Abstract
It was aimed to conduct the validity and reliability study of the Resilience Scale for Nurses and to adapt it into Turkish society. Two hundred thirty seven nurses working in a university hospital constituted the sample of this methodological study. The data of the study were collected using the Resilience Scale for Nurses and the personal information form. Language and content validity, construct validity and reliability value determination tests were conducted respectively. In the study, the scale’s content validity index was found to be 97.6%. The internal consistency reliability of the scale was found to be α = 0.86. According to the exploratory factor analysis, the total variance of the four-factor scale is 62.6%. The correlation values of total score of the items were between 0.35–0.62, and after the confirmatory factor analysis, the factor load of the items was between 0.469 and 0.792. It was found that the scale was a valid and reliable measurement tool that is applicable for Turkish society.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Psychological resilience is the ability to overcome a challenging or difficult situation (Ross, Holliman, & Dixon, 2003). Breda (2018) defined resilience as getting positive and even unexpected achievements under difficult conditions and the ability to adjust extraordinary conditions and situations. In general, not changes in life, but the number of events perceived as bad by the individual affects the individual’s level of resilience (Garcia-Dia, DiNapoli, Garcia-Ona, Jakubowski, & O’Flaherty, 2013). Resilience is consisting of only four basic temporal elements that is broadly applicable across individuals, families, and communities. These elements are (a) baseline or preadversity adjustment from which responses to adversity and ultimately resilient outcomes are referenced; (b) the actual aversive circumstances themselves; (c) postadversity resilient outcomes, referenced to both the aversive circumstances and baseline adjustment; and (d) predictors of resilient outcomes measured prior to, during, and after the aversive circumstances (Bonanno, Romero, & Klein, 2015).
The stress and challenges faced by the individual in her/his life sometimes have strengthening effect rather than hurtful effect. There is a shifting balance between life events, which may heighten a person’s vulnerability, and protective factors, which enhances resilience (Windle, 2011). In order to develop resilience, the individual should first face some risk factors such as the occurrence of a problem or worsening of an existing problem. From this aspect, resilience is a very important concept for nurses who face many risk factors in the work environment and should serve patients who are in need and difficult situation (McCann et al., 2013; Hart, Brannan, & De Chesnay, 2014).
Psychological resilience includes nurses’ ability to effectively and positively overcome challenges they face in clinical settings, to have professional competence and to help patients maintaining their optimum physical state (Park & Park, 2016). When the factors affecting the resilience of nurses were examined, it appeared that there were many factors such as work environment-related problems, communication problems with colleague or team members, problems related to patients/their relatives, nurses’ lack of positive objectives and expectations for the future (Çam & Büyükbayram, 2017). On the other hand, there were protective factors affecting the resilience. When the literature was reviewed, it appeared that there were protective factors such as secure attachment (Basım & Çetin, 2011), self-esteem (Öz & Bahadır Yılmaz, 2009; McDonald, Jackson, Wilkes, & Vickers, 2012), positive feelings (McDonald et al., 2012), hope (McCann et al., 2013; Hart, Brannan, & De Chesnay, 2014), humor (Metzl & Morrell, 2008), cognitive flexibility (McAllister, 2013), coping skills (Gillespie, Chaboyer, & Wallis, 2009), ability to express and manage feelings. It was also reported that characteristics such as taking positive and resilient persons as model, extraversion, conscientiousness, self-esteem were directly related to resilience (Tarantino, Earley, Audia, D’Adamo, & Berman, 2013).
It is particularly important to improve the resilience of nurses since this would positively affect both patients and nurses (Williams et al., 2016). In studies evaluating psychological resilience in nurses, it is stated that it is important to improve the individual resilience of nurses in order to increase the quality of care. Besides, it was found that resilience provided protection against work-related stress and also played an important role in the protection of mental and physical health of nurses (McCann et al., 2013; McDonald, Jackson, Wilkes, & Vickers, 2013; Hart, Brannan, & De Chesnay, 2014).
