Abstract
This study investigated objective and subjective cognitive effort as a function of task difficulty in schizophrenia, based on the principles of motivational intensity theory. Thirty individuals with schizophrenia and 30 healthy controls worked on four levels of a working memory task ranging from easy to extremely difficult. We assessed objective effort as cardiovascular activity during task performance and subjective effort via self-report. In addition, we assessed participants’ task performance, negative symptoms, amotivation, depression, and fatigue. Cardiovascular activity during the task increased only in the healthy control group, but not in the schizophrenia group, indicating attenuated objective effort in schizophrenia. However, individuals with schizophrenia reported similar levels of subjective effort as healthy controls. Moreover, we found a negative association between fatigue and cardiovascular activity only in the schizophrenia group. Our results show a dissociation between objective and subjective effort in schizophrenia, which may explain decreased willingness to mobilize cognitive resources in individuals with schizophrenia. Moreover, our results highlight the importance of fatigue in effort in schizophrenia, a variable rarely considered in the current literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies suggest that the role of cognitive deficits in schizophrenia could have been overestimated and attributable to secondary factors and notably reduced effort (Beck et al., 2018; Grant et al., 2019; Kreis et al., 2020; Moritz et al., 2017). The few studies that have investigated cognitive effort in schizophrenia have consistently found a reduced willingness to expend cognitive effort. This applies to both behavioral measures based on effort-based decision-making paradigms (Culbreth et al., 2016, 2020; Reddy, Horan, et al., 2018; Strauss et al., 2016; Wolf et al., 2014) and psychophysiological measures, mainly pupillary responses, as an indicator of objective effort (McGovern et al., 2020; Reddy, Reavis, et al., 2018). Reduced effort in schizophrenia seems to be associated with negative symptoms (e.g., Culbreth et al., 2020; Gold et al., 2013; Granholm et al., 2007, 2016) including amotivation, even though not all studies find this association (e.g., Fervaha et al., 2013, 2015; Kreis et al., 2020).
As stated above, past studies with schizophrenic individuals have applied decision-making paradigms in which the dependent variable was individuals’ willingness to mobilize resources for obtaining rewards (Culbreth et al., 2018). However, according to theories based on the energy conservation principle, such as motivational intensity theory (MIT) (Brehm & Self, 1989), momentary effort is primarily a function of subjective task difficulty (i.e., task demand). MIT posits that effort rises proportionally with subjective task difficulty up to the point where a task is perceived as too difficult. Subjective task difficulty results from the integration of all available information about task demand, including objective task difficulty and other information like individuals’ current state (e.g., mood). The benefits of success (e.g., rewards) only indirectly influence the proportional relationship between perceived task difficulty and effort—they determine the maximum effort that is justified. Up to that limit, resources are mobilized proportionally to subjective demand. MIT has received ample empirical support regarding objective physiological measures of effort (Gendolla, et al., 2019; Wright & Kirby, 2001).
Based on Wright’s (1996) integration of MIT with the active coping approach (Obrist, 1981), a considerable number of experiments have confirmed the predictions of MIT using cardiovascular measures reflecting resource mobilization (Gendolla et al., 2012, 2019, for overviews). This research is based on the observation that beta-adrenergic sympathetic nervous system (SNS) impact on the heart is proportional to task engagement (Obrist, 1981). Pre-ejection period (PEP)—a cardiac contractile force indicator—is the most direct non-invasive measure of beta-adrenergic impact. Systolic blood pressure (SBP)—the maximum arterial pressure following a heartbeat—is a satisfactory effort indicator because cardiac contractile force systematically influences systolic pressure (Levick, 2003). SBP is easier to measure than PEP and will be the main dependent variable in the present study. In contrast, heart rate (HR) and diastolic blood pressure (DBP) are less systematically influenced by beta-adrenergic SNS impact (Papillo & Shapiro, 1990) and less reliably reflect effort.
Research in the context of MIT has identified several variables, like fatigue, that influence perceived difficulty and consequently effort (Gendolla et al., 2012, 2019; Wright, 2014; Wright & Stewart, 2012). Individuals who experience high levels of fatigue perceive tasks as more difficult and mobilize more effort than individuals who experience low levels of fatigue when tasks are relatively easy. However, because fatigue increases subjective difficulty, it leads to disengagement in objectively difficult tasks. Dispositional negative mood influences perceived task difficulty in a similar way (e.g., Brinkmann & Gendolla, 2007, 2008; Silvia et al., 2014, 2016). These latter studies were based on the mood-behavior-model (MBM; Gendolla, 2000), according to which mood is integrated as a piece of information together with other diagnostic information in behavior-related judgments. Hence, individuals in a negative mood judge the difficulty of a task as higher than those in a positive mood (e.g., Gendolla et al., 2001). Resources are then mobilized according to the principles of MIT (Gendolla et al., 2012). Interestingly, depressive symptoms including negative mood (Baynes et al., 2000) and fatigue (Waters et al., 2013) are highly prevalent in schizophrenia—up to 75% of individuals with schizophrenia have these symptoms. Although these variables might exert an impact on cognitive effort in individuals with schizophrenia, they have been largely ignored to date.
Furthermore, past studies on effort in schizophrenia have hardly considered the role of subjective effort although the process of resource mobilization includes a subjective experience, which appears to be essential (van den Bosch & Rombouts, 1997). Research with healthy participants has not found clear relationships between physiologically assessed objective effort and effort experiences (e.g., Bijleveld, 2018). To date, only one study has assessed both objective effort (pupillary responses) and subjective effort (self-report) in schizophrenia (Kreis et al., 2020). Results showed lower objective effort and higher subjective effort in schizophrenia compared to healthy controls. Nevertheless, the patient group in this study was not representative of the schizophrenia population; its memory performance was comparable to the healthy control group. Taken together, insights in the relationships between objective resource mobilization and subjectively experienced effort in schizophrenia are scarce.
