Abstract
Evaluating interventions to improve the mental health among university students in China is a critical priority. Depression, compared to other psychological problems, is one of the most commonly occurring disorders and is associated with school-related impairment and risk of suicide. The aim of the current study is to obtain estimates for design of future definitive trial and obtain preliminary evidence of the effect of a computerized positive mental imagery training intervention, which consisted of 8 sessions delivered across 4 weeks. Participants use ambiguous cues to generate positive scenarios repeatedly from a first-person perspective. In the current study, the BDI-II, PANAS, and RRS were measured at baseline, post-training, and 4-week follow-up. Forty-one participants were non-randomly assigned to either the intervention training group (n = 22) or wait-list (n = 19). Results showed an attrition rate for interventional group was 20%. In addition, group × time interaction for depressive symptoms, positive and negative affect, and rumination, with the intervention group demonstrated better outcomes than controls across time. The largest treatment gains and clinically significant improvements were observed at follow-up. Positive mental imagery training was successfully tested with an acceptable attrition rate. Preliminary results showed that it improved Chinese university students’ depressive symptoms, mood, and maladaptive thinking style. Future larger scale intervention trials are needed to further evaluate the efficacy of this intervention among Chinese university students.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The mental health of Chinese university students is of critical importance. A recent study of 5972 undergraduates from 6 universities in mainland China found that 19.9% met criteria for mild to high depression. More alarmingly, 7%–8% reported suicidal behavior (i.e., presence of suicidal ideation or attempt) in the past year (Tang et al. 2018) One study conducted by Chen et al. (2013) indicated that 11.7% of the participants had a BDI score ≥ 14, and 4% met criteria for Major Depression Disorder by Structured Clinical interview (SCID). Shi et al. (2016) found the prevalence of depression in Chinese medical university students was high and 66.8% met the criteria for depression based on the Center for Epidemiologic Studies Depression Scale (CES-D). Results of meta-analyses suggested the prevalence of depression among university students in mainland China ranges from 23.8% to 30.39% (Jiang et al. 2015; Lei et al. 2016). These studies highlighted the critical and urgent need to develop interventions to address depression among university students.
Mental health services available at universities are not sufficient to meet students’ needs. According to a nationwide survey of 24 countries, structural barriers (e.g., cost, availability, inconvenience) were most common among young adults with perceived need for treatment (Andrade et al. 2014). Psychological or mental health services freely provided by university psychological counselling centers would reduce these barriers. However, in China, psychological professionals and services at tertiary educational institutions are not sufficient and students expect more psychological counseling services to be provided by universities (Liu and Shi 2010). Another common barrier to psychological treatment in university settings is the long waiting list, leading to delays in needed services. The Chinese government aimed to improve this situation, which led to the creation of a mental illness prevention curriculum (e.g., as a regular course throughout a semester), while expanded psychological counselling services was not considered a top priority (Yang et al. 2015). More accessible psychological intervention and services are needed for Chinese university students.
Given limited human resources, low-intensity interventions may play a vital role in lessening barriers to treatment for students and strengthen mental health services at universities. Low-intensity interventions are brief, evidence-based, and they may rely on self-help. Previous research showed that low-intensity interventions could enhance individuals’ mental health (Bowler et al. 2012; Davies et al. 2014), and found the effect in improving symptoms of depression in university students (Hall et al. 2018; Saleh et al. 2018).
In addition to specialist models of care, interventions need to be developed, adapted and trialed that can be scalable to wider group of people who may not seek the help of a therapist. Positive mental imagery training (PMIT) is an intervention first developed by Blackwell and Holmes (2010), and adopted from an experimental research paradigm studying the effect of mental imagery on emotion (Holmes and Mathews 2005). The intervention is based on the common characteristic of negative bias among individuals with depression, and utilizes cognitive bias modification, by which selective information processing is directly retrained (MacLeod and Mathews 2012), in order to reduce depressive symptoms. The intervention is delivered by computer and normally has guidance from a researcher at the beginning and monitor throughout the training duration (Blackwell et al. 2015).