Positive attitudes towards the profession, future and life of nurses with high resilience positively affect their professional and life outcomes, which positively affects the care services provided by nurses to individuals, families and society despite many individual, professional and health system-related problems (Çam & Büyükbayram, 2017). In this context, it is important to determine the level of resilience of nurses for the improvement of the quality of care provided by nurses.
Studies have examined resilience as a combination of personal, familial and cultural factors and a function of protective factors consisting of personal and social resources (Johnson, Glassman, Fiks, & Rosen, 1990; Losel & Briesenel, 1990). The basis of resilience is also considered as dispositional qualities, emotional family ties, calmness, self-confidence, existential loneliness, persistence, and meaningfulness (Werner & Smith, 1982). While psychosocial behaviors have been studied, little progress has been made in developing resilience measures (Polk, 1997). As a result of the literature review, it was found that there was no measurement tool to evaluate the resilience of nurses in our country. It was believed that this study would contribute to the literature in terms of planning interventions to evaluate and improve the resilience of nurses. In addition, this measurement tool will be important for evaluating the psychological status of nurses, especially in the pandemic process, which marked the year 2020. As always, the nurses have been at the forefront as a real warrior in the pandemic process, and have put all their strengths for patients, putting their own families in the background. Heavy working conditions, working away from their families, inadequate financial support may have negatively affected the psychological resilience of nurses. This study aimed to evaluate the psychometric properties of the Resilience Scale for Nurses developed by Park, Choi and Kim (2019).
Methods
Design
This is a methodological study.
Sample/Participants
In the literature, there were different opinions about the number of samples in methodological studies. Sample size is an important factor for the estimation method used in confirmatory factor analysis to give correct results while adapting a scale (Çapık, 2014). According to Kline (2015), sample size should be 10 times higher than the number of items and should not be less than 200. Andrew, Pedersen and McEvoy (2011) stated that it was important for sample size to be 20 for each item and to include at least 10 subjects. In line with this information, the study sample of 237 nurses was of sufficient size (sample size in additional analyses made for the content validity of the scale was not included in this group).
The characteristics of the nurses are presented in Table 1. All nurses participating in the study were female and the average age of them was 32.53 ± 5.78. Approximately 83 % of them were undergraduate students and had been working as nurse for about 10 years (9.97 ± 6.20). In terms of the position and department where they were working, more than half of them (55.7%) were working in internal department and about 80 % of them (79.7%) were working as clinic nurse. More than half (57.0%) of them had voluntarily chosen the nursing profession.
Data Collection and Tools
This study was conducted with the nurses working in a university hospital between July and December 2019. Necessary explanations were made to the nurses and the data collection tool was distributed and taken back a week later by researchers. Due to the workload of the nurses, this period was given to fill the data collection tool effectively. It took 10–15 min for each participant to fill in the data collection tool. The personal information form and the Resilience Scale for Nurses were used to collect the data.
Personal Information Form
This form included questions about personal information about the nurses such as age, educational status, marital status, department where they work, their position in that department and their willingness to choose the profession.
Resilience Scale for Nurses
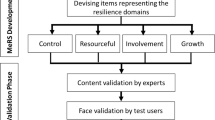
The theoretical framework of the scale was initially based on Rogers’ theory and four structures were created within the scope of Polk’s model (Polk, 1997). After the scale was developed, it was compared with similar studies (Kim & Park., 2016; Park & Park, 2016) by Park, Choi and Kim. It was a 5-point Likert-type scale developed by Park, Choi and Kim (2019) in order to measure the resilience of nurses. The scale’s original form consists of 19 items and is scored as “Strongly disagree=1, Disagree=2, Neither agree or disagree=3, Agree=4, Strongly agree=5”. The original scale’s Cronbach’s alpha value was found to be 0.94 (Park, Choi & Kim, 2019). It consists of four sub-dimension (Philosophical pattern, Relational pattern, Situational pattern, Dispositional pattern).