In the present study, we investigated for the first time both objective cognitive and subjective effort in schizophrenia. To assess objective effort, we monitored cardiovascular activity, especially SBP, during a short-term memory task. In addition, we assessed subjective effort at the end of each of the four task difficulty levels. Finally, we also examined how SBP activity during cognitive performance was influenced by fatigue, negative mood, and negative symptoms.
Based on the predictions and extensions of MIT (Gendolla et al., 2012, 2019), we expected that SBP activity (i.e., objective effort) in the schizophrenia group would be higher on the easy and moderate task levels but lower on the difficult level compared to healthy controls. This is due to more negative mood and fatigue in schizophrenia, resulting in the experience of higher task demand (Gendolla, 2000; Wright, 2014). On the extremely difficult level SBP activity was expected to be low for all participants. Based on previous findings (e.g., Kreis et al., 2020), we expected that the schizophrenia group would perceive subjective effort as higher than the healthy control group.
In contrast to the theory-based main hypotheses described above, we did not formulate any a priori hypotheses concerning the links between effort and negative symptoms, notably amotivation, in schizophrenia because past research has revealed mixed results. Related statistical analyses were conducted exploratively.
Method
Participants
Based on power considerations described in detail at the end of this section, we recruited 35 individuals with a diagnosis of schizophrenia according to DSM-5 criteria and 33 healthy controls. Groups were matched on sex, age, and educational status. All individuals with schizophrenia were recruited at the hospital. The final patient sample consisted of 4 hospitalized individuals, 4 individuals treated in an inpatient clinic, 17 individuals followed by a recovery and rehabilitation center, and 5 outpatients. Non-clinical participants were recruited from a list of persons who had already completed psychological studies. Non-inclusion criteria comprised neurological disorders or cranial trauma antecedents, cardiovascular disease and/or treatment for high blood pressure, and abuse of/dependence on a substance (except cannabis or tobacco). To exclude psychotic disorders in healthy controls, we assessed the 7th version of the DSM-5 Mini-International Neuropsychiatric Interview (Sheehan, 2016). From the 68 participants initially enrolled in the study, 8 participants (5 individuals with schizophrenia and 3 healthy controls) were excluded for the following reasons: one patient wished to abandon the study in progress, 2 patients and 1 healthy control individual showed extreme cardiovascular reactivity (outliers), 2 patients had missing data due to a computer problem, and 2 healthy controls presented severe depressive symptoms, leaving data of 30 patients and 30 healthy controls for data analysis. Data of participants with extreme cardiovascular reactivity (i.e., cardiovascular task score - cardiovascular baseline score) were removed based on the criterion z < -3.29 (Fields, 2013). Specifically, these participants had extremely low cardiovascular activity during the task period compared with the baseline period. This suggests that these participants probably moved their arms during the resting period, biasing their cardiovascular baseline values.
For patients, treatment doses were calculated in chlorpromazine equivalents according to the minimum effective dose method (Leucht et al., 2015). In the schizophrenia group, psychotic symptoms were evaluated with the Positive and Negative Syndrome Scale (PANSS, Kay et al., 1987). As the best tool available in French, the Scale for the Assessment of Negative Symptoms (SANS, Andreasen, 1989) was used to specifically measure negative symptoms and amotivation (i.e., Avolition score of the SANS). All participants completed the second version of the Beck Depression Inventory (BDI-II; Beck et al., 1996) and the Fatigue Impact Scale (FIS, Fisk et al., 1994). To determine the mental load in working memory, we administered the WAIS IV Letter-Digit Sequence test (Wechsler, 2008). We also recorded Body Mass Index (BMI).
In previous studies using cardiovascular measures of objective effort, medium effect sizes have been usual. According to an a priori power analysis with MorePower (Campbell & Thompson, 2012), the required minimal sample size was 11 participants per group to detect a medium effect size with 80% power in our 5 × 2 mixed model ANOVA. The study was conducted according to the ethics code of the World Medical Association (Declaration of Helsinki) and its later amendments (IRB approval: 202000663). Participants did not receive any payment for participation.
Cardiovascular Measures
Cardiovascular activity was noninvasively assessed with the Dinamap Procare monitor® (GE Medical Systems, Information Technologies Inc., Milwaukee, WI), which uses oscillometry to determine blood pressure activity. The blood pressure cuff was placed on the brachial artery above the elbow of participants’ non-dominant arm and inflated automatically. SBP and DBP (both in millimeters of mercury, mmHg) and HR (in beats per minute, bpm) were recorded each minute during the baseline period and during each difficulty level of the experimental task.
Self-Report Measures
All participants were asked to indicate their current mood state by means of two positive (“happy”, “joyful”) and two negative (“sad”, “depressed”) items from the hedonic tone scales of the U-WIST (Matthews et al., 1990) using 7-point Likert scales ranging from 1 (not at all) to 7 (very much). An index was calculated by summing the negative and reverse-scored positive items; the higher the score, the more negative the mood (Cronbach’s α = 0.80). We added one question about current fatigue level to be answered on a 7-point Likert scale from 1 (not at all tired) to 7 (very tired). In addition, all participants self-reported the amount of effort they had expended (1—no effort to 7—considerable effort). Other task-related self-report measures are reported in the Supplemental Online Material (SOM).