PMIT is a novel intervention which is specific to depression. People with depression tend to ignore or discount positive information (Levens and Gotlib 2009), and are prone to attend to negative stimulus (Bar-Haim et al. 2007). Modifying this bias, through being exposed to positive stimuli or persistently making positive attributions to ambiguous scenarios, may alter cognitions. People with depression were also characterized by verbal and ruminative processing and a third-person perspective in mental imagery (Koster et al. 2011; Williams and Moulds 2007). Therefore, non-verbal processing and the utilization of the first-person perspective in mental imagery modifies maladaptive thinking, and in turn, depressive symptoms. According to Blackwell and Holmes (2010), during PMIT, participants repeatedly generated positive mental imagery from a first-person perspective from a variety of ambiguous daily scenarios. This intervention was tested in clinical trials in different populations, such as out-patients with depression (Torkan et al. 2014) and community populations with depression (Blackwell et al. 2015; Pictet et al. 2016; Renner et al. 2017), but it has not been evaluated in a Chinese population.
Burnett Heyes et al. (2017)demonstrated that engaging in positive mental imagery promoted positive mood. A different mood program incorporating mental imagery found that imaging from a field perspective (i.e., as if they were experiencing and seeing scenarios through their own eyes) were more effective in increasing positive mood than from an observer perspective (i.e., seeing themselves from the outside) (Grol et al. 2017). Affect is closely associated with psychiatric conditions, overall wellbeing, and mental health (Dixon-Gordon et al. 2015; Fredrickson 2001; Watson et al. 1988). Existing research recognizes the reciprocal relationship between rumination and negative affect (Brans et al. 2013; Schafer et al. 2017), and Torkan et al. (2014) has confirmed the effectiveness of PMIT on rumination, which is defined as the repetitive and passive attentiveness on one’s own symptoms of distress (Nolen-Hoeksema et al. 1997), often observed in individuals with depression, and considered as the cognitive process related to the onset and maintenance of depression (Watkins 2008). Thus, interventions that improve mood and rumination are likely be effective to enhance individuals’ mental health, particularly those with mood-related disorders, such as depression.
Accumulating evidence demonstrated that positive mental imagery training reduced greater depressive symptoms (Lang et al. 2012; Pictet et al. 2016; Torkan et al. 2014), anhedonia (Blackwell et al. 2015), as a standalone intervention compared with a control condition (Blackwell et al. 2015; Lang et al. 2012). Adjunct to iCBT, completers in the positive group demonstrated greater decreases in depressive symptoms after receiving positive mental imagery training and completion of the whole program, compared with the control group (Williams et al. 2015). Various studies evaluated the effect of PMIT in different countries, however, cognitive bias modification, the key mechanism of PMIT, has yet to be evaluated in China (Huang and Wang 2015).
The aim of the current pilot study is (1) obtain estimates to inform sample size calculation and (2) obtain preliminary evidence for further a definitive trial study.
Methods
Design
The study obtained approval from the university Ethics Review Board. A pilot, non-blind, non-randomized controlled trial with two groups was conducted. Intervention condition (training group versus wait-list control) is between-group factor and time (pre-intervention, post-intervention, and 4-week after the end of intervention) is within-group factor. Time interval between pre and post-intervention assessment was 4 weeks.