Philosophical pattern (1, 2, 3, 4, 5, 6): This pattern is manifested by personal beliefs. The belief that self-knowledge is valuable and reflection about oneself and events contribute to this pattern.
Relational pattern (7, 8, 9, 10): The relational pattern refers to the characteristics of roles and relationships that influence resilience.
Situational pattern (11, 12, 13): This pattern discloses resilience as a characteristic approach to situations or stressors and is manifested as cognitive appraisal skills, problem-solving ability, and attributes that indicate a capacity for action in facing a situation.
Dispositional pattern (14, 15, 16, 17, 18, 19): The dispositional pattern refers to the pattern of physical and ego-related psychosocial attributes that contribute to the manifestation of resilience.
In the original study, the Cronbach’s alpha values of the sub-dimensions were found as follows; Philosophical pattern = 0.92, Relational pattern = 0.80, Situational pattern = 0.84, Dispositional pattern = 0.84. The total score of the scale varies from 19 to 95, and the higher total score means that nurses have higher resilience.
Data Analysis
The data were evaluated using SPSS 23.00 and AMOS 24.0 programs. Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA) techniques were used for scale construct validity. Direct Oblimin method was used in exploratory factor analysis. Bartlett Sphericity test and Keiser-Mayer-Olkin tests were used to determine the adequacy of the scale content and sample size. The factor structure and factor loads of the scale were examined by confirmatory factor analysis (0.469–0.792). Furthermore, Davis technique was used to assess expert opinion in the content validity analysis. In the Davis technique, expert opinions are analyzed as a) appropriate, b) needs some correction, c) needs quite correction, d) not suitable. The content validity index (CVI) is obtained by dividing the sum of A and B in all expert forms by the total number of experts. If CVI is greater than 80%, the question is sufficient in terms of content validity (Davis, 1992).
Ethical Principles
Written permission was obtained from the corresponding author, Sunghee Park via e-mail, for the validity and reliability study of the Resilience Scale for Nurses. Sunghee Park emailed the necessary data about the scale and stages. The necessary permissions were taken from the XXX University Clinical Researches Ethics Committee (70904504–331) to conduct this study. Before starting the study, the nurses were informed about the aim of the study, the time of the completion of the questionnaire and voluntary participation, and after their questions (if any) were answered, the written informed contents were received from those who agreed to participate in study.
Results
Results of Linguistic and Content Validity Analysis
The linguistic validity of the scale was tested using translation-back translation method and translated from English to Turkish by three English linguists. After these translations were edited, the form was translated back into English by three English linguists who were capable of understanding and speaking both languages (Turkish-English) independent of the first group of translators. After the English translated version of the scale was compared with the original English version, the Turkish version was reviewed. After necessary corrections were made, the scale was submitted to expert opinion for the content validity.
The Davis technique was applied to the scale which was sent to nine experts for the evaluation of content validity, and the scale’s CVI was found to be 97.6% and there was no item excluded from the content. It was determined that the scale was an appropriate tool for the measurement of the resilience of nurses. In the content validity analysis stage, the scale was also applied to 20 clinic nurses to control whether the items were expressed in an accurate and understandable manner, and the scale was finalized in accordance with the opinions of the nurses.
Results of the Construct Validity Study
Kaiser-Meyer-Olkin (KMO) and Bartlett test results of the scale were found to be 0.912 and χ2 = 2849.893 (p < .001). Exploratory Factor Analysis (EFA) was used to examine the factor structure of the Resilience Scale for Nurses. Since Items 3, 6, 8 and 11 of the Resilience Scale for Nurses, the original form of which consisted of 19 items, showed low correlation as a result of the EFA, these four items were excluded from the scale and thus 15-item scale with four factors was obtained. The factor loads varied between 0.469 and 0.792. The four-factor structure accounted for 62.606% of the total variance. In accordance with the scale’s original form and the contents of items, Factor 1 was described as “Philosophical pattern”, Factor 2 was described as “Relational pattern”, Factor 3 was described as “Situational pattern” and Factor 4 was described as “Dispositional pattern” (Table 2).