Experimental Task
We administered a computerized Sternberg-type short-term memory task in which participants determined whether a target letter had been part of a series of previously presented letters. Each trial started with a centrally displayed fixation cross (1000 ms), which was replaced by a series of meaningless letters (e.g., “KJHGFD”) (750 ms), followed by a mask consisting of a row of “X”, and a target letter. The participant had a maximum of 2000 ms to indicate as quickly and accurately as possible whether that target letter had been present or not in the previous letter series by pressing respective response keys. If the participant did not respond within 2000 ms, the message "Please respond faster" appeared. Objective task difficulty was manipulated by varying the number of letters: 3 letters for the easy level, 5 for the moderate level, 7 for the difficult level, and 12 for the extremely difficult level. The difficulty levels order was randomized. Correctness feedback (during training) and a "response recorded" message (during the experimental task) were displayed after each response. To keep the duration of each trial identical for all participants, these messages were presented for 4000 ms minus participants’ reaction time. The experimental task was programmed using E-Prime 2.0 (Psychology Software Tools, Pittsburgh, PA). Each level of difficulty consisted of 24 trials for a total duration of 3 min per level.
Procedure
After having read introductory information, participants signed the consent form and sat down in a comfortable chair in front of a computer in a quiet room in the hospital. At recruitment, participants had been asked not to drink coffee or tea and not to smoke 30 min before the experiment to avoid effects on cardiovascular measures. The experimenter placed the blood pressure cuff on participants’ nondominant arm and provided a cushion to stabilize the arm in a comfortable position. Participants were asked not to move their arm during the experiment to prevent movement artefacts. The instructions were presented on-screen, and the experimenter took place in an adjacent control room. To avoid observer bias, participants were informed that the experimenter could not monitor their performance.
First, participants indicated their momentary mood and fatigue. Second, participants completed an 8-min resting period to assess cardiovascular baseline values, while they watched an emotionally neutral documentary ("The heritage of the Ardèche"). Third, participants worked on the experimental task, starting with 8 training trials comprised of series of 6 nonsense letters. Afterwards, participants completed the four difficulty levels. At the end of each difficulty level, participants rated subjective effort and other task-related self-report measures (see SOM). Before each difficulty level, a 2-min break was programmed so that cardiovascular activity could return to the resting state. After having performed all levels of the Sternberg task there was a 10-min break, after which participants performed a working memory test and completed the questionnaires and the semi-structured interview about clinical measures. Finally, participants were debriefed and thanked for their participation. Figure 1 summarizes the procedure.
Data Reduction and Primary Measures
Our primary effort measures were objective SBP activity (in mmHg) and subjective self-reported effort. Descriptive statistics and results for DBP, HR, and task demand appraisals are presented in the SOM. Cardiovascular baseline scores (t1) were computed by averaging the last three measures (last 3 min) of the resting period (Cronbach’s αs > 0.98). Cardiovascular task activity was determined by averaging the three measures collected for each task difficulty level (Cronbach’s αs > 0.94).
Based on signal detection theory (Green & Swets, 1966), we calculated a sensitivity index (d') as performance measure (d’ = z(Hits)–z(False Alarms)) for the Sternberg task. Given that some data had probabilities equal to 1 (in the case that participants did not make any errors), which does not allow for a d’ calculation, we added 0.5 to all data (Fienberg, 2007). Moreover, we assessed reaction times for correct responses.
Data-Analysis Plan
Statistical analyses were performed with JASP0.14.0.0. First, we compared socio-demographic, working memory span, psychological, and bodyweight data between the two participant groups. All data were normally distributed (i.e., absolute values for skewness and kurtosis were lower than 3 and 10, respectively, Weston & Gore, 2006). For our primary theory-based hypotheses, we conducted a 5 (Difficulty) × 2 (Group) mixed-model ANOVA of SBP activity, including baseline activity as t1 measure together with the four difficulty levels. We did not compute cardiovascular reactivity scores (Llabre et al., 1991), because Difficulty was manipulated as a within-subjects factor. Moreover, we ran 4 (Difficulty) × 2 (Group) mixed-model ANOVAs of the subjective effort and performance measures. Whenever Mauchly’s test of sphericity was significant, a Greenhouse–Geisser correction was applied. For significant ANOVA effects, post hoc multiple comparisons with Bonferroni corrections were conducted. Effect sizes are presented as η2p. For our secondary exploratory analyses, we computed Pearson bivariate or partial correlations (for SBP with baseline t1 measure as control variable) to investigate the relationships between psychological and effort measures in schizophrenia. A Benjamini-Yekutieli correction (Benjamini & Yekutieli, 2001) was performed to control for false discovery rate of multiple tests.
Results
Group Comparisons
Sociodemographic, clinical, neuropsychological, bodyweight, momentary mood, and fatigue data for the two groups are presented in Table 1. No significant differences were found for gender, education, and age (ps > 0.06). Individuals with schizophrenia reported more depressive symptoms (M = 14.17, SD = 9.50) than healthy controls (M = 3.53, SD = 2.66), t(58) = -5.90, p < 0.001, d = -1.53. Individuals with schizophrenia also reported more fatigue (M = 78.10, SD = 24.50) than healthy controls (M = 47.30, SD = 27.70), t(58) = -4.56, p < 0.001, d = -1.18. Participants in the schizophrenia group (M = 12.87, SD = 4.10) were in a significantly more negative momentary mood than healthy controls (M = 8.50, SD = 3.48), t(58) = -4.45, p < 0.001, d = -1.15. However, no significant difference between the two groups emerged for momentary fatigue, t(58) = -0.08, p = 0.93, d = -0.02. Working memory scores were lower in the schizophrenia group (M = 17.30, SD = 3.03) compared to the healthy control group (M = 19.18, SD = 2.35), t(58) = 2.67, p = 0.01, d = 0.69. Finally, BMI was higher in the schizophrenia group (M = 25.62, SD = 5.87) than in the healthy control group (M = 22.76, SD = 2.85), t(58) = -2.37, p = 0.02, d = -0.62.
