecting (pre-) malignancy was 37–56 % [7–10]. Colon adenoma size and dysplasia grade have been reported to correlate with likelihood of detection by PET/CT [6, 9, 14]. When our colonoscopic and pathologic results (size and pathologic grade of polyps) were compared with previous studies, our study had smaller size and lower grade than those of previous studies. In our study, 154 out of 614 subjects (248 lesions: 170: tubular adenoma with low grade dysplasia, 51 hyperplastic polyp, 11 polypoid colonic mucosal tissue, 8 chronic non-specific colitis, 2 carcinoid tumor and 6 others, size: 0.49 ± 0.31 cm) were negative on FDG PET/CT, and these lesions consisted of 196 small size polyps (≤0.5 cm), 34 medium size polyps (0.6–0.9 cm) and 36 large polyps (≥1 cm). Because of these factors, we think that the sensitivity of FDG PET for detecting (pre-) malignancy in our study was lower than that of previous studies.
A correlation between SUVmax and colon neoplasm histology has not been demonstrated consistently. Although Gutman et al. [8] and Chen et al. [15] found that mean SUVs increased with higher grades of dysplasia with highest levels in patients with colon cancers, Israel et al. [7] did not observe such a progression in SUV values. In our study, the mean SUVmax of adenocarcinoma and adenoma were higher than those of physiologic bowel uptake and diverticulitis (8.3 ± 6.8 vs. 4.4 ± 1.6, p = 0.032). Especially, the mean SUVmax of adenocarcinoma plus tubulovillous adenoma were significantly higher than those of adenoma with lower grade dysplasia (p = 0.012, Fig. 4), and of physiologic bowel uptake and diverticulitis (p < 0.0001, Fig. 4). But, there was an overlap of FDG uptake between (pre-) malignancy and benign condition, and there was no significant difference of SUVmax between adenoma with lower grade dysplasia and physiologic uptake (p = 0.387, Fig. 4). It seems that mean SUVmax is not effective for differentiating between (pre-) malignancy and benign condition, because they all demonstrate increased FDG activity. Therefore, it seems that 18F-FDG PET/CT will never completely replace colonoscopy for screening of colorectal (pre-) malignancy.
The mean SUVmax of adenocarcinoma plus tubulovillous adenoma were significantly higher than those of adenoma with lower grade dysplasia (p = 0.012), and of physiologic bowel uptake and diverticulitis (p < 0.0001). There was no significant difference of SUVmax between adenoma with lower grade dysplasia and physiologic uptake (p = 0.387)
However, incidental colonic FDG uptake is not infrequent finding encountered during 18F-FDG PET/CT. Although the sensitivity of 18F-FDG PET/CT detecting (pre-) malignancy is low, we think that incidental colonic FDG uptake has clinical significance. Therefore, we think that one way improving the sensitivity of 18F-FDG PET/CT detecting (pre-) malignancy is using the standardized PET cut-off value. Luboldt et al. [16] found that a standardized PET cut-off (e.g. SUVmax ≥ 5) improved the accuracy of differentiating (pre-) malignancy and benign condition. In our study, the optimal cut-off values for differentiating (pre-) malignant lesion from other benign condition was 5.0 (sensitivity = 50 %, specificity = 88 %, AUC = 0.643).
In conclusion, colonoscopic evaluation could be recommended by presence of focal colonic FDG uptake on 18F-FDG PET/CT, especially when SUVmax is over 5.
References
Kim DH. Risk factors of colorectal cancer. J Korean Soc Coloproctol. 2009;25:356–62.
Muto T, Bussey HJ, Morson BC. The evolution of cancer of the colon and rectum. Cancer. 1975;36:2251–70.
Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology. 1997;112:594–642.
Choi EK, Yoo IR, Park HL, Choi HS, Han EJ, Kim SH, et al. Value of surveillance 18F-FDG PET/CT in colorectal cancer: comparison with Conventional Imaging Studies. Nucl Med Mol Imaging. 2012;46:189–95.
Yoon HJ, Lee JJ, Kim YK, Kim SE. FDG-PET/CT is superior to enhanced CT in detecting recurrent subcentimeter lesions in the abdominopelvic cavity in colorectal cancer. Nucl Med Mol Imaging. 2011;45:132–8.
Yasuda S, Fujii H, Nakahara T, Nishiumi N, Takahashi W, Ide M, et al. 18F-FDG PET detection of colonic adenomas. J Nucl Med. 2001;42:989–92.
Israel O, Yefremov N, Bar-Shalom R, Frenkel A, Kagana O, Keidar Z, et al. PET/CT detection of unexpected gastrointestinal foci of 18F-FDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med. 2005;46:758–62.
Gutman F, Alberini JL, Wartski M, Vilain D, Le Stanc E, Sarandi F, et al. Incidental colonic focal lesions detected by FDG PET/CT. AJR. 2005;185:495–500.
Nakajo M, Jinnouchi S, Tashiro Y, Shirahama H, Sato E, Koriyama C, et al. Effect of clinicopathologic factors on visibility of colorectal polyps with FDG PET. AJR. 2009;192:754–60.
Kei PL, Vikram R, Yeung HW, Stroehlein JR, Macapinlac HA. Incidental finding of focal FDG uptake in the bowel during PET/CT: cT features and correlation with histopathologic results. AJR. 2010;194:401–6.
Chung DS, Kang S, Park JB. Incidental finding of appendiceal adenocarcinoma in F-18 FDG PET/CT for health screening. Nucl Med Mol Imaging. 2012;46:306–10.
Tatlidil R, Jadvar H, Bading JR, Conti PS. Incidental colonic fluorodeoxyglucose uptake: correlation with colonoscopic and histopathologic findings. Radiology. 2002;224:783–7.
Pai MS, Cho YK, Jung SA, Shim KN, Lee HS. Colonic uptake patterns of F-18-FDG PET in asymptomatic adults: comparison with colonoscopic findings. Nucl Med Mol Imaging. 2005;39:15–20.
van Kouwen MC, Nagengast FM, Jansen JB, Oyen WJ, Drenth JP. 2-(18F)-fluoro-2-deoxy-d-glucose Positron emission tomography detects clinical relevant adenomas of the colon: a Prospective Study. J ClinOncol. 2005;23:3713–7.
Chen YK, Kao CH, Liao AC, Shen YY, Su CT. Colorectal cancer screening in asymptomatic adults: the role of FDG PET scan. Anticancer Res. 2003;23:4357–61.
Luboldt W, Volker T, Wiedemann B, Zöphel K, Wehrmann U, Koch A, et al. Detection of relevant colonic neoplasms with PET/CT: promising accuracy with minimal CT dose and a standardized PET cut-off. EurRadiol. 2010;20:2274–85.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hwang, J.P., Woo, SK., Yoon, S.Y. et al. The potential usefulness of 18F-FDG PET/CT for detecting colorectal carcinoma and adenoma in asymptomatic adults. Ann Nucl Med 29, 157–163 (2015). https://doi.org/10.1007/s12149-014-0922-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-014-0922-x