Results of the Confirmatory Factor Analysis
Confirmatory Factor Analysis (CFA) was performed to determine whether the four-factor structure of the scale would be confirmed or not. To demonstrate the adequacy of the model tested in CFA, several adaptation indices were used. Chi-square goodness of fit test, GFI, RMSEA, CFI and AGFI goodness of fit indices were examined for CFA performed in this study. Convergent validity and discriminatory validity of the item were verified to evaluate the construct validity of the scale. Convergent validity was evaluated with standard factor load, critical rate (C.R.) value, Average Variance Extracted (AVE) and Construct Reliability (CR). Discriminant validity was evaluated by the difference between the square of the correlation coefficient and the AVE value.
According to the results of Confirmatory Factor Analysis, it was found that χ2 = 259.60; df = 78 and p = 0.000. χ2/df was equal to 3.32 and lower than the acceptable reference value of ≤5 (İlhan & Çetin, 2014). Furthermore, the values of RMSEA = 0.079, CFI = 0.900, GFI = 0.860, AGFI = 0.900 were also found. According to these values, they were at reasonable fitness level. All the results showed that the model-data fitness was acceptable. In other words, it can be said that the four-model model was appropriate and the construct validity of the scale was met (Table 3). By examining the Path diagram according to the confirmatory factor analysis, it was found that the model was fit and that the path graph for the scale items was within the acceptable limits (Figure 1).
Internal Reliability Results
The reliability of the scale was evaluated based on the item-total correlation and the correlation and alpha values in cases where items were excluded. According to the Cronbach’s alpha values of the 15-item final version of the Resilience Scale for Nurses, the total value of the scale was found to be 0.862 including 0.855 for Philosophical pattern, 0.697 for Relational pattern, 0.862 for Situational pattern and 0.841 for Dispositional pattern (Table 4).
Discussion
The aim of this study was to adapt the Resilience Scale for Nurses into Turkish and to test its validity-reliability.
Validity of the Resilience Scale
Validity refers to the degree to which a measurement tool accurately measures the characteristics that are intended to be measured without other characteristics (Karakoç & Dönmez, 2014). It shows whether the researcher really measures the variable which he/she intends to measure, and it is a compulsory process for a measurement tool (Tezbaşaran, 2008; Erefe, 2012; Karasar, 2016; Sümbüloğlu & Sümbüloğlu, 2017).
In terms of linguistic validity, it firstly refers to the determination of the fitness of intended expressions for the purpose and the fact that the expressions are appropriate for the educational, cultural and knowledge level of the target group. According to this approach, two independent translators should translate the scale to the target language and another two independent translators should translate the scale to the original language. Then, the draft scale should be compared by the researcher with the original scale and a pilot study should be performed to test the scale (Karakoç & Dönmez, 2014). In this study, a similar process was applied in the linguistic validity stage of the “Resilience Scale for Nurses” and after making necessary corrections, the scale was submitted to expert opinion for the evaluation of content validity.
Content validity refers to the degree to which the overall scale and its each item serve the purpose. The opinions of the subject matter experts are obtained for the content validity as well as many techniques are used for the evaluations done by the experts on content validity (Karakoç & Dönmez, 2014).
Adequate sample size is required to perform the construct validity analyses of the scale. Since the KMO value should be >0.90 (Yu, 2012; Park, Choi, & Kim, 2019), the sample size was considered appropriate to perform the factor analysis. Construct validity is used to determine which concepts or characteristics the scale measures. The total variance of the four-factor structure obtained in the EFA is similar to the original version of the scale (Park, Choi, & Kim, 2019). However, the factor load values of 15 items as a result of the EFA of the scale are greater than 0.32 (Tabacnick & Fidell, 2014). Four items with low factor loading were excluded. The low factor load of these items may be due to the insufficient sample size.
