Abstract
This study aimed to examine the stability of depression subtypes over time or the multiple factors and mechanisms that influence these subtypes. Data from two waves of the China Health and Retirement Longitudinal Study (CHARLS) for 2013 (T1) and 2018 (T2), separated by 5 years were included in latent class analysis (LCA) and latent transition analysis (LTA). Specifically, scores on the 10-item Chinese version of the Centre for Epidemiological Studies Depression Scale (CES-D-10) of 2,828 Chinese individuals aged 60 years and older were analyzed. Older Chinese adults were categorized into three classes based on depressive symptoms: the severe depressive symptoms, the mild depressive symptoms, and transition groups. At T2, 70.4% of participants reported severe depressive symptoms, 62.1% reported mild depressive symptoms, and 49.2% were placed in the transition group. Patients in the severe depressive symptoms and mild depressive symptoms tended to switch to the transition group over time, with probabilities of 21.1% and 28.2%, respectively. Further analysis showed that sex, place of residence, marital status, ability to perform activities of daily living (ADLs), self-rated health status, and life satisfaction significantly predicted this transition. This study demonstrated a transition pattern of depressive symptoms in Chinese older adults. We should pay more attention to key elderly groups such as unmarried women, alcohol consumption, and poor self-rated health, rationally plan mental health resources, and establish a dynamic tracking service system to prevent the depression and related adverse consequences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Data from the “2019 WHO Statistical Report” revealed that there were more than 350 million people with depression worldwide (Herrman et al., 2022), and the prevalence of depression is especially high in the elderly population; furthermore, the global prevalence of depressive symptoms is as high as 28.4% (Hua et al., 2015; Wang et al., 2020). In China, the older adults with depressive symptoms but not meeting the diagnostic criteria for clinical depression is much larger, with reported prevalence rates ranging from 20.0% to 33.0% (Li et al., 2014; Tang et al., 2021; Zhang et al., 2012), depressive symptoms is often accompanied by psychological symptoms such as anxiety, compulsion, and fear, is a potential risk factor for suicidal behavior, which not only increases the mortality of older adults but also results in high medical costs of US $426,700 per capita per year (Hsieh & Qin, 2018). Therefore, given increasing population aging in China, research has focused on maintaining and promoting the physical and psychological health of older adults, implementing early preventive interventions, reducing the occurrence of depressive symptoms, and thereby improving their quality of life (Hu et al., 2022a, b; Moreno-Agostino et al., 2021).
Current situation of cross-sectional data study on depressive symptoms in population
Some of the existing findings, such as Petkus, AJ have found that genetic factors play a greater part in the association between depressive symptoms and physical illness for men than in women. For both sexes, across all ages, physical illness can equally trigger social and health limitations that contribute to depressive symptoms (Petkus et al., 2017). Fan, XW found that the prevalence of depressive symptoms was high among middle-aged and elderly people in China, and subjective quality of life evaluation, health status and marital status were the main factors affecting depressive symptoms (Fan et al., 2021). In addition, Yuan, L, Fu, C, Sun, F and other scholars also found similar results (Fu et al., 2023; Sun et al., 2020; Yuan et al., 2023). These studies on depressive symptoms have used standardized scales, and the severity of depressive symptoms in subjects was determined according to a standardized threshold and used to divide individuals into groups (Kong et al., 2018; Zhao B & C., 2018). However, this process ignores individuals with similar overall scores who may have completely different response patterns on the scale items. These patterns reflect qualitative differences among individuals, resulting in a high degree of heterogeneity within the categorized groups. Studies have shown that the viewing that depression as a homogeneous entity may be an important cause of treatment failure; that is, ignoring the potential phenotypes of depressed people and applying a "one-size-fits-all" approach to treatment may lead to increased severity of depression in the population(Catarino et al., 2022).
Current status of longitudinal data on depressive symptoms in population
The dynamic change of depressive symptoms over time has been confirmed by many longitudinal studies. For example, Li, C defined four heterogeneous depressive symptom trajectories in Chinese adults: stable-low, high-decreasing, high-stable, and low-increasing, and found that gender, education, income, and self-reported health status were associated with the trajectories(Li et al., 2023). A melancholy subtype and an atypical subtype were identified in both T0 and T1, in a sample of elderly depression in the Netherlands. The melancholic subtype was characterized by decreased appetite and weight and had a stability of 0.86. The atypical subtype was characterized by increased appetite and weight, had a stability of 0.93, although the discriminating power of different symptoms had decreased at T1 (Veltman et al., 2020). The older adults in the United States have identified four underlying depressive symptoms: multiple symptoms, depressed mood, fatigue, and minimal symptoms. Most residents remained in the same status from admission to 90 days (Yuan et al., 2021). In addition, He, RJ, Lamers, Torre-Luque and others also found similar results (He et al., 2023; Lamers et al., 2012; Torre-Luque et al., 2020). However, to our knowledge, few LTA studies in recent years have been conducted in the population of older Chinese adults with depressive symptoms. According to previous studies, there are likely different subtypes of depressive symptoms in the older adult population in China. Moreover, the number of older Chinese adults is increasing, and the number of depressed people is increasing each year, which may lead to differences in depressive symptoms in older adults and different transition patterns.