Effort Measures
Objective Effort—SBP Activity
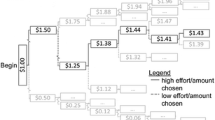
The 5 × 2 ANOVA revealed a Difficulty main effect, F(3.22, 187.06) = 15.08, p < 0.001, η2p = 0.21, and a Difficulty x Group interaction, F(3.22, 187.06) = 3.94, p = 0.008, η2p = 0.06, in absence of a Group main effect (p = 0.13) (see Fig. 2). Follow-up comparisons of the interaction showed that baseline values were significantly lower than the four task measures in the healthy control group (ps < 0.001). By contrast, in the schizophrenia group, no significant differences emerged between the five SBP measures (ps > 0.33).
Means and standard errors of SBP activity as a function of group and difficulty (asterisks indicate a significant difference). The standard errors were corrected according to the within-subjects design as proposed by Cousineau & O’Brien (2014)
In the schizophrenia group, an association between SBP and fatigue (FIS) emerged, r(27) = 0.40, p = 0.030. No significant associations between SBP and negative mood (BDI-II, U-WIST) were found in schizophrenia, r(27) = 0.14, p = 0.48; r(27) = -0.14, p = 0.48, respectively. Neither negative symptoms nor amotivation were significantly associated with SBP activity, r(27) = -0.09, p = 0.64; r(27) = 0.33, p = 0.09, respectively.
Subjective Effort – Self-Reported Effort
Only a Difficulty main effect was found, F(2.53, 146.66) = 39.25, p < 0.001, η2p = 0.40 (other ps > 0.36). All difficulty levels significantly differed from each other (ps < 0.001), except the moderate and difficult levels (p = 0.09). As objective task difficulty increased, so did subjective effort (see Fig. 3).
Task Performance Measures
Sensitivity – d’ Index
We found a Difficulty main effect, F(3, 174) = 162.11, p < 0.001, η2p = 0.74 (other ps > 0.16). All difficulty levels significantly differed from each other (ps < 0.001). The sensitivity index decreased with increasing task difficulty (see Table 2).
Reaction Times
The analysis revealed a Group main effect, F(1, 58) = 7.94, p = 0.007, η2p = 0.12. Individuals with schizophrenia responded significantly slower than healthy controls. Also the Difficulty main effect was significant, F(3, 174) = 30.02, p < 0.001, η2p = 0.34. As depicted in Fig. 4, reaction times increased with objective task difficulty. All difficulty levels significantly differed from each other (ps < 0.001), except the moderate and difficult conditions (p = 0.90). The interaction effect was not significant (p = 0.60).
Discussion
This study investigated objective and subjective cognitive effort in schizophrenia compared with healthy controls. Regarding objective effort, healthy controls’ SBP increased during the task compared to the baseline period, whereas individuals with schizophrenia showed no such effect. That is, using a well validated psychophysiological measure of objective effort (Gendolla et al., 2012, 2019; Richter et al., 2016; Wright & Kirby 2001, for reviews), our results indicate impaired resource mobilization in the schizophrenia group. However, while schizophrenia individuals did not increase their objective effort during the cognitive task, they reported a similar level of subjective effort as the healthy control participants. Interestingly, other studies found that individuals with schizophrenia perceived to expend higher cognitive effort than healthy controls (e.g., Culbreth et al., 2016; Kreis et al., 2020). A dissociation of objective and subjective effort measures was also found in metacognition (Raffard et al., 2020a) and in the intensity of physical exercise in individuals at high risk for psychosis (Damme et al., 2021). Although our results were not identical with those previous findings, they support the idea of an effort dissociation in schizophrenia in that low objective effort goes together with the experience of high subjective effort.
Our finding of blunted SBP reactivity in the schizophrenia group is consistent with studies using pupil dilation as objective effort measure (Granholm et al., 2007; Kreis et al., 2020) and corroborates the hypothesis of blunted cognitive effort in schizophrenia. However, contrary to our predictions, we did not find that objective difficulty moderated SBP activity. Although there was a significant difference in SBP activity between baseline and task in the control group, reflecting increased effort during performance, we did not find that SBP was further moderated by objective task difficulty. It is conceivable that the within-persons task difficulty manipulation has prevented us from replicating difficulty effects found in previous studies with between-persons difficulty manipulations (e.g., Richter et al., 2008). However, while healthy controls showed a general increase in objective effort during task performance, individuals with schizophrenia did not—they remained on their baseline level.
It is of note that the SBP baseline values in the schizophrenia group were higher than in the healthy control group. One might therefore suspect that schizophrenia individuals’ SBP activity could not increase much more during the experimental task in line with the law of initial values (see Llabre et al., 1991). On the other hand, studies on depression found that depressed individuals’ SBP could increase during cognitive tasks even with high SBP baseline values (Franzen & Brinkmann, 2015; Franzen et al., 2019). Moreover, the SBP values of the schizophrenia group in the present study were still normotensive (Chobanian et al., 2003). Therefore, we conclude that the lack of SBP reactivity in the present study’s schizophrenia group points to deficits in objective cognitive effort rather than to other physiological reasons underlying the lack of adjustment to task demands.