Confirmatory Factor Analysis (CFA) was performed to measure the construct validity of the “Resilience Scale for Nurses”. CFA is a type of structural equation modeling (SEM) which is called as a research method by itself (Şimşek, 2007). CFA which is performed to examine the factor structure of a scale in nursing researches (Çapık, 2014) is used to reveal the underlying structure of a large number of variables. The aim of the CFA is to facilitate understanding and interpretation of the relationships between the many variables which are considered to be related and to theoretically find what the scale questions measure (Şencan, 2005; Çapık, 2014). As a result of the CFA analysis of the Resilience Scale including four sub-dimensions and 15 items, the “t” values of the items were found significant (p < 0.05). The fact that “t” values of all items in the model are significant is a necessary condition for the model to be acceptable (Çelik & Yılmaz, 2014). In the CFA of the scale, it was found that the fit indexes were appropriate and similar to the original version of the scale (Park, Choi, & Kim, 2019). In this context, it was determined that the results obtained from the data collected from the individuals were fit to the theoretical construct.
In addition to the fit values, the Construct Reliability (CR) value is calculated to test the reliability of the scale’s structure. It is also necessary to determine the Average Variance Extracted (AVE) values, which is a summary of the extent of convergence between certain items representing a latent structure. CR and AVE values are also used in determining the convergent validity of a scale. Convergent validity is the assessment of the degree of relationship of two similar concepts measured. Hair, Black, Babin and Anderson (2010) state that values between .60 and .70 are acceptable for values of CR and values of .70 and above are accepted as good. It is recommended that the AVE be .50 and above. It is seen that the CR values showing the structural reliability of the scale are good for all four sub-dimensions. The AVE values of the scale are seen to be at a good level. Compared with the original scale, it is seen that AVE and CR values are in appropriate ranges (Park, Choi, & Kim, 2019).
In the structural equation modeling, path diagrams are obtained as a result of analyses. After appropriate matrix is created, Path diagram is drawn, which shows model variables, t values, factor loads, unexplained variance and some goodness of fit values (Gatignon, 2011; Çapık, 2014). As a result of the Path analysis performed in the study, the path graph for the scale items was found to be within the appropriate range. Consequently, it was determined that the four-sub-dimension structure of the 15-item “Resilience Scale for Nurses” was appropriate for the model and that the scale met the construct validity requirements.
Reliability of the Resilience Scale
Reliability of a measurement tool is the degree of consistency with which the tool measures the intended variable and the degree to which the measurement results are free from errors (Tavşancıl, 2010; Taşkın & Akat, 2010). For internal consistency reliability, the scale items should have a certain conceptual construct and the items should measure the same construct interrelatedly (Şencan, 2005; Gürbüz & Şahin, 2014). Cronbach Alpha value is a measure of internal consistency of items in the scale (Alpar, 2010). Cronbach’s Alpha, essentially a reliability index value, provides information about the inter-item correlation in the scale and about the degree to which it represents the hidden variable in the background (Şencan, 2005). As Cronbach Alpha coefficient increases, the reliability of the scale increases, too (Şencan, 2005; Tezbaşaran, 2008). Özdamar (2013) stated that the reliability of a scale is high if its Cronbach Alpha coefficient was between 0.80 ≤ a < 1.00. It was determined the Cronbach Alpha reliability coefficient was high for overall and sub-dimensions of the “Resilience Scale for Nurses” and it was found a = 0.86 for the overall reliability of the scale. Although this finding is lower than Cronbach’s alpha value of the original scale (Park, Choi & Kim, 2019), it is good level. This difference between the two studies may have resulted from cultural differences, the main impressive factor in scale adaptation studies. Consequently, it was determined that there was inter-term consistency and represented the variable in the background which was intended to be measured.