Summary and hypotheses
In conclusion, this study adopted a longitudinal design and analyzed two waves of survey data (separated by 5 years) collected from older Chinese adults to explore the evolution of depressive symptoms. It is possible to estimate individual changes in latent states at different time points and assesses the stages of individual development from the perspective of transition probabilities, enabling the examination of longitudinal latent classes (Hu et al., 2022a, b; Lenferink et al., 2022). The following hypothesis was proposed. Based on previous research, we expected to identify three to four latent classes (as the optimal number of latent classes) based on data from T1 and T2(Rodgers et al., 2014; Ulbricht et al., 2018a, b; Ulbricht et al., 2018a, b). Among these latent classes, we expected that individuals in the group with mild depressive symptoms would show greater stability, while individuals in the transition and severe depressive symptoms groups would be more prone to switching among groups(Lamers et al., 2012; Ni et al., 2017; Tay et al., 2017). In addition, given that many studies have explored the factors influencing depressive symptoms, we further explored not only the factors influencing each latent class but also the factors that affect the transition among latent states in older Chinese individuals to help design targeted interventions to improve depressive symptoms in Chinese older adults.
Methods
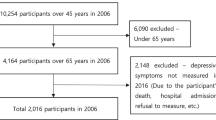
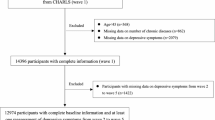
Sample
The sample data were extracted from the China Health and Retirement Longitudinal Study (CHARLS) project database, which includes high-quality microdata representing families and individuals aged 45 years and above in China; the CHARLS aimed to analyze the problem of population aging. The CHARLS baseline survey was conducted in 2011, followed by surveys in 2013, 2015 and 2018, with surveys administered in 28 provinces across the country (Zhao et al., 2014). Due to the short interval between 2015 with the other two time points and the serious data missing phenomenon of incorporating three time points together. Therefore, to study the changes in depressive symptoms among older Chinese adults in recent years and to better estimate the changes in the latent state of individuals at different time points, this study selected data from waves in 2013 (T1) and 2018 (T2) to explore the transformation of depressive symptoms and the factors influencing the transformation of depressive symptoms among older Chinese individuals. The samples were selected according to the following criteria: The subjects were elderly, and T1 was 60 years old and above; Complete data on T1 and T2 depressive symptoms assessments; Samples with missing values on the study variables are excluded. A total of 2828 valid samples were obtained.
The average age of the 2,828 respondents was 65.60 years (SD: 4.93; range: 60 to 93). Of the respondents, 1,638 (57.9%) were female, 1,499 (53.0%) did not receive a formal education, 2,420 (85.6%) were married, 2,144 (75.8%) were rural residents, 477 (16.9%) were drinkers, 858 (30.3%) were smokers, 1,625 (57.5%) slept less than 7 h per night, 2,303 (81.4%) had received financial support from their children, 1,501 (53.1%) participated in social activities, 1,210 (42.8%) lived with their children, and 551 (19.5%) had limited ability to perform ADLs. The average self-rated health and life satisfaction scores were 2.15 (SD: 0.880) and 3.18 (SD: 0.729), respectively.
Measurements
Depressive symptoms
Depressive symptoms were measured with the 10-item Chinese version of the Centre for Epidemiological Studies Depression Scale (CES-D-10) (Zheng et al., 2022), which includes three sections: somatic symptoms, depressive symptoms, and positive affect (Guarnaccia et al., 1989; Yen et al., 2000). It has good validity in various age groups in China and exhibits measurement invariance across genders in adult samples (Ren et al., 2019). The CES-D-10 contains 10 items with four response options. Participants report the frequency of depressive symptoms experienced in the past week on a scale ranging from 0 = "rarely (less than one day)" to 3 = "most of the time (5–7 days)" (Knoll et al., 2007). According to the scoring criteria, a CES-D-10 total score ≥ 1 is the cutoff value for depressive symptoms. Two items of positive affect are reverse scored: Item 5 (“I felt hopeful about the future”) and Item 8 (“I was happy”). For LCA, the "rarely (less than one day)" option was coded as 0, representing the absence of depressive symptoms, and the other three options were coded as 1, representing the presence of depressive symptoms.
Covariates
The included sociodemographic characteristics were as follows: (1) sex (male/female), (2) education level (no formal education/primary school/middle school/high school or above), and (3) place of residence (urban/rural). Health and behavioral habits were assessed and included the following: (1) activities of daily living (ADLs), measured with Katz scale: the ability of older individuals to take care of themselves in daily life, including bathing, dressing, going to the toilet, controlling defecation and urination, getting into and out of bed, and feeding themselves(those who cannot complete any one of these six daily activities independently were defined as disabled) (Katz et al., 1963); (2) alcohol consumption (no/yes); (3) smoking status (not a past/current smoker or past/current smoker); (4) sleep (< 7 h/ ≥ 7 h): according to the Healthy China Initiative (2019–2030), sufficient sleep was defined as ≥ 7 h per night, and insufficient sleep was defined as < 7 h per night (Zheng et al., 2022); and (5) self-rated health status (measured with a single item, "How do you rate your health?" with five response options: excellent, very good, good, fair, and poor. We set the health dummy variable to 1 when the response options were “excellent”, “very good”, and “good” or 0 when the response options were “fair” and “poor”). The family factors included (1) marital status (married/other); (2) economic support from children (yes/no); and (3) living with children (yes/no). The sociological factors included (1) social activities (yes/no) and (2) life satisfaction (measured with a single item, "How satisfied are you with your life?”, with five response options: completely satisfied, very satisfied, somewhat satisfied, not very satisfied and not at all satisfied. We set the life satisfaction dummy variable to 1 when the response options were “extremely satisfied”, “very satisfied”, and “somewhat satisfied”. Otherwise, the value was 0).