However, unlike most other studies (e.g., Culbreth et al., 2016, 2020; Granholm et al., 2007, 2016), we found no evidence for associations with negative symptoms. One reason for this could be that we did not manipulate reward but task difficulty. Indeed, previous research indicates that negative symptoms are associated with an underestimation of reward value (Strauss et al., 2014, for review). A second reason for not finding a significant association might be the low severity of negative symptoms in the present schizophrenia group. A third reason might be that we did not use the gold standard tool for assessing negative symptoms, such as the Clinical Assessment Interview for Negative Symptoms (CAINS, Kring et al., 2013) or the Brief Negative Symptom Scale (BNSS, Strauss et al., 2012), for which no validated French versions exist. These points should be considered for future studies.
Short-term memory performance was affected by schizophrenia. Although the sensitivity index was similar in both groups, reaction times were significantly longer in the schizophrenia group than in the control group. The latter effect is consistent with the literature (Aleman et al., 1999). Furthermore, reaction times increased and sensitivity decreased with objective task difficulty in both groups, indicating effective manipulations of objective task difficulty.
Another interesting result of our study is the association between cognitive effort and fatigue in schizophrenia. Fatigue refers to “the awareness of a decreased capacity for physical and/or mental activity due to an imbalance in the availability, utilization, and/or restoration of resources needed to perform activity” (Aaronson et al., 1999, p.46). Fatigue affects subjective task difficulty and thus effort: For objectively easy tasks, individuals who experience high levels of fatigue perceive task demand as higher and thus mobilize more resources than those with low levels of fatigue (e.g., Wright & Stewart, 2012). Surprisingly, to date fatigue has not been considered in effort investigations in schizophrenia, although up to 60% of patients experience significant levels of fatigue (Waters et al., 2013) and although fatigue leads to motivational difficulties and cognitive deficits (Raffard, Rainteau, et al., 2020). Cognitive and behavioral therapies for fatigue have been shown to be effective in chronic fatigue syndrome (Knoop et al., 2008) and are currently implemented in schizophrenia (Raffard et al., 2020b). As such, treating fatigue in schizophrenia could improve the mobilization of cognitive resources. Future studies are needed to test this hypothesis.
Our study has some limitations. The schizophrenia group was relatively asymptomatic regarding amotivation. Although other studies have found associations between SANS avolition scores and objective effort (i.e., pupillary response; Granholm et al., 2007), this scale is not the gold standard for assessing negative symptoms and amotivation (Strauss & Gold, 2016). Another limitation is related to the nature and the assessment of objective effort in terms of SBP activity assessed in a within-subjects design. Future research might use cardiac pre-ejection period as the most reliable non-invasive measure of beta-adrenergic impact on the heart (Gendolla et al., 2019; Richter et al., 2016; Wright, 1996). Additionally, task difficulty could be manipulated between persons to produce stronger effects (Richter et al., 2008).
Taken together, our results indicate that individuals with schizophrenia mobilized less objective effort and responded more slowly than healthy controls but subjectively experienced effort on a similar level as healthy controls. Our findings highlight a dissociation between subjective and objective effort in patients with schizophrenia. The role of fatigue in this process merits to be further investigated in future research.
Data Availability
The datasets collected during the current study are available from the corresponding author on reasonable request.
Notes
Because depression and BMI were significantly higher in the schizophrenia group than in the healthy control group and because these two clinical variables could influence objective effort (i.e., cardiovascular activity), we also considered them as covariates in the analyses of SBP reactivity reported the main text.
Depression (BDI-II score) had no significant covariate main or interaction effects (all ps > .18).
By contrast, BMI had a significant covariate main effect, F(1, 57) = 42.42, p < .001, η2p = .43, on cardiovascular reactivity. Moreover, the analysis revealed a Difficulty x Group interaction, F(3.22, 183.61) = 4.09, p = .007, η2p = .06, in absence of Group (p = .95) or Difficulty (p = .70) main effects. Follow-up comparisons found that the SBP baseline values were significantly lower than the four task measures in the healthy control group (ps < .001). By contrast, in the schizophrenia group, no significant differences emerged between the five SBP measures (ps > .85). The addition of the BMI covariate did not change the Difficulty x Group interaction effect or the follow-up comparisons presented in this manuscript.
We also conducted a 4 (Difficulty) × 2 (Group) mixed-model ANOVA of the error rates (i.e., sums of false alarms and omission errors). That analysis only found a Difficulty main effect, F(2.56, 148.26) = 152.51, p < .001, η2p = .72, (others ps > .09). These results do not differ from those found for the sensitivity index.
References
Aaronson, L. S., Teel, C. S., Cassmeyer, V., Neuberger, G. B., Pallikkathayil, L., Pierce, J., ... & Wingate, A. (1999). Defining and measuring fatigue. Image: The Journal of Nursing Scholarship, 31(1), 45–50.
