Abstract
Public stigma is one of barriers for help-seeking of people with depression, which can be predicted by psychosocial causal beliefs. The present study aimed to explore how psychosocial causal beliefs, stereotypes, and emotional reactions could affect professional help-seeking preferences. A representative community-based sample of Taiwanese adults aged 20–65 (n = 800) was recruited by a random-digit-dialing computer-assisted telephone interviewing system. Participants were asked to describe their psychosocial causal beliefs, stereotypes, emotional reactions, and professional help-seeking preferences for a person with depression described in a case vignette. Serial mediation analyses were conducted to test the direct and indirect effects of psychosocial causal beliefs on professional help-seeking preferences. Psychosocial causal beliefs were positively associated with perceived dependency, which resulted in stronger pity and, in turn, increased help-seeking preferences for mental health professionals. Psychosocial causal beliefs were positively associated with perceived dependency, which resulted in stronger fear and, in turn, increased help-seeking preferences for other medical professionals (i.e., general practitioner, and Chinese medical doctor). This study indicated that reducing negative emotions such as fear and increasing pity were likely to be useful in promoting public preferences to seek help from mental health professionals. Understanding the complex associations between causal beliefs, stereotypes, emotional reactions, and help-seeking preferences might enable further work in designing evidence-based interventions for depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression affects depressed individuals’ quality of life and has great impact on their family, as well as on society as a whole (Ferrari et al., 2013; Greenberg et al., 2015; Whiteford et al., 2013). The World Health Organization has shown that depression will be the single largest contributor to global disability. The prevalence of depression was estimated to be 4.4% of the world’s population (WHO, 2017). Likewise, depression is a significant public health problem in Taiwan. The prevalence rate of depression was approximately 8.9%. Among these subjects, 62.5% were diagnosed with major depression with a tendency for self-harm (The Department of Statistics of Ministry of Health & Welfare, 2018). Prompt initial treatment was more likely to reduce the burdens and hazards of untreated depression (Wang et al., 2007). How to seek help early for depression is thus an important public health issue.
Although depression is treatable and preventable, people do not always seek help when they suffer from depression (Wang et al., 2007). Around 40–50% of people with major depression received any formal professional help in Western countries (Puyat et al., 2016). However, a much lower proportion of Chinese people received any formal professional help for depression; only around 8–20% sought help (Liao et al., 2012; Phillips et al., 2009). Public help-seeking preferences are important, since they may shape the beliefs of individuals with depression and confidants that advise friends or family members with symptoms of depression (Moro et al., 2015). In terms of professional help-seeking preferences, most research findings suggest that psychologists are frequently preferred in Western countries, followed by psychiatrists and general practitioners (Angermeyer et al., 2009; Holzinger et al., 2011; Moro et al., 2015). In some cases, however, it has been found that the public in Western countries prefers to recommend people with depression to seek help from general practitioners rather than mental health professionals (Angermeyer, Matschinger, et al., 2013; Angermeyer, Millier, et al., 2013; Munizza et al., 2013; Picco et al., 2016). However, general practitioners might have difficulties diagnosing and treating depression (Thornicroft et al., 2007). In Chinese culture, although Chinese medicine is one of the commonly used complementary and alternative medicine therapies for major depression (Wong et al., 2017), the limited number of studies on Chinese medicine pattern-based treatment of depression and low methodological quality makes it difficult to form a conclusion regarding the benefits of Chinese medicine as a treatment for depression (Yeung et al., 2015). Accordingly, there is a disparity between evidence-based treatment strategies and public opinion (Angermeyer Matschinger, & Schomerus, 2013; Angermeyer, Millier, et al., 2013; Holzinger et al., 2011; Munizza et al., 2013). It is therefore crucial to understand the factors that may influence professional help-seeking preferences for depression.
The general public tends to regard depression as being caused by environmental or situational factors, benefitting mostly from psychotherapy and alternative treatments (Angermeyer & Matschinger, 2003a; Angermeyer, Matschinger, et al., 2013; Angermeyer, Millier, et al., 2013). To better understand and explain the mechanisms leading to psychosocial causal beliefs (i.e., stress situations such as family quarrels, financial/ working difficulties, and childhood problems such as being abused or having lost a parent as little child), stigma and help-seeking preferences, attribution theory provides a model of causal understanding of events that has implications for individuals’ attitudes (Weiner et al., 1988). Controllability is one of the attribution related to mental illness stigma (Corrigan, 2000). Controllability refers to the amount of volitional control individuals can exert over their illnesses. When the symptoms of mental illness are thought to controllable by the individuals, it raises negative emotions (e.g., anger and fear) and rejection from the public in Western countries (Corrigan, 2000; Weiner et al., 1988). Conversely, if onset of symptoms is deemed uncontrollable, it may arouse positive emotion (i.e., sympathy) and provide help (Corrigan, 2000; Weiner et al., 1988). Psychosocial causal beliefs rather than biomedical beliefs on mental illness have been found to be positively associated with controllability in Chinese public (Mak et al., 2014). Biomedical causal beliefs on depression were clearly associated with help-seeking preferences for mental health professionals such as psychiatrists and psychologists (Pescosolido et al., 2010; Schomerus et al., 2012; Tompkins et al., 2017), while the mixed picture emerged with regard to psychosocial causal beliefs. A number of studies have found that people who attribute depression to psychosocial causes are more likely to recommend help from mental health professionals, while other studies have found that psychosocial causal beliefs are more likely to recommend help from general practitioners and Chinese medicine (Boge et al., 2018; Nortje et al., 2016; Speerforck et al., 2017). Previous studies indicated that endorsement of psychosocial causes of depression remained unchanged at a high level, especially in the Asian cultural sphere (Angermeyer et al., 2009; Schomerus et al., 2012). However, several key questions remain unanswered. Firstly, evidence was mostly lacking for non-Western groups (Hagmayer & Engelmann, 2014). Secondly, it is still unknown how psychosocial causal beliefs influence help-seeking preferences for mental health professionals and for other medical professionals differentially. Previous studies have suggested that public stigma (i.e., stereotypes or emotional reactions) might mediate the association of psychosocial causal beliefs with behavioral outcomes (Mak et al., 2014; Schnyder et al., 2018). Studies on the mediation effect of public stigma between psychosocial causal beliefs and professional help-seeking preferences are still lacking. Therefore, the mediating influence of public stigma on psychosocial causal beliefs warrants addressing.