Statistical analyses
LTA was performed using Mplus 8.4. The first step of analysis was to conduct separate LCAs for the measurements at T1 and T2, which were separated by 5 years, to evaluate the number of classes at each time point. Based on previous LCA and LTA studies, the CES-D score (treated as a dichotomous variable: presence/absence of depressive symptoms) was set as an explicit response indicator, and models with 1 to 5 classes were investigated. The latent class variables were assumed to explain a series of observed associations within depression (Liao & Lian, 2020). In this study, two sets of parameters were estimated: (1) latent class probability and (2) conditional probability, that is, the estimated probability of the observed variable when the individual belonged to a particular class. The fitting indices of the model with the optimal class solution were as follows: the Akaike information criterion (AIC), Bayesian information criterion (BIC), adjusted BIC (aBIC), entropy, Lo–Mendell–Rubin likelihood ratio test (LMR), and bootstrap likelihood ratio test (BLRT). Among them, smaller AIC, BIC and aBIC values correspond to a better model fit (Luo et al., 2023). Entropy is an indicator used to evaluate the classification accuracy, ranging from 0 to 1, and values ≥ 0.8 indicates that the classification accuracy is greater than 90%. The LMR and BLRT were used to compare the fit of the K-1 and K-class models (Luo et al., 2023; Ying et al., 2021). The p values were significant, indicating that the fitting results of the K class models were better than those of the K-1 class models (Lubke & Muthen, 2007; Nylund et al., 2007). In addition, simplicity and interpretability were considered when determining the best fitting model.
Next, LTA was used to estimate the changes between individual latent states at different time points using the transition matrix, and state probability was used to determine the transition probabilities of individuals (Collins & Wugalter, 1992). LTA expands on LCA because it uses longitudinal data, with the advantages of LCA in managing class variables and the advantages of longitudinal analysis methods allowing exploration of developmental trends. The model estimated latent state transition probabilities, estimating class changes and stability, and described patterns of depressive symptoms changes in older Chinese individuals over five years.
Finally, after participants were assigned to the most likely class according to their posterior probability, SAS 9.4 was used to evaluate the baseline factors associated with stable subtypes in univariate and multivariate analyses including sociodemographic characteristics, health and behavioral habits, family factors, and sociological factors as independent variables and latent change types of depressive symptoms as dependent variables. An unordered multicategory logistic regression was performed.
Results
Common method bias
Common method bias test was assessed with Harman’s one-factor test, and all items measured at the two time points were analyzed by principal component analysis without rotation. The results showed that at T1, two common factors with eigenvalues greater than one were extracted, and the first common factors explained 33.86% of the variation. At T2, two common factors had eigenvalues greater than one, and the first explained 38.21% of the total variation. More than one common factor was extracted at both time points, and the variance explained by the first common factor was less than the critical standard (40.0%), suggesting that our results were not affected by common method bias.
Identification of the number of latent classes of depressive symptoms in elderly Chinese individuals
Table 1 presents the fit indicators of latent class models with different numbers of classes of depressive symptoms in older Chinese individuals at T1 and T2. The AIC, BIC, and aBIC values gradually decreased with an increasing number of classes, reaching the lowest value in the five-class model. However, the entropy values of the five-class model at T1 and T2 were not optimal, and the LMR(P) values were greater than 0.05(i.e., not significant), indicating that the five-class model was not ideal. Although the four-class model had adequate entropy values at T1, showing high classification accuracy, heterogeneity within classes was reduced as classes were added (Ni et al., 2017). Given the consistency of models at the two time points and simplicity, the three-class model was chosen (Ni et al., 2017). With the three-class model, the P values of LMR and BLRT at T1 and T2 were significant (P < 0.001) and significantly better than those of the two-class model; the entropy values were all > 0.70, indicating that the three-class model had the best fit to the data. The depressive symptoms of older Chinese individuals showed consistent modeling at the two time points separated by five years.
Results of the latent class and transition model for depressive symptoms among older Chinese adults
Figure 1 shows the item-response probabilities that jointly characterized the three different depressive states in older Chinese adults at T1 and T2. Given the conditional probabilities of each CES-D-10 item in the three classes at T1 and T2, the severity of depressive symptoms nomenclature was used to name the groups: the severe depressive symptoms, mild depressive symptoms and transition group. In the severe depressive symptoms group, more than 70% of individuals reported experiencing eight CES-D-10 items, and the proportion of subjects in this group increased slightly over time, with values at T1 and T2 of 14.85% and 22.84%, respectively. The incidence of depressive symptoms was lowest in the mild depressive group among the three groups. In this group, less than 20% of individuals reported experiencing 7 CES-D-10 items, and less than 10% of individuals reported experiencing 5 CES-D-10 items. The proportion of subjects in mild depressive symptoms decreased over time, from 45.79% at T1 to 40.98% at T2. The overall probabilities of depressive symptoms in the transition group was between those of the other two groups. The proportion of participants in this group decreased slightly over time, from 39.36% at T1 to 36.17% at T2.
Table 2 shows the prevalence of each type of depressive symptoms at T1 and T2. The reference was the mild depressive symptoms; at T1, this group accounted for 45.79% of the participants, and at T2, this group accounted for 40.98% of participants. The second part of Table 2 shows the LTA results, revealing the changes in the membership of these three groups at the two time points. The stability of severe depressive symptoms was higher; the probability of remaining in the severe depressive symptoms (i.e., categorized into the severe depressive symptoms at T1 and T2) was 70.4%, while the probabilities of remaining in the mild depressive symptoms and transitioning groups were 62.1% and 49.2%, respectively. Both individuals with severe depressive symptoms and those with mild depressive symptoms tended to switch to the transition group over time, with transition probabilities of 26.1% and 24.7%, respectively. Individuals in the transition group tended to switch to the severe depressive symptoms, with a transition probability of 21.1%.