Item-total score correlation coefficient was used to determine the ability of each item to measure what is intended to be measured using the scale (Özdamar, 2013). Item-total correlation coefficient should not be negative and higher than +0.25 (Alpar, 2010). If there is a positive and “adequately high” correlation in the relationship between the score of an item and the overall score of the scale, then this item is considered as distinctive or it is assumed that these items represent similar behaviors and the item is included in the scale (Büyüköztürk, 2019). It was determined that item-total score correlation of the 15-item scale was between 0.35 and 0.62 (n: 237) and there was no item which should be excluded from the scale. Although this finding is lower than the original values of the scale (0.53–0.76) (Park, Choi, & Kim, 2019), it is compatible because it is higher than the specified +25 limit value. Consequently, it was found that the scale items were distinctive in terms of attributes which they measured and that the reliability of 15 items constituted the scale was high and they were intended for the same purpose.
Limitations
Intensive work of nurses may have limited participation in the research. In addition, the other limitations of the study are that the study was conducted in a single center and during daylight hours.
Conclusion
When the validity and reliability results of the “Resilience Scale for Nurses” developed by Park, Choi and Kim (2019) to determine resilience of nurses were examined, it was determined that the linguistic validity analysis of the 5-point Likert-type scale was performed, and that the CVI indicating content validity, the item-total correlation indicating reliability and the Cronbach Alpha value were high. According to the CFA results, it was found that “t” values of 15 items were significant and the four-factor structure of the scale was acceptable.
As a result of the analyses, the total Cronbach Alpha value of the scale (Philosophical pattern: 1, 2, 4, 5, Relational pattern: 7, 9, 10, Situational pattern: 12, 13, Dispositional pattern: 14, 15, 16, 17, 18, 19) was found to be a = 0.86 and that the scale was a valid and reliable scale.
The results of the Resilience Scale for Nurses included the nurses who were working in a university hospital where the validity and reliability study was conducted. Thus, it is particularly important to conduct studies on different samples for the validity and reliability of the scale. The studies in which this scale will be used will make significant contributions to its ability to measure.
References
Alpar, R. (2010). Spor, sağlık ve eğitim bilimlerinden örneklerle uygulamalı istatistik ve geçerlilik güvenirlilik. Ankara: Detay Yayıncılık.
Andrew, D. P. S., Pedersen, P. M., & McEvoy, C. D. (2011). Research methods in sport management. Champaign: Human Kinetics.
Basım, H. N., & Çetin, F. (2011). Yetişkinler için psikolojik dayanıklılık ölçeğinin güvenilirlik ve geçerlilik çalışması. Turk Psikiyatri Dergisi, 22, 104–114.
Bonanno, G. A., Romero, S. A., & Klein, S. I. (2015). The temporal elements of psychological resilience: An integrative framework for the study of individuals, families, and communities. Psychological Inquiry, 26(2), 139–169. https://doi.org/10.1080/1047840X.2015.992677.
van Breda, A. D. (2018). A critical review of resilience theory and its relevance for social work. Social Work/Maatskaplike Werk, 54(1), 1–18. https://doi.org/10.15270/54-1-611.
Büyüköztürk, Ş. (2019). Sosyal bilimler için veri analizi el kitabı. 25. Baskı, Ankara: Pegem Yayıncılık.
Çam, O., & Büyükbayram, A. (2017). Hemşirelerde psikolojik dayanıklılık ve etkileyen faktörler. Psikiyatri Hemşireliği Dergisi, 8(2), 118–126.
Çapık, C. (2014). Geçerlik-güvenirlik çalışmalarında doğrulayıcı faktör analizinin kullanımı. Anadolu Sağlık ve Hemşirelik Dergisi, 17(3), 196–205.
Çelik, H. E., & Yılmaz, V. (2014). LISREL 9.1 ile yapısal eşitlik modellemesi: Temel kavramlar-uygulamalar-programlar. 3. Baskı, Ankara: Anı Yayıncılık.
Davis, L. L. (1992). Instrument review: Getting the most from a panel of experts. Applied Nursing Research, 5, 194–197. https://doi.org/10.1016/S0897-1897(05)80008-4.
Erefe, İ. (2012). Hemşirelikte araştırma ilke süreç ve yöntemleri, 4. Hemar-Ge Yayıncılık: Baskı. İstanbul.