Public stigma is one of the most important barriers to help-seeking and is particularly profound among Chinese communities (Clement et al., 2015). However, evidence for the association between public stigma and professional help-seeking preferences is limited. Only one study indicated that anger toward people with depression was associated to fewer recommendations to seek help from mental health professionals, while fear was positively correlated with help-seeking preferences for mental health professionals (Speerforck et al., 2017). Public stigma is defined as the public endorsement of stereotypes about mental illness that leads to the public’s negative emotions, such as fear, against people who have a mental illness, and even worse, may lead to rejection, avoidance, discrimination, and status loss (Corrigan, 2016; Parcesepe & Cabassa, 2013). A quarter of the general public perceives people with depression as dangerous, while more than half of the general public considers them to be unpredictable and dependent on other people (Aromaa et al., 2011; Lien & Kao, 2019). Endorsing the stereotypes has a positive effect on the emotional reactions (e.g., anger and fear) of the public in Western countries (Angermeyer & Matschinger, 2003a; Makowski et al., 2016). Social attribution theory has shown that stereotypes of dangerousness may induce an emotional response such as fear, increasing discriminatory behavior (e.g., withholding help) (Corrigan et al., 2003). A review article indicated that the public’s emotional reaction to people with mental illnesses may be an area that needs more attention (Wei et al., 2015). While the stigma of severe mental disorders has remained unchanged or even worsened over the last two decades, the public in Western countries readiness to recommend help-seeking from mental health professionals has increased (Angermeyer, Matschinger, et al., 2013; Pescosolido et al., 2010). Therefore, a deeper understanding of professional help-seeking preferences within the Chinese society and their relation to psychosocial causal beliefs, stereotypes, and emotional reactions is necessary.
Aims
The aims of this study were to (a) examine the associations between the public’s psychosocial causal beliefs and stereotypes, emotional reactions, and help-seeking preferences; (b) examine the mediating role of stereotypes (i.e., perceived dangerousness and perceived dependency) on the relation between psychosocial causal beliefs and help-seeking preferences; (c) examine the mediating role of emotional reactions (i.e., anger, pity, and fear) on the relation between psychosocial causal beliefs and help-seeking preferences; and (d) examine the serial mediating roles of stereotypes and emotional reactions on the relation between psychosocial causal beliefs and help-seeking preferences.
Method
Participants
During October and November of 2016, cross-sectional data were obtained through a random-digit-dialing computer-assisted telephone interview (CATI) survey by a telephone research company in Taiwan. The computer-assisted telephone interviews (CATI) was successfully used previously in a population-based attitude research in psychiatry (Cook & Wang, 2011). In order to increase reliability and counteract possible interviewer effects, personal, fully structured interviews were carried out by well-trained employees of a large Taiwanese opinion polling firm, all of whom were fluent in the local language (i.e., Mandarin or Taiwanese). In this study, we recruited 800 participants (response rate of 74.6% at an individual level) between the ages of 20 and 65. The sample size for this study was calculated to be 784 adults with a 95% confidence level and a 3.5% confidence interval. The present study included 800 adults, which has appropriate sample size. A stratified and clustered multistage random sampling process according to gender, age (i.e., 20–30, 31–30, 41–50, 51–65 years) and geographic location was used to select the respondents. With regards to sex, age, and geographical areas, the sampling was comparable with the whole population aged 20 to 65 years in 2016. Prior to data collection, ethical approval was obtained from the local Institutional Review Board in Taiwan. Further detailed information about the sampling procedures can be found in a previous publication (Lien & Kao, 2019).
Instruments
Case Vignette
The interview was based on presenting a case vignette describing a male (‘Daxiong’) or a female (‘Mei’) with major depression, according to the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition criteria (Association, 2013), without use of clinical terminology. The vignette had been submitted to four psychiatrists or psychologists for blind diagnostic allocation before use. All experts arrived at the correct diagnosis based on the case’s history. The gender of the person described in the vignette was systemically varied, where 50% of the cases presented were female. The name ‘Daxiong’ or ‘Mei’ was randomly assigned to minimize potential bias related to the sex of the person in the case vignette.