Factors influencing depressive symptoms in older Chinese adults
Next, multinomial logistic regression analysis was conducted with three classes of depressive symptoms as the dependent variables and sociodemographic characteristics, health and behavioral habits, family factors and sociological factors as covariates in the latent class models. The reference category of the latent state at baseline (T1) was the mild depressive symptoms, and the ratio of changes in the probability that subjects belonging to the severe depressive symptoms (i.e., the odds ratio) under the influence of covariates was obtained. As shown in Table 3, male sex, urban residence, being married, sleep duration ≥ 7 h, and ability to perform ADLs alleviated depressive symptoms in older Chinese adults.
To explore the influence of related factors on depressive symptoms in older individuals in China, their influence on the likelihood of transitioning between groups was further explored. The subjects who remained in their original group were used as the reference group, and the odds ratios of switching to other groups were calculated (Hu et al., 2022a, b). As shown in Table 4, the odds of male subjects and urban residents switching from the mild depressive symptoms to severe depressive symptoms were higher, and the probability of urban residents switching from the transition group to the severe depressive symptoms were also higher. Married subjects were more likely to change from the transition group to the mild depressive symptoms. The probabilities of drinkers switching from the mild depressive symptoms to the severe depressive symptoms and from the transition group to the severe depressive symptoms were higher and lower, respectively. The probability of the subjects with poor self-rated health switching from the mild depressive symptoms to the transition group and from the severe depressive symptoms to the mild depressive symptoms were higher and lower, respectively. In addition, the probabilities of switching from the severe depressive symptoms to the mild depressive symptoms and from the severe depressive symptoms to the transition group were lower among participants with a limited ability to perform ADLs.
Discussion
In this study, LCA and LTA were used to analyze the latent characteristics and transition patterns of depressive symptoms profiles among older Chinese adults during 2013–2018. The model had good fit, indicating substantial heterogeneity in depressive symptoms among older Chinese adults in this study. We identified three subtypes of depressive symptoms: the mild depressive symptoms, transition group, and severe depressive symptoms(Baert et al., 2010). All three subtypes of depressive symptoms showed high stability from T1 to T2, with the severe depressive symptoms exhibiting the greatest stability. Additionally, different transition probabilities were observed among the different subtypes of depressive symptoms. Individuals in the severe depressive symptoms and mild depressive symptoms tended to switch to the transition group, while those in the transition group tended to switch to the severe depressive symptoms (Hu et al., 2022a, b). Multivariate regression analyses revealed that sex, place of residence, marital status, alcohol consumption, ADL scores, self-rated health, and life satisfaction all predicted the occurrence of depressive symptoms and changes over time among older individuals in China.
Consistent with the hypothesis and previously published studies, we found that depressive symptom profiles among older individuals in China could be divided into three obvious classes at both T1 and T2 (Collins & Wugalter, 1992). In terms of proportion of subjects in the mild depressive symptoms, that at T2 was 4.81% lower than that at T1. Studies have shown that older individuals with mild depressive symptoms mainly show emotional problems, such as ease of crying, loss of appetite and fatigue. According to the scale standard, the recognition rate of depressive symptoms is low. These symptoms are easy to overlook, but persistent pessimism may gradually escalate into depression (Wang et al., 2018). Therefore, compared with traditional depressive symptoms analysis results, the present study’s results can not only be used to identify depressed older individuals but also help screen older individuals for depression to provide more targeted preventive interventions. The latent state probabilities of the transition group at T1 and T2 were 39.36% and 36.17%, respectively. Persistent negative emotions will gradually escalate over time, resulting in severe depressive symptoms; however, if individuals receive good guidance, symptoms are likely to abate (Wang et al., 2018). Therefore, we should monitor this population to prevent the accumulation and aggravation of negative emotions. The proportion of the latent state in the severe depressive symptoms increased by 7.99% between T1 and T2. The physiological function of older individuals gradually declines, leading to a gradual increase in disappointment, resulting in more severe depression (Zhang et al., 2019). For these people, mental health education should be provided, and psychological interventions should be implemented to lead these individuals to increase the acceptance of aging, thereby reducing their severity of depression.
According to the LTA, the severe depressive symptoms had the greatest stability: the probability of remaining in this group five years later was as high as 70.4%, which is higher than the critical value (50%) for stability used by other scholars (Geiser et al., 2006; Kleinjan et al., 2010). The mild depressive symptoms and the transition group also showed moderate stability, and the probability of remaining in the same group between T1 and T2 was close to or higher than 50%, which is also consistent with previous research results and supported our hypothesis (Lamers et al., 2012; Rodgers et al., 2014). According to Beck's cognitive model of depression, the root of depressive symptoms is the irrational cognitive schema that is formed in the early stage. If the schema is not broken or reconstructed, it will continue to interact with stress, resulting in the maintenance of the depressive state (Liao & Lian, 2020; Zheng et al., 2022). In LTA, we observed transitions among subtypes of depressive symptoms. Notably, individuals in the severe depressive symptoms and mild depressive symptoms groups tended to switch to the transition group (with probabilities of 21.1% and 28.2%, respectively), and those in the transition group tended to switch to the severe depressive symptoms, with a probability of 26.1%. In general, people in the severe depressive symptoms had the most significant difficulty with self-relief symptoms, and those in the transition group had a greater probability of worsening depressive symptoms, which may indicate that endogenous or depressive symptoms become increasingly serious with age (Parker et al., 2001). This reminds us once again that once depressive symptoms in older individuals reach a certain level, alleviating them naturally is difficult.