Garcia-Dia, M. J., DiNapoli, J. M., Garcia-Ona, L., Jakubowski, R., & O’Flaherty, D. (2013). Concept analysis: Resilience. Archives of Psychiatric Nursing, 27, 264–270. https://doi.org/10.1016/j.apnu.2013.07.003.
Gatignon, H. (2011). Statistical analysis of management data. London: Springer.
Gillespie, B. M., Chaboyer, W., & Wallis, M. (2009). The influence of personal characteristics on the resilience of operating room nurses: A predictor study. International Journal of Nursing Studies, 46, 968–976. https://doi.org/10.1016/j.ijnurstu.2007.08.006.
Gürbüz, S., & Şahin, F. (2014). Sosyal bilimlerde araştırma yöntemleri. Ankara: Seçkin Yayıncılık.
Hair Jr., J. F., Black, W. C., Babin, B. J., & Anderson, R. E. (2010). Multivariate data analysis (Seventh ed.). New Jersey: Pearson Prentice Hall.
Hart, P. L., Brannan, J. D., & De Chesnay, M. (2014). Resilience in nurses: An integrative review. Journal of Nursing Management, 22, 720–734. https://doi.org/10.1111/j.1365-2834.2012.01485.x.
İlhan, M., & Çetin, B. (2014). LISREL ve AMOS Programları kullanılarak gerçekleştirilen Yapısal Eşitlik Modeli (YEM) analizlerine ilişkin sonuçların karşılaştırılması. Eğitimde ve Psikolojide Ölçme ve Değerlendirme Dergisi, 5(2), 26–42.
Johnson, H., Glassman, M., Fiks, K., & Rosen, T. (1990). Resilient children: Individual differences in development outcome of children born to drug abusers. The Journal of Genetic Psychology, 151, 523–539.
Losel, F., & Bliesener, T. (1990). Resilience in adolescence: A study on the generalizability of protective factors. In K. Hurrelmann & F. Losel (Eds.), Health hazards in adolescence (pp. 299–320). New York, NY: Walter de Gruyter.
Werner, E., & Smith, R. (1982). Vulnerable but invincible: A longitudinal study of resilient youth and children. New York, NY: McGraw-Hill.
Karakoç, F. Y., & Dönmez, D. (2014). Ölçek geliştirme çalışmalarında temel ilkeler. Tıp Eğitimi Dünyası, 40, 39–49.
Karasar, N. (2016). Bilimsel araştırma yöntemi. Ankara: Nobel Akademik Yayıncılık.
Kim, S., & Park, S. (2016). Verification of validity and reliability of resilience scale for nurses. Journal of the Korean Data Analysis Society, 18(4B), 2257–2269.
Kline, R. B. (2015). Principles and practice of structural equation modeling. New York: Guilford Press.
McAllister, M. (2013). Resilience: A personal attribute, social process and key professional resource for the enhancement of the nursing role. Professioni Infermiesristiche, 66, 55–62. https://doi.org/10.7429/pi.2013.661055.
Mccann, C. M., Beddoe, E., Mccormick, K., Huggard, P., Kedge, S., Adamson, C., & Huggard, J. (2013). Resilience in the health professions: A review of recent literature. International Journal of Wellbeing, 3, 60–81.
McDonald, G., Jackson, D., Wilkes, L., & Vickers, M. H. (2013). Personal resilience in nurses and midwives: Effects of a work-based educational intervention. Contemporary Nurse, 45(1), 134–143. https://doi.org/10.5172/conu.2013.45.1.134.
McDonald, G., Jackson, D., Wilkes, L., & Vickers, M. H. (2012). A work-based educational intervention to support the development of personal resilience in nurses and midwives. Nurse Education Today, 32, 378–384. https://doi.org/10.1016/j.nedt.2011.04.012.
Metzl, E. S., & Morrell, M. A. (2008). The role of creativity in models of resilience: Theoretical exploration and practical applications. Journal of Creativity in Mental Health, 3, 303–318. https://doi.org/10.1080/15401380802385228.