Psychosocial Causal Beliefs
After presenting the case vignette, the respondents were asked to respond to two items and rate each as a likely or unlikely cause for the person described in the vignette. For each question, respondents were asked to rate the cause as ‘likely’, ‘not likely’, or ‘I don’t know’. The answer of ‘likely’ was used as an indicator for the endorsement of psychosocial causal belief (1 versus 0). The psychosocial causal beliefs items were: (1) stress situations such as family quarrels, financial/ working difficulties, and (2) childhood problems such as being abused or having lost a parent as little child. A sum score of each item was used for subsequent analyses, with higher scores indicating greater psychosocial causal beliefs. This scale was adapted from previous study used by Cook and Wang (Cook & Wang, 2011). A significant correlation between these two items was obtained in the present study (r = 0.18, p < 0.01).
Stereotypes
Stereotypes were assessed using the Personal Attributes Scale (PAS) (Ellison et al., 2015). Four items covering two major stereotypes were selected in this study: perceived dangerousness (2 items) and perceived dependency (2 items). The perceived dangerousness items were: (1) the vignette person is dangerous and (2) the vignette person is aggressive or violent. The perceived dependency items were: (1) the vignette person is helpless, and (2) the vignette person depends on other people. Participants were asked to rate on a 5-point Likert-type scale (1 = strongly disagree, 5 = strongly agree) which assessed their personal attitudes toward the person described in the vignette. For our analysis, the sum score of the two types of stereotypes (i.e., perceived dangerousness and perceived dependency) were used, respectively, with higher scores indicating an endorsement of negative stereotypes. Significant correlations were found between two items for perceived dangerousness (r = 0.53, p < 0.01) and perceived dependency (r = 0.27, p < 0.01), respectively.
Emotional Reactions
According to previous studies (Angermeyer & Matschinger, 2003b; Ellison et al., 2015), three main types of emotional reactions to people with mental illness could be distinguished: fear, pity, and anger. To assess subjects’ emotional reactions, a list of five items was used to assess the respondents' emotional reactions to the person described in the vignette. Participants were asked to rate their emotional reactions on a five-point Likert scale from 1 = ‘strongly disagree’ to 5 = ’strongly agree’. The one fear item was: the vignette person scares me. The two pity items were: (1) I feel sympathy and (2) I feel the need to help. The two anger items were: (1) I react angrily or feel annoyed and (2) I react with incomprehension. For our analysis, a sum score of each type of emotional reaction was used indicating fear, pity, and anger reaction, respectively, with higher scores indicating stronger fear, pity, and anger reaction. In the present study, significant correlations were found between items for anger (r = 0.28, p < 0.01) and pity (r = 0.33, p < 0.01).
Professional Help-Seeking Preferences
Professional help-seeking preferences were assessed by means of the following open-ended question: “Who do you think the person in the vignette should seek help from?” Several choices of types of help were offered, including a general practitioner, psychiatrist, psychologist, or counselor. To explore the cultural dimension of Chinese respondents’ beliefs on professional help and treatment methods, ‘Chinese medical doctor’ was added to the list of choices. For each question, respondents were asked to rate their preference on a 5-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. In this study, professional help-seeking preferences were divided into two groups, mental health professionals (i.e., psychiatrists, psychologists, or counselors) and other medical professionals (i.e., general practitioners and Chinese medical doctors). For our analysis, a sum score of each group were used, with higher scores indicating stronger recommendations. In the present study, significant correlations were found between items for help-seeking preferences for mental health professionals (r = 0.41, p < 0.01) and help-seeking preferences for other medical professionals (r = 0.22, p < 0.01).
Socio-Demographic Characteristics
Information regarding the participants’ sex, age, and educational attainments, marital status, family incomes, and their place of residence was collected.
Analysis
All statistical analyses were performed using the SPSS version 23.0. First, we imputed missing scale values using the participants’ mean if 25% or less of the item responses were missing (Roth, Switzer, and Switzer 1999). Thus, we imputed the family incomes levels of 21 participants (2.63%). Second, we tested the association between baseline social-demographic characteristics and help-seeking preferences via Student's t-tests, ANOVA, and Pearson's correlations. Third, zero-order relations among study variables were examined with Pearson's correlations. Fourth, in order to further test whether both types of stereotypes (i.e., perceived dangerousness and perceived dependency) and emotional reactions mediated the effects of psychosocial causal beliefs on both types of professional help-seeking preferences, four separate mediation analyses were conducted using model 81 (enabling tests of serial mediation models) of the PROCESS macro in SPSS (Hayes, 2017). This provided indirect effect estimates for serial multiple mediators, standard errors, and confidence intervals derived from the bootstrap distribution with 5,000 bootstrap estimates. Mediation models assessed the indirect effects without needing the relation between the independent and dependent variables to be significant (Hayes, 2017). Bootstrapped CIs have been seen to be superior to the standard forms of estimating the SEs of indirect effects (Hayes, 2017). An indirect effect was significant if the CI did not include the 0 value.
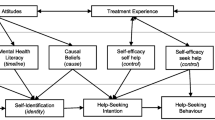
As shown in Fig. 1, psychosocial causal beliefs were independent variables, stereotypes (i.e., perceived dangerousness and perceived dependency) were primary mediators, and emotional reactions (i.e., anger, pity, and fear) were secondary mediating variables. Help-seeking preferences for mental health professionals (Mediation Analysis 1, 2) and help-seeking preferences for other medical professionals (Mediation Analysis 3, 4) were dependent variables. To further establish the validity of the model, biomedical causal beliefs (brain disorders or chemical imbalances, head injuries, and genetics/inherited causes), educational attainments, and family incomes were included as covariates.