The Healthy China Initiative (2019–2030) noted that the prevalence rates of mood disorders, especially depressive disorders, has been increasing in China in recent years (Zheng et al., 2022). One of the main goals of mental health promotion actions is to slow the increase in depression prevalence (Liao & Lian, 2020). To validate empirical classifications, most previous studies have further explored differences in symptomatology, demographics characteristics, and comorbidities among subtypes of depressive symptoms (Wang et al., 2018). The present study also examined the transitions among subtypes of depressive symptoms and the factors influencing these transitions. We found that female sex, rural residence, being unmarried, lack of sleep, inability to perform ADLs, poor self-rated health status, and low life satisfaction can worsen depressive symptoms, which is consistent with previous studies (Liao & Lian, 2020; Ni et al., 2017). A person-centered perspective can identify high-risk individuals who need targeted and adaptive interventions, improve management to guide clinical diagnostic practices, and facilitate the design of targeted interventions. In future work, targeted interventions should be carried out according to subtypes of depressive symptoms in older individuals to explore new ways to enhance the well-being of older individuals, reduce the occurrence and development of negative emotions, strengthen their sense of identity, and improve their behavioral lifestyle, thus reducing the occurrence and development of depression. This can help millions of older people to become healthier, happier and more active members of society; help revitalize China's economy; and contribute to the achievement of the United Nations 2030 Sustainable Development Goals (Ni et al., 2017).
Longitudinal analysis showed that older individuals who were females, rural residents, nonmarried, drinkers, had limited ADLs and had poor self-rated health status had the most unstable depressive symptoms over time. This suggests that these populations may be risk groups for depression. Women generally have a longer life expectancy and a higher rate of widowhood than men. In the short term, these older individuals may have difficulty adjusting to changes with aging and declining interactions with their children (Hong et al., 2022). Unmarried older individuals experience more stressful life events and experience greater loneliness, which may damage personal happiness and trigger or aggravate depressive symptoms (Guo et al., 2017). Furthermore, previous studies have found that alcohol abuse increases the risk of depressive symptoms through mediating behaviors. The results of this study further support this point, suggesting that people with depression use alcohol as self-medication or as a means to reduce negative emotions (Chichetto et al., 2019). Consistent with previous findings, physical health was another critical factor affecting depressive symptoms among older people in this study (Chen et al., 2012). In the Chinese culture, older people are often regarded as dependent on their families, even as a burden, especially when their physical health decreases with age, and the frustration and disappointments caused by the loss of social roles undermine the life satisfaction and self-esteem of older individuals. This reduces their self-reported health, social participation and likelihood of talking to individuals when encountering problems. These factors also highlight the loneliness and helplessness of older individuals (Li et al., 2014). Therefore, interventions to address depression in older individuals should include efforts to restore their sense of self-efficacy in the family context and change the power relationship within the Chinese family (Guo et al., 2017).
Regarding depressive symptoms in the older population, we did not find associations with smoking, social interactions, or family factors (such as economic support and living with their children) in this study. The reasons may be as follows: the inclusion of only two waves of data (from 2013 and 2018), differences in views of mental health problems, differences in definitions of depressive symptoms, and differences in the screening tools used (Krishnamoorthy et al., 2020). The strength of this study is that most previous research on depression in older individuals has focused on people with a clinical diagnosis of depression, and less attention has been directed toward nonclinical populations with depressive symptoms (Abdoli et al., 2022; Hu et al., 2022a, b). Thus, this study is the first in recent years to conduct LTA of depressive symptoms in a nonclinical population with older Chinese individuals and to consider the impact of sociodemographic characteristics, health and behavioral habits, family factors, and sociological factors on depressive symptoms in older Chinese adults. Differences among these symptoms were particularly pronounced in the first-identified data-driven subtypes; therefore, these data can be compared with data from several studies carried out in younger and older Chinese individuals. One of the important limitations of this study is that depression measures were self-reported, which may lead to underestimation of depressive symptoms and biased responses. Second, our model used only the CES-D-10 scale to measure depressive symptoms. However, previous studies, both cross-sectional and those including more depressive symptoms, have reported subgroups similar to those found in this study, indicating that adding more symptoms to the model does not necessarily change the outcomes. Therefore, although this study used only a single scale, it also identified relatively stable subtypes. Third, in this study, only a small proportion of older Chinese individuals exhibited a transition in depressive symptoms, which limits our ability to access the impact of interventions to some extent (Ni et al., 2017).
Conclusion
Our findings showed that the severe depressive symptoms had the highest risk and exhibited considerable stability, representing the target population for preventing the transition to clinical depression and for reducing negative events caused by extreme emotions in individuals. The next step should be to develop a dynamic tracking system. For individuals in the mild depressive symptoms and transition groups, interventions should focus on preventing the progression of symptoms. Given the current situation, where social and psychological service resources are in short supply, along with the factors influencing latent class transition, we suggest that focusing on rural women who are not married, consume alcohol, have limited ability to perform ADLs, have poor self-rated health, and have low life satisfaction could improve the effectiveness of depression prevention and management. Exploring dynamic changes in depression subtypes provides more possibilities for future hierarchical treatment interventions aimed at improving the outcomes of older Chinese individuals with depressive symptoms (Catarino et al., 2022).
Data availability
Data from this study are available at the public website: https://charls.charlsdata.com.