Aleman, A., Hijman, R., de Haan, E. H. F., & Kahn, R. S. (1999). Memory Impairment in Schizophrenia: A Meta-Analysis. American Journal of Psychiatry, 156(9), 1358–1366. https://doi.org/10.1176/ajp.156.9.1358
Andreasen, N. C. (1989). The Scale for the Assessment of Negative Symptoms (SANS): Conceptual and theoretical foundations. The British Journal of Psychiatry, 155(S7), 49–52. https://doi.org/10.1192/S0007125000291496
Baynes, D., Mulholland, C., Cooper, S. J., Montgomery, R. C., MacFlynn, G., Lynch, G., … King, D. J. (2000). Depressive symptoms in stable chronic schizophrenia: Prevalence and relationship to psychopathology and treatment. Schizophrenia Research, 45(1), 47‑56. https://doi.org/10.1016/S0920-9964(99)00205-4
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498. https://doi.org/10.1037/t00742-000
Beck, A. T., Himelstein, R., Bredemeier, K., Silverstein, S. M., & Grant, P. (2018). What accounts for poor functioning in people with schizophrenia: A re-evaluation of the contributions of neurocognitive v. attitudinal and motivational factors. Psychological Medicine, 48(16), 2776‑2785. https://doi.org/10.1017/S0033291718000442
Benjamini, Y., & Yekutieli, D. (2001). The control of the false discovery rate in multiple testing under dependency. The Annals of Statistics, 29(4), 1165–1188. https://doi.org/10.1214/aos/1013699998
Bijleveld, E. (2018). The feeling of effort during mental activity. Consciousness and Cognition, 63, 218–227. https://doi.org/10.1016/j.concog.2018.05.013
Brehm, J. W., & Self, E. A. (1989). The intensity of motivation. Annual Review of Psychology, 40, 109–131. https://doi.org/10.1146/annurev.ps.40.020189.000545
Brinkmann, K., & Gendolla, G. H. E. (2007). Dysphoria and mobilization of mental effort: Effects on cardiovascular reactivity. Motivation and Emotion, 31(1), 71. https://doi.org/10.1007/s11031-007-9054-0
Brinkmann, K., & Gendolla, G. H. E. (2008). Does depression interfere with effort mobilization? Effects of dysphoria and task difficulty on cardiovascular response. Journal of Personality and Social Psychology, 94(1), 146–157. https://doi.org/10.1037/0022-3514.94.1.146
Campbell, J. I. D., & Thompson, V. A. (2012). MorePower 6.0 for ANOVA with relational confidence intervals and Bayesian analysis. Behavior Research Methods, 44(4), 1255‑1265. https://doi.org/10.3758/s13428-012-0186-0
Chobanian, A. V., Bakris, G. L., Black, H. R., Cushman, W. C., Green, L. A., Izzo, J. L., … null, null. (2003). Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension, 42(6), 1206‑1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2
Cousineau, D., & O’Brien, F. (2014). Error bars in within-subject designs: A comment on Baguley (2012). Behavior Research Methods, 46(4), 1149–1151. https://doi.org/10.3758/s13428-013-0441-z
Culbreth, A., Westbrook, A., & Barch, D. (2016). Negative symptoms are associated with an increased subjective cost of cognitive effort. Journal of Abnormal Psychology, 125(4), 528–536. https://doi.org/10.1037/abn0000153
Culbreth, A. J., Moran, E. K., & Barch, D. M. (2018). Effort-based decision-making in schizophrenia. Current Opinion in Behavioral Sciences, 22, 1–6. https://doi.org/10.1016/j.cobeha.2017.12.003
Culbreth, A. J., Moran, E. K., Kandala, S., Westbrook, A., & Barch, D. M. (2020). Effort, avolition, and motivational experience in schizophrenia: Analysis of behavioral and neuroimaging data with relationships to daily motivational experience. Clinical Psychological Science, 8(3), 555–568. https://doi.org/10.1177/2167702620901558
Damme, K. S. F., Sloan, R. P., Bartels, M. N., Ozsan, A., Ospina, L. H., Kimhy, D., & Mittal, V. A. (2021). Psychosis risk individuals show poor fitness and discrepancies with objective and subjective measures. Scientific Reports, 11(1), 9851. https://doi.org/10.1038/s41598-021-89301-5
Fervaha, G., Graff-Guerrero, A., Zakzanis, K. K., Foussias, G., Agid, O., & Remington, G. (2013). Incentive motivation deficits in schizophrenia reflect effort computation impairments during cost-benefit decision-making. Journal of Psychiatric Research, 47(11), 1590–1596. https://doi.org/10.1016/j.jpsychires.2013.08.003
Fervaha, G., Duncan, M., Foussias, G., Agid, O., Faulkner, G. E., & Remington, G. (2015). Effort-based decision making as an objective paradigm for the assessment of motivational deficits in schizophrenia. Schizophrenia Research, 168(1), 483–490. https://doi.org/10.1016/j.schres.2015.07.023
Field, A. (2013). Discovering statistics using IBM SPSS statistics. sage.
Fienberg, S. E. (2007). The Analysis of Cross-Classified Categorical Data. Springer Science & Business Media.
Fisk, J. D., Ritvo, P. G., Ross, L., Haase, D. A., Marrie, T. J., & Schlech, W. F. (1994). Measuring the functional impact of fatigue: Initial validation of the fatigue impact scale. Clinical Infectious Diseases, 18(Suppl 1), S79-83. https://doi.org/10.1093/clinids/18.supplement_1.s79
Franzen, J., & Brinkmann, K. (2015). Blunted cardiovascular reactivity in dysphoria during reward and punishment anticipation. International Journal of Psychophysiology, 95(3), 270–277. https://doi.org/10.1016/j.ijpsycho.2014.11.007
Franzen, J., Brinkmann, K., Gendolla, G. H. E., & Sentissi, O. (2019). Major depression impairs incentive processing: Evidence from the heart and the face. Psychological Medicine, 49(6), 922–930. https://doi.org/10.1017/S0033291718001526
Gendolla, G. H. E. (2000). On the impact of mood on behavior: An integrative theory and a review. Review of General Psychology, 4(4), 378–408. https://doi.org/10.1037/1089-2680.4.4.378
Gendolla, G. H., Abele, A. E., & Krüsken, J. (2001). The informational impact of mood on effort mobilization: A study of cardiovascular and electrodermal responses. Emotion, 1(1), 12. https://doi.org/10.1037/1528-3542.1.1.12
Gendolla, G. H. E., Wright, R. A., & Richter, M. (2012). Effort intensity: Some insights from the cardiovascular system. In R. M. Ryan (Ed.), The Oxford Handbook of Human Motivation (p. 420‑438). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780195399820.013.0024
Gendolla, G. H. E., Wright, R. A., & Richter, M. (2019). Advancing issues in motivation intensity research: Updated insights from the cardiovascular system. In R. M. Ryan (Ed.), The Oxford Handbook of Human Motivation (2nd.ed). (p. 373–392). Oxford University Press.