Öz, F., & Bahadır Yılmaz, E. (2009). Ruh sağlığının korunmasında önemli bir kavram: Psikolojik sağlamlık. Sağlık Bilimleri Fakültesi Hemşirelik Dergisi, 82–89.
Özdamar, K. (2013). Paket programlar ile istatistiksel veri analizi. Ankara: Nisan Kitabevi, 9.Baskı.
Park, M. M., & Park, J. (2016). Development of resilience scale for nurses. Journal of Korean Academy of Fundamentals of Nursing, 23(1), 32–41. https://doi.org/10.7739/jkafn.2016.23.1.32.
Park, S., Choi, M., & Kim, S. (2019). Validation of the resilience scale for nurses. Archives of Psychiatric Nursing, Article in Press., 33, 434–439. https://doi.org/10.1016/j.apnu.2018.12.004.
Polk, L. V. (1997). Toward a middle-range theory of resilience. Advances in Nursing Science, 19(3), 1–13. https://doi.org/10.1097/00012272-199703000-00002.
Ross, L., Holliman, D., & Dixon, D. R. (2003). Resiliency in family caregivers. Journal of Gerontological Social Work, 40(3), 81–96. https://doi.org/10.1300/J083v40n03_07.
Şencan, H. (2005). Sosyal ve davranışsal ölçümlerde güvenirlik ve geçerlik. Ankara: Seçkin Yayıncılık.
Şimşek, Ö. F. (2007). Yapısal eşitlik modellemesine giriş, temel ilkeler ve LİSREL uygulamaları. Ankara: Ekinoks.
Sümbüloğlu, V., & Sümbüloğlu, K. (2017). Biyoistatistik. 17. Baskı, Ankara: Hatipoğlu Yayınevi.
Tabachnick, B. G., & Fidell, L. S. (2014). Using multivariate statistics (6th ed.). USA: Pearson Education Limited.
Tarantino, B., Earley, M., Audia, D., D’Adamo, C., & Berman, B. (2013). Qualitative and quantitative evaluation of a pilot integrative coping and resiliency program for healthcare professionals. Explore (New York, N.Y.), 9, 44–47. https://doi.org/10.1016/j.explore.2012.10.002.
Taşkın, Ç., & Akat, Ö. (2010). Araştırma Yöntemlerinde Yapısal Eşitlik Modelleme. Bursa: Ekin Yayınevi.
Tavşancıl, E. (2010). Tutumların Ölçülmesi ve SPSS ile Veri Analizi (4. Basım). Ankara: Nobel Yayın Dağıtım.
Tezbaşaran, A. (2008). Likert Tipi Ölçek Geliştirme Kılavuzu. 3. Baskı, Ankara: Türk Psikologlar Derneği Yayınları.
Williams, J., Hadjistavropoulos, T., Ghandehari, O. O., Malloy, D. C., Hunter, P. V., & Martin, R. R. (2016). Resilience and organisational empowerment among long-term carenurses: Effects on patient care and absenteeism. Journal of Nursing Management, 24(3), 300–308. https://doi.org/10.1111/jonm.12311.
Windle, G. (2011). What is resilience? A review and concept analysis. Reviews in Clinical Gerontology, 21, 152–169. https://doi.org/10.1017/S0959259810000420.
Yu, J. (2012). Yu jong pil professor's structural equation modeling concept and understanding. Seoul: Hannarae Publishing Co..
Acknowledgments
We would like to thank all the participants shared their information with us.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Derya Adıbelli, Nurcan Kırca, Kerime Bademli, Concept and design of study or acquisition of data or analysis and interpretation of data.
Derya Adıbelli, Nurcan Kırca, Kerime Bademli, Drafting the article or revising it critically for important intellectual content; and.
Derya Adıbelli, Nurcan Kırca, Kerime Bademli, Final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adıbelli, D., Kırca, N. & Bademli, K. The psychometric properties of Turkish version of the resilience scale for nurses. Curr Psychol 40, 4709–4717 (2021). https://doi.org/10.1007/s12144-021-02029-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-021-02029-3