References
Abdoli, N., Salari, N., Darvishi, N., Jafarpour, S., Solaymani, M., Mohammadi, M., & Shohaimi, S. (2022). The global prevalence of major depressive disorder (MDD) among the elderly: A systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews, 132, 1067–1073. https://doi.org/10.1016/j.neubiorev.2021.10.041
Baert, S., De Raedt, R., & Koster, E. H. W. (2010). Depression-related attentional bias: The influence of symptom severity and symptom specificity. Cognition & Emotion, 24(6), 1044–1052. https://doi.org/10.1080/02699930903043461
Catarino, A., Fawcett, J. M., Ewbank, M. P., Bateup, S., Cummins, R., Tablan, V., & Blackwell, A. D. (2022). Refining our understanding of depressive states and state transitions in response to cognitive behavioural therapy using latent Markov modelling. Psychological Medicine, 52(2), 332–341. https://doi.org/10.1017/S0033291720002032
Chen, Y., Hicks, A., & While, A. E. (2012). Depression and related factors in older people in China: A systematic review. Reviews in Clinical Gerontology, 22(1), 52–67. https://doi.org/10.1017/S0959259811000219
Chichetto, N. E., Kundu, S., & Freiberg, M. S. (2019). Association of Syndemic Unhealthy Alcohol Use, Cigarette Use, and Depression With All-Cause Mortality Among Adults Living With and Without HIV Infection: Veterans Aging Cohort Study. Open Forum Infectious Diseases, 6(6), 1–8. https://doi.org/10.1093/ofid/ofz188
Collins, L. M., & Wugalter, S. E. (1992). Latent Class Models for Stage-Sequential Dynamic Latent-Variables. Multivariate Behavioral Research, 27(1), 131–157. https://doi.org/10.1207/s15327906mbr2701_8
Fan, X. W., Guo, X., Ren, Z., Li, X. R., He, M. F., Shi, H., Zha, S., Qiao, S. Y., Zhao, H. F., Li, Y. Y., Pu, Y. J., Liu, H. J., & Zhang, X. M. (2021). The prevalence of depressive symptoms and associated factors in middle-aged and elderly Chinese people. Journal of Affective Disorders, 293, 222–228. https://doi.org/10.1016/j.jad.2021.06.044
Fu, C., Cao, L. M., & Yang, F. (2023). Prevalence and determinants of depressive symptoms among community-dwelling older adults in China based on differences in living arrangements: a cross-sectional study. Bmc Geriatrics, 23(1). https://doi.org/10.1186/s12877-023-04339-6
Geiser, C., Lehmann, W., & Eid, M. (2006). Separating “rotators” from “nonrotators” in the Mental Rotations Test: A multigroup latent class analysis. Multivariate Behavioral Research, 41(3), 261–293. https://doi.org/10.1207/s15327906mbr4103_2
Guarnaccia, P. J., Angel, R., & Worobey, J. L. (1989). The Factor Structure of the Ces-D in the Hispanic Health and Nutrition Examination Survey - the Influences of Ethnicity, Gender and Language. Social Science & Medicine, 29(1), 85–94. https://doi.org/10.1016/0277-9536(89)90131-7
Guo, J., Guan, L. D., Fang, L. M., Liu, C. C., Fu, M. Q., He, H., & Wang, X. H. (2017). Depression among Chinese older adults: A perspective from Hukou and health inequities. Journal of Affective Disorders, 223, 115–120. https://doi.org/10.1016/j.jad.2017.07.032
He, D. L., Fan, Y. Y., Qiao, Y. A., Liu, S. Y., Zheng, X. W., & Zhu, J. J. (2023). Depressive symptom trajectories and new-onset arthritis in a middle-aged and elderly Chinese population. Journal of Psychosomatic Research, 172. https://doi.org/10.1016/j.jpsychores.2023.111422
Herrman, H., Patel, V., Kieling, C., Berk, M., Buchweitz, C., Cuijpers, P., Furukawa, T. A., Kessler, R. C., Kohrt, B. A., Maj, M., McGorry, P., Reynolds, C. F., Weissman, M. M., Chibanda, D., Dowrick, C., Howard, L. M., Hoven, C. W., Knapp, M., Mayberg, H. S., … Wolpert, M. (2022). Time for united action on depression: A lancet-world psychiatric association commission. Lancet, 399(10328), 957–1022. https://doi.org/10.1016/S0140-6736(21)02141-3
Hong, H., Kang, S., Kim, J., Gong, J. Y., & Kang, H. (2022). Gender difference in the relationships between behavioral risk factors and depression in older Korean adults. Journal of Mens Health, 18(3), 1–8. https://doi.org/10.31083/j.jomh1803067
Hsieh, C.-R., & Qin, X. (2018). Depression hurts, depression costs: The medical spending attributable to depression and depressive symptoms in China. Health Economics, 27(3), 525–544. https://doi.org/10.1002/hec.3604
Hu, T., Zhao, X. Y., Wu, M., Li, Z. Y., Luo, L., Yang, C. M., & Yang, F. (2022a). Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Research, 311(114), 1–10. https://doi.org/10.1016/j.psychres.2022.114511
Hu, X., Chen, Y., Wang, Z., Huebner, E. S., & Ling, Y. (2022b). A Latent Transition Analysis of Internet Addiction in Early Adolescents and Its Contributing Factors. Journal of Early Adolescence, 43(5), 603–631. https://doi.org/10.1177/02724316221116045
Hua, Y., Wang, B., Wallen, G. R., Shao, P., Ni, C. P., & Hua, Q. Z. (2015). Health-Promoting Lifestyles and Depression in Urban Elderly Chinese. PLoS ONE, 10(3), 1–11. https://doi.org/10.1371/journal.pone.0117998
Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A., & Jaffe, M. W. (1963). Studies of Illness in the Aged-the Index of ADL-a Standardized Measure of Biological and Psychosocial Function. JAMA, 185(12), 914–919. https://doi.org/10.1001/jama.1963.03060120024016
Kleinjan, M., Wanner, B., Vitaro, F., Van den Eijnden, R., Brug, J., & Engels, R. (2010). Nicotine Dependence Subtypes Among Adolescent Smokers: Examining the Occurrence, Development and Validity of Distinct Symptom Profiles. Psychology of Addictive Behaviors, 24(1), 61–74. https://doi.org/10.1037/a0018543