Participants
Participants were recruited via advertisement on social networking services (e.g., university forum, WeChat-a widely popular Chinese social media platform), and they decided whether to join the training that semester (training group) or next semester (wait list). Two advertisements for each group were prepared. They described the training as part of the research project and its purpose, which is to test whether the computerized positive imagery training can improve mood symptoms. It also included some criteria of participants’ characteristics (e.g., students enrolled in university, fluent in Chinese), who could have benefit from it (e.g., people who feel sad, upset, loss of interest), the study procedure, details of the training (e.g., time for each session, frequency, training venue), compensation, and a link and scannable code for application for each group. People who completed the application form of the training were considered intervention-seeking. In consideration of students’ schedule and service needs, we decided not to randomize participant into groups and allowed them to decide when to participate to increase their commitment to this study. Eligible participants were university students aged 18 or above, intervention seeking, fluent in Chinese, with no hearing impairment, or vision impairment (or corrected to normal), and whose depression severity between minimal to moderate (BDI-II scores ≤28). Participants were excluded if they were receiving psychological therapy or medication, met ICD-10 criteria for substance abuse, excessive drinking, mania, psychotic disorders, or if they were at high risk of suicide, assessed by the Chinese version of Mini-international Neuropsychiatric Interview (MINI, Version 5.0; Sheehan et al. 1998) via phone by four first-year and five second-year clinical psychology master students who had received sufficient training on administering the MINI. We did not decide a lower cut-off for depression because the help-seeking participants believed they had some symptoms, and we included them in the pilot study for their benefit and well-being as they might not receive other psychological services compared to those with severe symptoms and suicidal risk. Enrolled participants who were not excluded after the first screening would be contacted for MINI interview by phone call and text message. Participants who did not answer the phone call would receive a text message for rescheduling the MINI interview, non-responsive participants would be contacted again on the first and the second day after the first call made. Participants would be categorized as cannot contact if they failed to reply the message or answer the third call. For those who go through the MINI screening, a phone would be made to them to confirm their time availability for training. Participants who did not answer the phone call would receive a text message about training invitation with request their time availability, non-responsive participants would be contacted again on the first and the second day after the first call made. Participants would be categorized as cannot contact if they failed to reply the message or answer the third call. Ineligible participants received a thank you email, and in cases where they were ineligible due to psychiatric condition or suicidality, contact information was provided for the university psychological health center. Eligible participants were invited to a computer room to take part in the study. The research purpose and process of intervention were explained to the participants before written consent was obtained. Recruitment started from November 2017, training was completed by April 2018, and follow-up was completed by June 2018. All assessments were completed on the Chinese questionnaire platform www.wjx.com.
Intervention
Four hundred and sixteen scenarios of auditory material in English from (Blackwell et al. 2015) were translated into Chinese by 3 s-year master students. Several expressions were adapted for Chinese culture (e.g. “Christmas” changed to “Chinese New Year”). After thorough discussion by three master students, 15 scenarios which were not common in China and 56 scenarios deemed irrelevant to Chinese university students were deleted, and 71 scenarios which were common and related to Chinese university students’ daily life were added, (e.g., “You felt lost in looking for a summer internship. So, you sent out a number of resumes to various companies for different positions and have had some interviews. Finally, you are offered your most desired internship position.”). There were 416 auditory materials obtained and recorded by two students (one male and one female). A total number of 416 non-copyright colored pictures related to Chinese university students’ everyday life were provided by one undergraduate and one master students. All pictures were adjusted to photo size of 640 × 480 pixel, and relevant Chinese description was added by three master students. The original PMIT used by (Blackwell et al. 2015) consisted of 12 sessions across 4 wks. The first week included six sessions, and the remaining 3 wks included two sessions for each week. Starting with an auditory session, PMIT proceeds with alternate types of training material (auditory versus picture-word). Due to the tight schedule of university students, PMIT used in this study was adjusted to a four-week training consisting of eight sessions, and each week included one auditory session and one picture-word session. Each session was comprised of a warm-up scenario and 64 training scenarios (eight blocks per session, eight trials per block), and no scenario was used more than once. The whole intervention (including warm-up) comprised 260 scenarios for auditory sessions (equal number of male and female voice) and 260 for picture-word session, which were randomly selected. All materials of the intervention were in Chinese. The average duration for an auditory scenario was 14 s. Each session lasted about 30 min.