Gold, J. M., Strauss, G. P., Waltz, J. A., Robinson, B. M., Brown, J. K., & Frank, M. J. (2013). Negative symptoms of schizophrenia are associated with abnormal effort-cost computations. Biological Psychiatry, 74(2), 130–136. https://doi.org/10.1016/j.biopsych.2012.12.022
Granholm, E., Verney, S. P., Perivoliotis, D., & Miura, T. (2007). Effortful cognitive resource allocation and negative symptom severity in chronic schizophrenia. Schizophrenia Bulletin, 33(3), 831–842. https://doi.org/10.1093/schbul/sbl040
Granholm, E., Ruiz, I., Gallegos-Rodriguez, Y., Holden, J., & Link, P. C. (2016). Pupillary responses as a biomarker of diminished effort associated with defeatist attitudes and negative symptoms in schizophrenia. Biological Psychiatry, 80(8), 581–588. https://doi.org/10.1016/j.biopsych.2015.08.037
Grant, P. M., Best, M. W., & Beck, A. T. (2019). The meaning of group differences in cognitive test performance. World Psychiatry, 18(2), 163–164. https://doi.org/10.1002/wps.20645
Green, D. M., & Swets, J. A. (1966). Signal Detection Theory and Psychophysics (p. xi, 455). Oxford, England: John Wiley.
Kay, S. R., Fiszbein, A., & Opler, L. A. (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2), 261–276. https://doi.org/10.1093/schbul/13.2.261
Knoop, H., van der Meer, J. W. M., & Bleijenberg, G. (2008). Guided self-instructions for people with chronic fatigue syndrome: Randomised controlled trial. The British Journal of Psychiatry, 193(4), 340–341. https://doi.org/10.1192/bjp.bp.108.051292
Kreis, I., Moritz, S., & Pfuhl, G. (2020). Objective versus subjective effort in schizophrenia. Frontiers in Psychology, 11. https://doi.org/10.3389/fpsyg.2020.01469
Kring, A. M., Gur, R. E., Blanchard, J. J., Horan, W. P., & Reise, S. P. (2013). The Clinical Assessment Interview for Negative Symptoms (CAINS): Final development and validation. The American Journal of Psychiatry, 170(2), 165–172. https://doi.org/10.1176/appi.ajp.2012.12010109
Leucht, S., Samara, M., Heres, S., Patel, M. X., Furukawa, T., Cipriani, A., … Davis, J. M. (2015). Dose equivalents for second-generation antipsychotic drugs : The classical mean dose method. Schizophrenia Bulletin, 41(6), 1397-1402. https://doi.org/10.1093/schbul/sbv037
Levick, J. R. (2003). An Introduction to Cardiovascular Physiology. London; New York: Arnold; Distributed in the United States of America by Oxford University Press.
Llabre, M. M., Spitzer, S. B., Saab, P. G., Ironson, G. H., & Schneiderman, N. (1991). The reliability and specificity of delta versus residualized change as measures of cardiovascular reactivity to behavioral challenges. Psychophysiology, 28(6), 701–711. https://doi.org/10.1111/j.1469-8986.1991.tb01017.x
Matthews, G., Jones, D. M., & Chamberlain, A. G. (1990). Refining the measurement of mood : The UWIST Mood Adjective Checklist. British Journal of Psychology, 81(1), 17–42. https://doi.org/10.1111/j.2044-8295.1990.tb02343.x
McGovern, J. E., Reddy, L. F., Reavis, E. A., & Green, M. F. (2020). Pupillary change on a cognitive effort task in schizophrenia : Associations with cognition and motivation. International Journal of Psychophysiology, 155, 1–7. https://doi.org/10.1016/j.ijpsycho.2020.05.003
Moritz, S., Klein, J. P., Desler, T., Lill, H., Gallinat, J., & Schneider, B. C. (2017). Neurocognitive deficits in schizophrenia. Are we making mountains out of molehills? Psychological Medicine, 47(15), 2602‑2612. https://doi.org/10.1017/S0033291717000939
Obrist, P. A. (1981). Cardiovascular Psychophysiology : A Perspective. Springer US. https://doi.org/10.1007/978-1-4684-8491-5
Papillo, J. F., & Shapiro, D. (1990). The cardiovascular system. Principles of Psychophysiology: Physical, Social, and Inferential Elements (pp. 456–512). Cambridge University Press.