Knoll, N., Rieckmann, N., & Kienle, R. (2007). The other way around: Does health predict perceived support? Anxiety Stress and Coping, 20(1), 3–16. https://doi.org/10.1080/10615800601032823
Kong, X. K., Xiao, Q. L., & Li, J. (2018). Urban-rural comparison on the risk factors of geriatric depressive symptoms. Chinese Mental Health Journal, 32(8), 648–655. https://doi.org/10.3969/j.issn.1000-6729.2018.08.005
Krishnamoorthy, Y., Rajaa, S., & Rehman, T. (2020). Diagnostic accuracy of various forms of geriatric depression scale for screening of depression among older adults: Systematic review and meta-analysis. Archives of Gerontology and Geriatrics, 87, 1–11. https://doi.org/10.1016/j.archger.2019.104002
Lamers, F., Rhebergen, D., Merikangas, K. R., de Jonge, P., Beekman, A. T. F., & Penninx, B. (2012). Stability and transitions of depressive subtypes over a 2-year follow-up. Psychological Medicine, 42(10), 2083–2093. https://doi.org/10.1017/S0033291712000141
Lenferink, L. I. M., Liddell, B. J., Byrow, Y., O’Donnell, M., Bryant, R. A., Mau, V., McMahon, T., Benson, G., & Nickerson, A. (2022). Course and predictors of posttraumatic stress and depression longitudinal symptom profiles in refugees: A latent transition model. Journal of Psychiatric Research, 146, 1–10. https://doi.org/10.1016/j.jpsychires.2021.12.009
Li, D., Zhang, D. J., Shao, J. J., Qi, X. D., & Tian, L. (2014). A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Archives of Gerontology and Geriatrics, 58(1), 1–9. https://doi.org/10.1016/j.archger.2013.07.016
Li, C., Liu, J., Ju, Y. M., Liu, B. S., & Zhang, Y. (2023). Multiple trajectories of depressive symptoms among Chinese in middle and late life: Characterization and risk factors. International Journal of Social Psychiatry, 69(6), 1462–1471. https://doi.org/10.1177/00207640231164020
Liao, Y. G., & Lian, R. (2020). Latent Transition Analysis of Depressive Symptoms in Adults: A Four-year Longitudinal Study. Chinese Journal of Clinical Psychology, 28(3), 518–522. https://doi.org/10.16128/j.cnki.1005-3611.2020.03.01
Lubke, G., & Muthen, B. O. (2007). Performance of factor mixture models as a function of model size, covariate effects, and class-specific parameters. Structural Equation Modeling-a Multidisciplinary Journal, 14(1), 26–47. https://doi.org/10.1207/s15328007sem1401_2
Luo, J., Liu, R., Luo, Y., Fang, Q., Liu, S., Yang, Z., Miao, J., & Lili, Z. (2023). The high burden of symptoms associated with cognitive impairment in lung cancer patients: A latent class analysis. Asia-Pacific Journal of Oncology Nursing, 10(4), 1–8. https://doi.org/10.1016/j.apjon.2023.100200
Moreno-Agostino, D., Wu, Y. T., Daskalopoulou, C., Hasan, M. T., Huisman, M., & Prina, M. (2021). Global trends in the prevalence and incidence of depression:A systematic review and meta-analysis. Journal of Affective Disorders, 281, 235–243. https://doi.org/10.1016/j.jad.2020.12.035
Ni, Y. H., Tein, J. Y., Zhang, M. Q., Yang, Y. W., & Wu, G. T. (2017). Changes in depression among older adults in China: A latent transition analysis. Journal of Affective Disorders, 209, 3–9. https://doi.org/10.1016/j.jad.2016.11.004
Nylund, K. L., Asparoutiov, T., & Muthen, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling-a Multidisciplinary Journal, 14(4), 535–569. https://doi.org/10.1080/10705510701575396
Parker, G., Roy, K., Hadzi-Pavlovic, D., Wilhelm, K., & Mitchell, P. (2001). The differential impact of age on the phenomenology of melancholia. Psychological Medicine, 31(7), 1231–1236. https://doi.org/10.1017/S0033291701004603
Petkus, A. J., Beam, C. R., Johnson, W., Kaprio, J., Korhonen, T., McGue, M., Neiderhiser, J. M., Pedersen, N. L., Reynolds, C. A., & Gatz, M. (2017). Gene-environment interplay in depressive symptoms: Moderation by age, sex, and physical illness. Psychological Medicine, 47(10), 1836–1847. https://doi.org/10.1017/S0033291717000290
Ren, F., Liu, J. L., Fang, Y. S., & Wang, M. C. (2019). Measurement Invariance of the CES-D in Adult Sample. Chinese Journal of Clinical Psychology, 27(5), 973–977. https://doi.org/10.16128/j.cnki.1005-3611.2019.05.025
Rodgers, S., Ajdacic-Gross, V., Muller, M., Hengartner, M. P., Holtforth, M. G., Angst, J., & Rossler, W. (2014). The role of sex on stability and change of depression symptom subtypes over 20 years: A latent transition analysis. European Archives of Psychiatry and Clinical Neuroscience, 264(7), 577–588. https://doi.org/10.1007/s00406-013-0475-3
Sun, F., Li, W. L., Jiang, L., & Lee, J. (2020). Depressive symptoms in three Chinese older workforce groups: The interplay of work stress with family and community factors. International Psychogeriatrics, 32(2), 217–227. https://doi.org/10.1017/S1041610219000528
Tang, T., Jiang, J. L., & Tang, X. F. (2021). Prevalence of depressive symptoms among older adults in mainland China: A systematic review and meta-analysis. Journal of Affective Disorders, 293, 379–390. https://doi.org/10.1016/j.jad.2021.06.050
Tay, A. K., Jayasuriya, R., Jayasuriya, D., & Silove, D. (2017). Twelve-month trajectories of depressive and anxiety symptoms and associations with traumatic exposure and ongoing adversities: A latent trajectory analysis of a community cohort exposed to severe conflict in Sri Lanka. Translational Psychiatry, 7, 1–9. https://doi.org/10.1038/tp.2017.166
Torre-Luque, La, A. D., & Ayuso-Mateos, J. L. (2020). The course of depression in late life: a longitudinal perspective. Epidemiology and Psychiatric Sciences, 29. https://doi.org/10.1017/S204579602000058X