Illustrations of conceptual model. c indicates the total effect of psychosocial causal beliefs on help-seeking preferences. c′ indicates the direct effect of psychosocial causal beliefs on help-seeking preferences. a1 indicates the direct effect of psychosocial causal beliefs on stereotypes. a2 indicates the direct effect of psychosocial causal beliefs on anger. a3 indicates the direct effect of psychosocial causal beliefs on pity. a4 indicates the direct effect of psychosocial causal beliefs on fear. b1 indicates the direct effect of stereotypes on help-seeking preferences. b2 indicates the direct effect of anger on help-seeking preferences. b3 indicates the direct effect of pity on help-seeking preferences. b4 indicates the direct effect of fear on help-seeking preferences. d21 indicates the direct effect of stereotypes on anger. d31 indicates the direct effect of stereotypes on pity. d41 indicates the direct effect of stereotypes on fear
Results
Descriptive Statistics of Public Beliefs and Attitudes Towards Depression
The public beliefs and attitudes towards depression as well as the descriptive statistics of the 800 participants are provided in Table 1. In other areas of stigma research, it has been suggested that high scores could be defined as above the midpoint of the possible range, and higher scores represented a greater endorsement of that variable (Ellison et al., 2015; Ritsher & Phelan, 2004). Psychosocial causes were highly endorsed for depression (mean = 1.41, mid-point = 1.00). The mean scores of perceived dangerousness were equal to the mid-point (mean = 6.00, mid-point = 6.00) and perceived dependency were above the mid-point (mean = 8.04, mid-point = 6.00). These findings indicated a high degree of public stigma such as perceived dependency toward depression. The predominant emotional reaction towards depression was pity (mean = 8.36, midpoint = 6.00), with fear (mean = 2.62, midpoint = 3.00) and anger (mean = 5.09, midpoint = 6.00) seen less frequently. The public showed high help-seeking preferences for both mental health professionals and other medical professionals, with mental health professionals (mean = 8.75, midpoint = 6.00) endorsed most frequently, followed by other medical professionals (mean = 6.29, midpoint = 6.00). Regarding the normal distribution, all variables stayed under the critical value of 7 for kurtosis and 2 for skewness (Mardia & Foster, 1983).
Correlation Analysis
There were several significant associations between help-seeking preferences and baseline social-demographic characteristics. Educational attainments were positively correlated with help-seeking preferences for mental health professionals (r = 0.11, p < 0.01), while educational attainments were negatively correlated with help-seeking preferences for other medical professionals (r = -0.08, p < 0.05). Furthermore, higher family incomes were significantly correlated with more preferable to help-seeking for mental health professionals (r = 0.08, p < 0.05).
The zero-order correlations of all study variables are shown in Table 1. Higher levels of psychosocial causal beliefs were associated with higher levels of both types of stereotypes (perceived dangerousness and perceived dependency). In addition, psychosocial causal beliefs exhibited significantly positive association with one of the emotional reactions (i.e., pity). With regard to the correlations between stereotypes and emotional reactions, higher levels of two types of stereotypes (i.e., perceived dangerousness and perceived dependency) were positively associated with negative emotional reactions (i.e., anger and fear). In addition, perceived dependency was positively associated with positive emotional reactions (i.e., pity). With regard to the associations between public stigma variables (i.e., stereotypes and emotional reactions) and help-seeking preferences, the results indicated that higher levels of the two types of stereotypes (i.e., perceived dangerousness and perceived dependency) and stronger emotional reactions such as pity and fear were correlated with higher help-seeking preferences for mental health professionals. Furthermore, perceived dependency and three types of emotional reactions were positively correlated with help-seeking preferences for other medical professionals.
Mediation Analysis
The results from the simple mediation and serial mediation associations are displayed in Table 2 and Table 3. There were three paths that showed significant indirect associations between psychosocial causal beliefs and help-seeking preferences for mental health professionals among the mediation models (Table 2). Only one path showed a significant indirect association between psychosocial causal beliefs and help-seeking preferences for other medical professionals among the mediation models (Table 3). Furthermore, all direct effects (c') and total effects (c) of psychosocial causal beliefs on both help-seeking preferences for mental health professionals and for other medical professionals were not significant in these models. These results indicated that full mediation obtained when the predictor variable (psychosocial causal beliefs) had no significant effect on the outcome variables (help-seeking preferences for mental health professionals and for other medical professionals).
Indirect and Serial Indirect Effects of Psychosocial Causal Beliefs on Help-Seeking Preferences for Mental Health Professionals
As shown in Table 2, the indirect effects of psychosocial causal beliefs on help-seeking preferences for mental health professionals mediated by perceived dependency were significant. The results indicated that greater psychosocial causal beliefs were associated with higher levels of perceived dependency that, in turn, were related to greater help-seeking preferences for mental health professionals. The result also indicated that pity was a significant mediator in the relationships between psychosocial causal beliefs and help-seeking preferences for mental health professionals. In other words, greater psychosocial causal beliefs led to emotional reactions such as pity, which resulted in greater help-seeking preferences for mental health professionals.
With regard to serial mediation effects of psychosocial causal beliefs on help-seeking preferences for mental health professionals, our results provided evidence of serial mediation when the paths included perceived dependency as a proximal mediator and pity as a distal mediator. The results demonstrated that psychosocial causal beliefs led to perceived dependency, which resulted in stronger pity and, in turn, increased help-seeking preferences for mental health professionals.