Training Group
Positive mental imagery training is a computerized intervention completed on Matlab 2014. During the auditory sessions, participants listened to some daily scenarios, closed their eyes to generate corresponding mental imageries as if they were experiencing and seeing it from their own eyes. Scenarios start from an ambiguous description, and end with a positive outcome (e.g. “You take charge of a project and have fallen behind on deadlines. Your friend offers you some help, and you are glad that you were supported.”). During the picture-word sessions, participants were exposed to some colored and ambiguous daily photos with positive description (Fig. 1), and then they were asked to combine the picture and word to generate the mental imagery. Participants rated the vividness of each mental imagery before moving to the next scenario, rating on a five-point scale, where 1 indicates not at all vivid and 5 indicates extremely. Each session started with a warm-up to allow participants to become familiar with the operation of the computerized intervention. A self-paced resting interval occurred before the participants moved to the next block (Fig. 2). After each session, participants were asked to respond to a 1-item question on their feeling that day as mood monitoring (−7 = very unhappy, 0 = neutral, 7 = very happy).
In the first session, participants were instructed to learn the skills of mental imagery and reminders of positive imagery training by Power Point slides on computer and that took about 5 min. Participants were provided the opportunity to ask questions about mental imagery and the training. Ensuring participants had no question, the first session of training started. All the trainings were done in a university computer room. Our guidance model included two parts: in-person assistance in computer room and on demand text message and phone support outside computer room. In-person assistance in computer room was to deal with technical problems using the program while on demand was to provide support or reschedule the training when needed during the training phase. Participants were offered 50 RMB (~9USD) following training completion and another 50 RMB at follow-up.
Wait-List
The wait-list did not receive the training during the study period and was informed via e-mail to join the training after the trial period concluded. After learning the purpose of the research, participants provided consent and started the first assessment (baseline). When they finished the baseline assessment, they were told the date of the second (post-training) and the third assessment (follow-up). Participants were offered 50 RMB and 30 RMB following the second and third assessments, to coincide with the post-training and follow-up for the training group.
Measurements
Assessment on depressive symptoms, positive and negative mood, and rumination were conducted at pre-training, post-training, and four-week follow-up.
Demographic Information
Demographics obtained included age, gender, degree type, and current level of depression.
Beck Depression Inventory-II (BDI-II)-Chinese Version
BDI-II was developed by Beck et al. (1996). The Chinese version of BDI-II was translated by Wang et al. (2011) among Chinese, which has been found positively related to Hamilton Depression Scale (HAMD) Chinese version, and whose two-factor construct was decided by EFA. The Chinese BDI-II has been widely used to measure depression severity among Chinese (Yang et al. 2012)It is a self-reported questionnaire consisting of 21 items. Each item is rated on a 4-point scale ranging from 0 to 3 based on severity. The total score ranges from 0 to 63, where 0 to 13 indicates minimal depression, 14–19 indicates mild depression, 20–28 indicates moderate depression, and 29–63 indicates severe depression. In this study, the Chinese version of BDI-II showed excellent internal consistency among Chinese university students (α = .90).
Positive Affect and Negative Affect Schedule (PANAS)-Chinese Version
PANAS is a self-reported questionnaire that consists of 2 10-item scales to measure positive affect and negative affect (Watson et al. 1988). The current study used a valid and reliable Chinese revised version of PANAS for university students (Qiu et al. 2008), consists of two nine-item scales to measure both positive (e.g., excited, proud) and negative affect (e.g., upset, ashamed). Each item was rated on a five-point scales that ranges from 1 (very little or not at all) to 5 (extremely strong) to reflect how strong the described affect that one has experience in the past 3 wks was. The revised version of both positive and negative scales showed good internal consistency among Chinese university students, α = .85 and α = .84 respectively (Qiu et al. 2008). The internal consistency of the positive and negative affect scales in this study were Cronbach’s α = .92 and α = .88, respectively.