Ulbricht, C. M., Chrysanthopoulou, S. A., Levin, L., & Lapane, K. L. (2018a). The use of latent class analysis for identifying subtypes of depression: A systematic review. Psychiatry Research, 266, 228–246. https://doi.org/10.1016/j.psychres.2018.03.003
Ulbricht, C. M., Dumenci, L., Rothschild, A. J., & Lapane, K. L. (2018b). Changes in Depression Subtypes Among Men in STAR*D: A Latent Transition Analysis. American Journal of Mens Health, 12(1), 5–13. https://doi.org/10.1177/1557988315607297
Veltman, E., Kok, A., Lamers, F., Stek, M., van der Mast, R., & Rhebergen, D. (2020). Stability and transition of depression subtypes in late life. Journal of Affective Disorders, 265, 445–452. https://doi.org/10.1016/j.jad.2020.01.049
Wang, C., Wu, Z., & Fang, Y. (2018). Progress in researches on latent class analysis based subtyping of depression. Journal of Shanghai Jiao Tong University, 38(6), 676–679. https://doi.org/10.3969/j.issn.1674-8115.2018.06.016
Wang, Q., Ding, F., Chen, D. N., Zhang, X. Y., Shen, K. H., Fan, Y. Y., & Li, L. (2020). Intervention effect of psychodrama on depression and anxiety: A meta-analysis based on Chinese samples. Arts in Psychotherapy, 69, 1–13. https://doi.org/10.1016/j.aip.2020.101661
Yen, S., Robins, C. J., & Lin, N. (2000). A cross-cultural comparison of depressive symptom manifestation: China and the United States. Journal of Consulting and Clinical Psychology, 68(6), 993–999. https://doi.org/10.1037/0022-006X.68.6.993
Ying, P. X., Li, H., & Tan, J. W. (2021). The superiority of high level of father presence on empathy and sympathy in early adolescents in south-eastern China: A person-centered perspective. Personality and Individual Differences, 181, 1–6. https://doi.org/10.1016/j.paid.2021.111048
Yuan, Y., Lapane, K. L., Rothschild, A. J., & Ulbricht, C. M. (2021). Changes in depressive symptoms and cognitive impairment in older long-stay nursing home residents in the USA: A latent transition analysis. Aging & Mental Health, 25(10), 1903–1912. https://doi.org/10.1080/13607863.2020.1849021
Yuan, L., Xu, Q., Gui, J., Liu, Y. Q., Lin, F. W., Zhao, Z., & Sun, J. H. (2023). Decomposition and comparative analysis of differences in depressive symptoms between urban and rural older adults: Evidence from a national survey. International Psychogeriatrics. https://doi.org/10.1017/S1041610223000078
Zhang, L., Xu, Y., Nie, H. W., Zhang, Y. D., & Wu, Y. (2012). The prevalence of depressive symptoms among the older in China: A meta-analysis. International Journal of Geriatric Psychiatry, 27(9), 900–906. https://doi.org/10.1002/gps.2821
Zhang, C. C., Li, M. M., & Zhao, H. N. (2019). Logistic regression and decision tree of anxiety status and its influencing factors in empty-nesters. Chinese Mental Health Journal, 33(8), 598–600. https://doi.org/10.3969/j.issn.1000-6729.2019.08.009
Zhao, Y. H., Hu, Y. S., Smith, J. P., Strauss, J., & Yang, G. H. (2014). Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). International Journal of Epidemiology, 43(1), 61–68. https://doi.org/10.1093/ije/dys203
Zhao B, & C., J. (2018). Analysis of the physical and mental factors of anxiety and depression in the elderly. Chinese Journal of Geriatrics, 37(10), 1156-1160. https://doi.org/10.3760/cma.j.issn.0254-9026.2018.10.024
Zheng, X., Cui, Y., Xue, Y., Shi, L., Guo, Y., Dong, F., & Zhang, C. (2022). Adverse childhood experiences in depression and the mediating role of multimorbidity in mid-late life: A nationwide longitudinal study. Journal of Affective Disorders, 301, 217–224. https://doi.org/10.1016/j.jad.2022.01.040
Acknowledgements
The data were from the China Health and Retirement Longitudinal Study (CHARLS). We thank the Institute of Social Science Survey of Peking University for the CHARLS data collection and analysis files. Thank you to the numerous staff members who have made tremendous efforts and selfless contributions to the CHARLS investigation.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Xuyang Li planned the study, framed the research, analyzed data and wrote the paper.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for this type of study is not required by our institute.
Ethics statement
The data collection was approved by the Ethics Review Committee of Peking University, and all respondents were informed and agreed in writing.
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key messages
1. severe depressive symptoms group has the most prominent risk and considerable stability, which is the key object to prevent the transformation to clinical depression and to reduce the malignant events caused by extreme emotions of individuals.
2. For the mild depressive symptoms group and transition group, the focus of the intervention is to curb their natural transition towards deterioration.
3. We suggests to focus on strengthening the female, rural residents, non-marital status, alcohol consumption, disability, poor self-assessed health status, and low life satisfaction is conducive to improving the effectiveness of depression prevention and control among the elderly in China.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, X. Stability and transitions of depressive symptoms among Chinese older adults over a 5-year follow up. Curr Psychol 43, 15787–15797 (2024). https://doi.org/10.1007/s12144-023-05522-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-023-05522-z