Indirect and Serial Indirect Effects of Psychosocial Causal Beliefs on Help-Seeking Preferences for Other Medical Professionals
As shown in Table 3, concerning serial mediation effects of psychosocial causal beliefs on help-seeking preferences for other medical professionals, significant serial indirect effects were found when the paths included perceived dependency as a proximal mediator and fear as a distal mediator. The results demonstrated that psychosocial causal beliefs led to perceived dependency, which resulted in stronger fear and, in turn, increased help-seeking preferences for other medical professionals.
Discussion
Before discussed our findings, there were few limitations should be noted. First, our data were collected cross-sectionally, so we could not reject the possibility of reverse causation. Future studies should examine our model with longitudinal data to better understand the pathways and causal relationships. Although our model proceeds in a logical fashion, alternative models are possible. Second, the use of a vignette to prompt discussion may not reflect the real attitude and behavior of individuals in actual situations of depression. However, we used an unlabeled case vignette in order to avoid a possible bias due to the use of any medical language within the interview. Third, the self-reported nature of the data might be biased by social desirability, where respondents could have responded to the interview questions in a way that makes them appear socially desirable, and therefore they might not actually have responded according to their true reactions. Of note, this seems to be less a problem in telephone surveys than in face-to-face interviews (Midanik et al., 2001). Fourth, the small number of items in some scales, notably the emotional reactions of fear, and the binary nature of the independent variable such as psychosocial causal beliefs scale, limits their usefulness. Finally, although our study was based on a large population survey representative of the Taiwan population, results might differ in other sociocultural contexts. Nevertheless, our cross-sectional design recruited data from the Eastern society in order to address the lack of evidence from non-Western countries.
To the best of our knowledge, this is the first study examining the relationship between different dimensions of stigma (i.e., stereotypes and emotional reactions), psychosocial causal beliefs, and professional help-seeking preferences among the Chinese public. This study has confirmed that perceived dependency stereotypes and emotional reactions (i.e., pity and fear) play a significant role in the stigma process in depression. Therefore, our findings could be especially helpful in designing interventions for reducing public stigma and increasing help-seeking preferences for mental health professionals. More generally, regarding the type of help-seeking preferences in general, population surveys from Singapore (Picco et al., 2016), Vietnam (Boge et al., 2018), Taiwan (Lien & Kao, 2019), French (Angermeyer, Matschinger, et al., 2013; Angermeyer, Millier, et al., 2013), Germany, Slovak Republic and Russia (Angermeyer et al., 2005) consistently showed that the lay public favored informal resources (such as family and confidant) over formal resources for depression. Our findings have important implications because informal sources of help should have adequate skills, knowledge, and mental health literacy to recognize mental health issues and to recommend mental health professional sources of help without having stigmatizing attitudes.
Our results supported the hypothesis that stereotypes of perceived dependency were significant mediators linking psychosocial causal beliefs and help-seeking preferences for mental health professionals. Specifically, among the public attitudes and beliefs of individuals with depression, greater psychosocial causal beliefs were associated with higher levels of perceived dependency that, in turn, led to more recommendations to seek help from mental health professionals. One potential explanation for this finding is that the perception of individuals with depression as dependent might lead the public to perceive depression as a more severe and disabling condition (i.e., having a poorer prognosis), and as a result, leads them to recommend mental health professionals more frequently. Previous studies have shown that when the public or the health professionals regarded individuals with physiological diseases as dependent, they were perceived as having a poorer prognosis and as needing more help from mental health professionals (Nordholm & Westbrook, 2010; Westbrook et al., 1984). Thus, interventions such as anti-stigma campaigns and educational programs might benefit from a more refined understanding of the anticipated prognosis (e.g., the prognosis without treatment or under optimal treatment) toward people with depression. However, in the context of mental health, the relationship between perceived dependency, anticipated prognosis, and help-seeking preferences is unclear. Future research examining the role of perceived dependency in predicting anticipated prognoses is required to clarify the associations and the underlying mechanisms.
Similar to previous study (Pattyn et al., 2013), this study found that psychosocial causal beliefs had positive indirect effects on the help-seeking preferences for mental health professionals (through the mediating effect of pity). The results of this study further support the importance of obtaining positive emotional reactions (such as pity) from the public for people with depressive disorders. It is therefore important that interventions in depression also focus on fostering beliefs with increased pity, as opposed to solely aiming to reduce negative stereotypes, an idea echoed in literature on effective anti-stigma interventions (Heijnders & Van Der Meij, 2006). In the current study, anger was not a significant mediator in the relationship between psychosocial causal beliefs and help-seeking preferences. Thus, the same conclusion can be drawn from the previous studies with regard to other disorders, in which anger was not a useful target during interventions (Angermeyer & Matschinger, 2003a, b; Ellison et al., 2015).