Ruminative Response Scale (RRS)- Chinese Version
RRS measured individuals’ reaction style to depression (Nolen-Hoeksema and Morrow 1991). It consists of 22 items and 3 subscales which are symptoms rumination (e.g., think about how angry you are with yourself), brooding (e.g., think “Why do I always react this way?”), and reflective pondering (e.g., analyze recent events to try to understand why you are depressed). Items are rated on a 4-point scale (1 = almost never, 2 = sometimes, 3 = often, 4 = almost always). The range of total score is 22–88, with higher score indicating stronger tendency of ruminative thinking style, and vice versa. The current study used a reliable and valid Chinese version of RRS that was revised by Han and Yang (2009), which had good criterion validity and acceptable model fit in CFA, and showed excellent reliability among university students, α = .90. The internal consistency of the RRS in the present study was excellent, α = .92.
Vividness Scale
The vividness scale consists of one self-reported question in Chinese to measure the vividness of mental imagery to evaluate the participants’ engagement in training. The question was displayed on screen after each trial. The item was rated on five-point scale from 1 (not at all) to 5 (extremely).
Statistical Analysis
According to the effect size reported by Lang and her colleague (Lang et al. 2012), the effect size of group × time interaction on BDI-II is ηp2 = .19 (f = .48). We used f = .40 as a conservative estimate of effect size. Calculated by G*Power 3.1.9.2, a total of 34 participants would be needed to provide 80% power to detect a significant group × time interaction on the primary outcome at a significance level of 5%, two-tailed. We intended to recruit 42 participants to allow for attrition up to 20%.
Statistical analysis was carried out by IBM SPSS Statistics 21. Independent samples t-test and Chi-square tests were used to examine the group difference of target variables and demographics at baseline. Two-way repeated-measures MANOVA was used to examine the differences in change among target variables across the three time-points between two groups, where group is between-group factor (training group vs. wait-list) and time is within-group factor (pre-training, post-training, and follow-up). Chi-square and Fisher’s exact tests were used to detect the clinically significant change of PMIT on depression, where clinical significance is defined by the reliable change index (RCI). According to Jacobson and Truax (1991) RCI is change index at 95% confident interval calculated by the reliability of measurement. Our study adopted the RCI of 7.16 calculated by Blackwell and Holmes (2010) that followed the method proposed by Jacobson and Truax (1991). Clinically significant change was met when the change scores of BDI-II was larger than 7.16. Decline of severity was not used as a criterion to decide clinically significant change in this study because some participants’ severity of depression was categorized as minimal level, which means they would not be able to move to a lower level.
Results
Participants
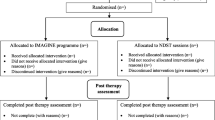
Recruitment started from November 2017. All follow-ups were conducted by June 2018. Demographic variables and the outcomes of MINI are shown in Table 1. A total of 176 of students were screened, 66 students were identified as eligible participants, and 51 of them completed baseline assessment. Among those completed assessment at baseline, 44 of them finished a second assessment after four-week since the first assessment was done, 41 completed the final assessment (see Fig. 2). Demographic and clinical characteristics are shown in Table 2.
For those who thoroughly completed the training and all assessments, training group consisted of 7 (31.8%) men and 15 (68.2%) women with a mean age of 22.1 (SD = 2.8) and a mean BDI-II score of 15.73 (7.5). Among them, there were 11 (52.4%) undergraduates, 10 (47.6%) master students, and 1(4.8%) PhD student. The wait-list included 6 men and 13 women with a mean age of 21.5 (SD = 1.8) and a mean BDI-II score of 13.9 (7.7). Among them, there were 10 (52.6%) undergraduates, 5 (26.3%) master students, and 4 (21.1%) PhD students. The rate of screen-positive (i.e. identified as eligible participants) is 37.5% and the attrition rate at post-intervention assessment for interventional group and the wait-list is 20% and 4.8%. The intervention completion rate of those who completed all assessments was 94.3%.