Raffard, S., Lebrun, C., Bayard, S., Macgregor, A., & Capdevielle, D. (2020). Self-awareness deficits of cognitive impairment in individuals with schizophrenia Really? Frontiers in Psychiatry, 11, 731. https://doi.org/10.3389/fpsyt.2020.00731
Raffard, S., Rainteau, N., Bayard, S., Laraki, Y., Norton, J., & Capdevielle, D. (2020b). Assessment of the efficacy of a fatigue management therapy in schizophrenia: Study protocol for a randomized, controlled multi-centered study (ENERGY). Trials, 21(1), 797. https://doi.org/10.1186/s13063-020-04606-6
Reddy, L. F., Horan, W. P., Barch, D. M., Buchanan, R. W., Gold, J. M., Marder, S. R., … Green, M. F. (2018a). Understanding the association between negative symptoms and performance on effort-based decision-making tasks: The importance of defeatist performance beliefs. Schizophrenia Bulletin, 44(6), 1217‑1226. https://doi.org/10.1093/schbul/sbx156
Reddy, L. F., Reavis, E. A., Wynn, J. K., & Green, M. F. (2018b). Pupillary responses to a cognitive effort task in schizophrenia. Schizophrenia Research, 199, 53–57. https://doi.org/10.1016/j.schres.2018.03.005
Richter, M., Friedrich, A., & Gendolla, G. H. (2008). Task difficulty effects on cardiac activity. Psychophysiology, 45(5), 869–875. https://doi.org/10.1111/j.1469-8986.2008.00688.x
Richter, M., Gendolla, G. H. E., & Wright, R. A. (2016). Three decades of research on motivational intensity theory: What we have learned about effort and what we still don’t know. Advances in Motivation Science, 3, 149–186. https://doi.org/10.1016/bs.adms.2016.02.001
Sheehan, D. (2016). The MINI international neuropsychiatric interview (Version 7.0.2) for DSM-5.
Silvia, P. J., Nusbaum, E. C., Eddington, K. M., Beaty, R. E., & Kwapil, T. R. (2014). Effort deficits and depression: The influence of anhedonic depressive symptoms on cardiac autonomic activity during a mental challenge. Motivation and Emotion, 38(6), 779–789. https://doi.org/10.1007/s11031-014-9443-0
Silvia, P. J., Mironovová, Z., McHone, A. N., Sperry, S. H., Harper, K. L., Kwapil, T. R., & Eddington, K. M. (2016). Do depressive symptoms “blunt” effort? An analysis of cardiac engagement and withdrawal for an increasingly difficult task. Biological Psychology, 118, 52–60. https://doi.org/10.1016/j.biopsycho.2016.04.068
Strauss, G. P., & Gold, J. M. (2016). A psychometric comparison of the clinical assessment interview for negative symptoms and the brief negative symptom scale. Schizophrenia Bulletin, 42(6), 1384–1394. https://doi.org/10.1093/schbul/sbw046
Strauss, G. P., Keller, W. R., Buchanan, R. W., Gold, J. M., Fischer, B. A., McMahon, R. P., … Kirkpatrick, B. (2012). Next-generation negative symptom assessment for clinical trials: Validation of the Brief Negative Symptom Scale. Schizophrenia Research, 142(1), 88‑92. https://doi.org/10.1016/j.schres.2012.10.012
Strauss, G. P., Whearty, K. M., Morra, L. F., Sullivan, S. K., Ossenfort, K. L., & Frost, K. H. (2016). Avolition in schizophrenia is associated with reduced willingness to expend effort for reward on a Progressive Ratio task. Schizophrenia Research, 170(1), 198–204. https://doi.org/10.1016/j.schres.2015.12.006
Strauss, G. P., Waltz, J. A., & Gold, J. M. (2014). A review of reward processing and motivational impairment in schizophrenia. Schizophrenia Bulletin, 40(Suppl_2), S107‑S116. https://doi.org/10.1093/schbul/sbt197
van den Bosch, R. J., & Rombouts, R. P. (1997). Coping and cognition in schizophrenia and depression. Comprehensive Psychiatry, 38(6), 341–344. https://doi.org/10.1016/s0010-440x(97)90930-5
Waters, F., Naik, N., & Rock, D. (2013). Sleep, fatigue, and functional health in psychotic patients. Schizophrenia Research and Treatment, 2013. https://doi.org/10.1155/2013/425826
Wechsler, D. (2008). Wechsler Adult Intelligence Scale-Fourth Edition (WAIS–IV). NCS Pearson, 22, 498.
Weston, R., & Gore, P. A. (2006). A brief guide to structural equation modeling. The Counseling Psychologist, 34(5), 719–751. https://doi.org/10.1177/0011000006286345
Wolf, D. H., Satterthwaite, T. D., Kantrowitz, J. J., Katchmar, N., Vandekar, L., Elliott, M. A., & Ruparel, K. (2014). Amotivation in schizophrenia: Integrated assessment with behavioral, clinical, and imaging measures. Schizophrenia Bulletin, 40(6), 1328–1337. https://doi.org/10.1093/schbul/sbu026
Wright, R. A. (1996). Brehm’s theory of motivation as a model of effort and cardiovascular response. The psychology of action: Linking cognition and motivation to behavior (pp. 424–453). Guilford Press.
Wright, R. A. (2014). Presidential address 2013: Fatigue influence on effort—considering implications for self-regulatory restraint. Motivation and Emotion, 38(2), 183–195. https://doi.org/10.1007/s11031-014-9406-5
Wright, R., & Kirby, L. (2001). Effort determination of cardiovascular response: An integrative analysis with applications in social psychology. Advances in Experimental Social Psychology, 33, 255–307.
Wright, R. A., & Stewart, C. C. (2012). Multifaceted effects of fatigue on effort and associated cardiovascular responses. In How motivation affects cardiovascular response: Mechanisms and applications (p. 199–218). Washington, DC, US: American Psychological Association. https://doi.org/10.1037/13090-010
Acknowledgements
We wish to thank the participants who volunteered for this research, Aline Deat for her help in the recruitment process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Décombe, A., Brinkmann, K., Merenciano, M. et al. Cognitive effort in Schizophrenia: Dissimilar effects on cardiovascular activity and subjective effort. Curr Psychol 42, 20737–20747 (2023). https://doi.org/10.1007/s12144-022-03145-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-022-03145-4