Interestingly, the current study found that perceived dependency would mediate the relationships between psychosocial causal beliefs and help-seeking preferences for mental health professionals. Furthermore, our serial mediation effect results extended prior research by showing that when the paths included the negative emotional reactions such as fear as the distal mediators, one could actually predict higher help-seeking preferences for other medical professionals, rather than mental health professionals. These findings have both theoretical and practical implications. In addition to Corrigan's model of public stigma, which showed that negative emotions are linked to discrimination (Corrigan, 2016; Corrigan et al., 2014), our serial mediation effect results add evidence to support that negative emotions may lead others to recommend that people with depression seek help from other medical professionals. A meta-analysis study indicated that the Chinese public's level of recognition of depression is low (Li & Reavley, 2020), which means that the public might have improper or insufficient knowledge about depression (Corrigan et al., 2014). Thus, the public would perceive people with depression as dependent, which in turn would lead to the public’s negative emotional reactions such as fear (Corrigan et al., 2014). Furthermore, the Chinese public had little knowledge on mental health treatment options, even though they agreed that one should seek professional help for mental illnesses (Li & Reavley, 2020; Wong et al., 2017). As a result, the public would suggest that people with depression should seek help from other medical professionals. Finally, we also found that although the public perceived the people with depression as dependent, the public would suggest that they seek help from mental health professionals when the public felt pity toward them. Our study found that fear and pity are linked to distinct types of professional help-seeking preferences. Previous studies also indicated that perceived dependency increased both fear and pity simultaneously, which had a competing effect on social distance (Angermeyer & Matschinger, 2003a, b). The serial mediation analyses further emphasize that the perception of increased pity and decreased fear toward people with depression should be considered when designing anti-stigma interventions for the public.
Conclusions
In conclusion, we hope to have been able to demonstrate the usefulness of the theoretical concept applied in this study. As our findings indicate, stereotypes and emotional reactions toward depression exist differential serial mediating effects on the relationships between psychosocial causal beliefs and help-seeking preferences for mental health professionals and for other medical professionals. This appears important not only on theoretical grounds. It may be even more important for practical reasons. These findings suggest that discussing the information and involving patients and their families in decision making for help seeking is important for effective management of depression. We would like to emphasize that successful anti-stigma interventions for depression should acknowledge psychosocial causal beliefs, stereotypes, and emotional reactions, all of which play a vital role in promoting public recommendations to seek help from mental health professionals. Understanding these complexity of the stigma process might enable us to further improve interventions for depression and potentially further prevent relapses of depression.
References
Angermeyer, M. C., Breier, P., Dietrich, S., Kenzine, D., & Matschinger, H. (2005). “Public attitudes toward psychiatric treatment An International Comparison.” Social Psychiatry and Psychiatric Epidemiology, 40, 855–864.
Angermeyer, M. C., Holzinger, A., & Matschinger, H. (2009). Mental health literacy and attitude towards people with mental illness: A trend analysis based on population surveys in the eastern part of Germany. European Psychiatry, 24, 225–232.
Angermeyer, M. C., & Matschinger, H. (2003). Public beliefs about schizophrenia and depression: Similarities and differences. Social Psychiatry and Psychiatric Epidemiology, 38, 526–534.
Angermeyer, M. C., & Matschinger, H. (2003). The stigma of mental illness: Effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatrica Scandinavica, 108, 304–309.
Angermeyer, M. C., Matschinger, H., & Schomerus, G. (2013). Attitudes towards psychiatric treatment and people with mental illness: Changes over two decades. The British Journal of Psychiatry, 203, 146–151.
Angermeyer, M. C., Millier, A., Remuzat, C., Refai, T., & Toumi, M. (2013). Attitudes and beliefs of the French public about schizophrenia and major depression: Results from a vignette-based population survey. BMC Psychiatry, 13, 313.
Aromaa, E., Tolvanen, A., Tuulari, J., & Wahlbeck, K. (2011). Personal stigma and use of mental health services among people with depression in a general population in Finland. BMC Psychiatry, 11, 52.
Association, A. P. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC.
Boge, K., Hahn, E., Cao, T. D., Fuchs, L. M., Martensen, L. K., Schomerus, G., Dettling, M., Angermeyer, M., Nguyen, V. T., & Ta, T. M. T. (2018). Treatment recommendation differences for schizophrenia and major depression: A population-based study in a Vietnamese cohort. International Journal of Mental Health Systems, 12, 70.
Clement, S., Schauman, O., Graham, T., Maggioni, F., Evans-Lacko, S., Bezborodovs, N., Morgan, C., Rusch, N., Brown, J. S., & Thornicroft, G. (2015). ’What is the impact of mental health-related stigma on help-seeking? A Systematic Review of Quantitative and Qualitative Studies’, Psychological Medicine, 45, 11–27.
Cook, T. M., & Wang, J. (2011). Causation beliefs and stigma against depression: Results from a population-based study. Journal of Affective Disorders, 133, 86–92.
Corrigan, P., Markowitz, F. E., Watson, A., Rowan, D., & Kubiak, M. A. (2003). An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior, 44, 162–179.
Corrigan, P. W. (2000). Mental health stigma as social attribution: Implications for research methods and attitude change. Clinical Psychology: Science and Practice, 7, 48–67.
Corrigan, P. W. (2016). Lessons learned from unintended consequences about erasing the stigma of mental illness. World Psychiatry, 15, 67–73.
Corrigan, P. W., Druss, B. G., & Perlick, D. A. (2014). The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychological Science in the Public Interest, 15, 37–70.
Ellison, N., Mason, O., & Scior, K. (2015). Public beliefs about and attitudes towards bipolar disorder: Testing theory based models of stigma. Journal of Affective Disorders, 175, 116–123.
Ferrari, A. J., Charlson, F. J., Norman, R. E., Patten, S. B., Freedman, G., Murray, C. J., Vos, T., & Whiteford, H. A. (2013). Burden of depressive disorders by country sex age and year: findings from the global burden of disease study 2010. PLoS Medicine, 10, e1001547.
Greenberg, P. E., Fournier, A. A., Sisitsky, T., Pike, C. T., & Kessler, R. C. (2015). The economic burden of adults with major depressive disorder in the United States (2005 and 2010). The Journal of Clinical Psychiatry, 76, 155–162.
Hagmayer, Y., & Engelmann, N. (2014). Causal beliefs about depression in different cultural groups-what do cognitive psychological theories of causal learning and reasoning predict? Frontiers in Psychology, 5, 1303.
Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). New York, NY, US.
Heijnders, M., & Van Der Meij, S. (2006). The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychology, Health & Medicine, 11, 353–363.
Holzinger, A., Matschinger, H., & Angermeyer, M. C. (2011). ’What to do about depression? Help-Seeking and Treatment Recommendations of the Public’, Epidemiology and Psychiatric Sciences, 20, 163–169.
Li, W., & Reavley, N. (2020). Recognition and beliefs about treatment for mental disorders in mainland China: A systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology, 55, 129–149.
Liao, S. C., Chen, W. J., Lee, M. B., Lung, F. W., Lai, T. J., Liu, C. Y., Lin, C. Y., Yang, M. J., & Chen, C. C. (2012). Low prevalence of major depressive disorder in Taiwanese adults: Possible explanations and implications. Psychological Medicine, 42, 1227–1237.
Lien, Y. J., & Kao, Y. C. (2019). Public beliefs and attitudes toward schizophrenia and depression in Taiwan: A nationwide survey. Psychiatry Research, 273, 435–442.
Mak, W. W. S., Chong, E. S., & Wong, C. C. (2014). Beyond attributions: Understanding public stigma of mental illness with the common sense model. American Journal of Orthopsychiatry, 84, 173–181.
Makowski, A. C., Mnich, E. E., Angermeyer, M. C., & von dem Knesebeck, O. (2016). Continuum beliefs in the stigma process regarding persons with schizophrenia and depression: results of path analyses. PeerJ, 4, e2360.
Mardia, K. V., & Foster, K. (1983). Omnibus tests of multinormality based on skewness and kurtosis. Communications in Statistics - Theory and Methods, 12, 207–221.
Midanik, L. T., Greenfield, T. K., & Rogers, J. D. (2001). Reports of alcohol-related harm: Telephone versus face-to-face interviews. Journal of Studies on Alcohol, 62, 74–78.
Moro, M. F., Angermeyer, M. C., Matschinger, H., Holzinger, A., Piras, A. P., Cutrano, F., Mura, G., & Carta, M. G. (2015). ’Whom to Ask for Professional Help in Case of Major Depression? Help-Seeking Recommendations of the Sardinian Public’, Administration and Policy in Mental Health and Mental Health Services Research, 42, 704–713.
Munizza, C., Argentero, P., Coppo, A., Tibaldi, G., Di Giannantonio, M., Picci, R. L., & Rucci, P. (2013). Public beliefs and attitudes towards depression in Italy: a national survey. PLoS One, 8, e63806.
Nordholm, L. A., & Westbrook, M. T. (2010). Effects of depression, self-blame and dependency on health professionals’ evaluation of paraplegic patients. Australian Occupational Therapy Journal, 33, 59–70.
Nortje, G., Oladeji, B., Gureje, O., & Seedat, S. (2016). Effectiveness of traditional healers in treating mental disorders: A systematic review. Lancet Psychiatry, 3, 154–170.
Parcesepe, A. M., & Cabassa, L. J. (2013). Public stigma of mental illness in the United States: A systematic literature review. Administration and Policy in Mental Health and Mental Health Services Research, 40, 384–399.
Pattyn, E., Verhaeghe, M., & Bracke, P. (2013). Attitudes toward community mental health care: The contact paradox revisited. Community Mental Health Journal, 49, 292–302.
Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., & Link, B. G. (2010). “‘A disease like any other’? A Decade of Change in Public Reactions to Schizophrenia, Depression, and Alcohol Dependence.” The American Journal of Psychiatry, 167, 1321–1330.
Phillips, M. R., Zhang, J., Shi, Q., Song, Z., Ding, Z., Pang, S., Li, X., Zhang, Y., & Wang, Z. (2009). Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: An epidemiological survey. Lancet, 373, 2041–2053.
Picco, L., Abdin, E., Chong, S. A., Pang, S., Vaingankar, J. A., Sagayadevan, V., Kwok, K. W., & Subramaniam, M. (2016). Beliefs About Help Seeking for Mental Disorders: Findings From a Mental Health Literacy Study in Singapore. Psychiatric Services, 67, 1246–1253.
Puyat, J. H., Kazanjian, A., Goldner, E. M., & Wong, H. (2016). ’How Often Do Individuals with Major Depression Receive Minimally Adequate Treatment? A Population-Based, Data Linkage Study’, Canadian Journal of Psychiatry, 61, 394–404.
Ritsher, J. B., & Phelan, J. C. (2004). Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Research, 129, 257–265.
Roth, P. L., Switzer, F. S., & Switzer, D. M. (1999). Missing Data in Multiple Item Scales: A Monte Carlo Analysis of Missing Data Techniques. Organizational Research Methods, 2, 211–232.
Schnyder, N., Michel, C., Panczak, R., Ochsenbein, S., Schimmelmann, B. G., & Schultze-Lutter, F. (2018). The interplay of etiological knowledge and mental illness stigma on healthcare utilisation in the community: A structural equation model. European Psychiatry, 51, 48–56.
Schomerus, G., Schwahn, C., Holzinger, A., Corrigan, P. W., Grabe, H. J., Carta, M. G., & Angermeyer, M. C. (2012). Evolution of public attitudes about mental illness: A systematic review and meta-analysis. Acta Psychiatrica Scandinavica, 125, 440–452.
Speerforck, S., Schomerus, G., Matschinger, H., & Angermeyer, M. C. (2017). Treatment recommendations for schizophrenia, major depression and alcohol dependence and stigmatizing attitudes of the public: Results from a German population survey. European Archives of Psychiatry and Clinical Neuroscience, 267, 341–350.
The Department of Statistics of Ministry of Health and Welfare, Taiwan. 2018. "Numbers of outpatients and inpatients with mental disorders by gender, age, and disease, year 2017." In, edited by Taiwan. The Department of Statistics of Ministry of Health and Welfare. Taiwan.
Thornicroft, G., Rose, D., & Kassam, A. (2007). Discrimination in health care against people with mental illness. International Review of Psychiatry, 19, 113–122.
Tompkins, K. A., Swift, J. K., Rousmaniere, T. G., & Whipple, J. L. (2017). The relationship between clients’ depression etiological beliefs and psychotherapy orientation preferences, expectations, and credibility beliefs. Psychotherapy (chicago, Ill.), 54, 201–206.
Wang, P. S., Angermeyer, M., Borges, G., Bruffaerts, R., Tat Chiu, W., DE Girolamo, G., Fayyad, J., Gureje, O., Haro, J. M., Huang, Y., Kessler, R. C., Kovess, V., Levinson, D., Nakane, Y., Oakley Brown, M. A., Ormel, J. H., Posada-Villa, J., Aguilar-Gaxiola, S., Alonso, J., … Ustun, T. B. (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry, 6, 177–85.
Wei, Y., McGrath, P. J., Hayden, J., & Kutcher, S. (2015). Mental health literacy measures evaluating knowledge, attitudes and help-seeking: A scoping review. BMC Psychiatry, 15, 291.
Weiner, B., Perry, R. P., & Magnusson, J. (1988). An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology, 55, 738–748.
Westbrook, M. T., Nordholm, L. A., & McGee, J. E. (1984). Cultural differences in reactions to patient behaviour: A comparison of Swedish and Australian health professionals. Social Science & Medicine, 19, 939–947.
Whiteford, H. A., Degenhardt, L., Rehm, J., Baxter, A. J., Ferrari, A. J., Erskine, H. E., Charlson, F. J., Norman, R. E., Flaxman, A. D., Johns, N., Burstein, R., Murray, C. J., & Vos, T. (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet, 382, 1575–1586.
WHO. 2017. Depression and other common mental disorders: global health estimates. (World Health Organization).
Wong, D. F. K., Cheng, C. W., Zhuang, X. Y., Ng, T. K., Pan, S. M., He, X., & Poon, A. (2017). Comparing the mental health literacy of Chinese people in Australia, China, Hong Kong and Taiwan: Implications for mental health promotion. Psychiatry Research, 256, 258–266.
Yeung, W. F., Chung, K. F., Ng, K. Y., Yu, Y. M., Zhang, S. P., Ng, B. F., & Ziea, E. T. (2015). Prescription of Chinese Herbal Medicine in Pattern-Based Traditional Chinese Medicine Treatment for Depression: A Systematic Review. Evidence-Based Complementary and Alternative Medicine, 2015, 160–189.
Funding
This study was supported by Ministry of Science and Technology, Taiwan (105–2410-H-003 -033 -SSS). The Ministry of Science and Technology of Taiwan was not involved in the study design, data collection, analysis, interpretation, and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
I-Chuan Tsai conceived the study and wrote the first draft, methodology, review and editing. Yu-Chen Kao contributed to the data acquisition, data interpretation, revising and editing the manuscript. Yin-Ju Lien contributed to the whole process of this manuscript, including the design of the study, data acquisition, data analysis, revising and editing the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The case vignette: Daxiong (or Mei) is 30 years old and is not married. He (or she) used to regularly help his (or her) father work on the store, but for the last 10–15 days, he (or she) has not been going to work. For the last 2–3 months, he (or she) has been staying alone and aloof. He (or she) has not been bathing regularly and sometimes becomes aggressive for no apparent reason. He (or she) never used to behave in this way. On several occasions, his (or her) father has found him (or her) talking to himself (or herself) when nobody else was around. He (or she) has become suspicious of others and says that people are talking about him (or her). For the last one week he (or she) has refused to eat food as he (she) suspects his (or her) food is being poisoned by the neighbors. Daxiong (or Mei) is 30 years old and was fine until six months ago when he (or she) began to feel tired all the time. He (or she) says that she is sad and has lost interest in life. Even his (or her) children and family don't make him (or her) feel happy. He (or she) cannot sleep and he (or she) has lost the taste for food, which he (or she) used to love. He (or she) has also lost interest in cooking because he (or she) can't concentrate. Sometimes he (or she) feels like jumping in the well to end her life.
Rights and permissions
About this article
Cite this article
Tsai, IC., Kao, YC. & Lien, YJ. Serial indirect effects of psychosocial causal beliefs and stigma on help-seeking preferences for depression. Curr Psychol 42, 13637–13647 (2023). https://doi.org/10.1007/s12144-021-02683-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-021-02683-7