Baseline Measures
A significant difference was observed in educational level, Fisher’s exact test: p = .043. There were no significant group differences discovered in terms of sex, age, BDI-II, PA, NA, and RRS, sex: χ 2 = .26, p = .607; age, t(49) = .14, p = .891; BDI-II: t(49) = .90, p = .372: PA = t(49) = .75, p = .460; NA: t(49) = 1.23, p = .226; RRS: t(49) = .1.35, p = .184. For those who thoroughly completed the training and all assessments, the differences between two groups in terms of BDI-II, PA, NA, and RRS scores at baseline were not significant, BDI-II: t(39) = .79, p = .434, PA: t(39) = 1.11, p = .273, NA: t(39) = 1.31, p = .200, RRS: t(39) = 1.19, p = .243. There was no significant difference on gender and educational level between two groups, gender: χ2 = .000, p = .987; educational level: Fisher’s exact test: p = .200. Table 2 shows the correlations between baseline measures. The average vividness scores of training group is 3.53 ± .58.
Primary Outcomes
No significant differences were found on BDI-II, PA, NA, and RRS between the controls who fully completed all assessments at three time points and those did not, BDI-II: t(19) = .69, p = .501; PA: t(19) = 1.44, p = .167; NA: t(19) = −1.04, p = .312; RRS: t(19) = 1.00, p = .331. In training group, there were no significant differences between participants who fully completed the assessment at three time points and those who did not, BDI-II: t(28) = −.40, p = .695; PA: t(28) = .13, p = .901; NA: t(28) = −.04, p = .965: RRS: t(28) = 1.90, p = .069.
A MANOVA was conducted with group and time as independent variables on BDI-II, PA, NA, and RRS. Mauchly’s assumptions were met, BDI-II: χ2 = 2.40, p = .302; PA: χ2 = .66, p = .718; NA: χ2 = 4.38, p = .112; RRS: χ2 = 1.50, p = .473. There was a significant group × time interaction on BDI-II, PA, NA, and RRS, F(8,150) = 2.19, p = .031, Wilks’ Lambda = .80, ηp2 = .105. Significant interaction effects on univariate ANOVA of the above variables was also found: BDI-II: F(2, 78) = 5.82, p = .004, ηp2 = .130; PA: F(2, 78) =3.22, p = .045, ηp2 = .076; NA: F(2, 78) = 3.81, p = .026, ηp2 = .089; RRS: F(2, 78) = 3.80, p = .027, ηp2 = .089. There were significant main effects of time on the all outcome variables except RRS, BDI-II: F(2, 78) = 11.88, p < .001, ηp2 = .223; PA: F(2, 78) = 4.54, p = .014, ηp2 = .104; NA: F(2, 78) = 5.33, p = .007, ηp2 = .120; RRS: F(2, 78) = 2.17, p = .121, ηp2 = .053. No main effect of group on all variables was found, ps > .05. Scores on outcome measures at pre-training, post-training and follow-up for the two groups are shown in Table 3.
Within Group Comparison
Means and standard deviations across all time points are shown in Table 3 and Figs. 3 and 4, and correlation coefficients, effect sizes (Cohen’s d), and 95% confident intervals of pairwise differences in change scores of key variables are shown in Table 4.
Training Group
A repeated measure ANOVA was conducted with time as independent variable on BDI-II, PA, NA, and RRS. Mauchly’s assumption of all variables is met, BDI-II:χ2(2) = 4.90, p = .086; PA: χ2(2) = .44, p = .801; NA: χ2(2) = 1.47, p = .478; RRS: χ2(2) = .37, p = .830. There are significant changes across the three time points on BDI-II, PA, NA, and RRS, BDI-II: F(2, 42) = 22.25, p < .001, ηp2 = .514; PA: F(2, 42) = 6.47, p = .004, ηp2 = .235; NA: F(2, 42) = 10.33, p < .001, ηp2 = .330; RRS: F(2, 42) = 5.18, p = .010, ηp2 = .198. After training, the BDI-II scores dropped significantly from pre-training to post-training, t(21) = 5.02, p < .001, d = .84, and from pre-training to follow-up, t(21) = 5.40, p < .001, d = .86. The PA score increased significantly from pre-training to post-training, t (21) = 3.66, p = .001, d = .63, and from pre-training to follow-up, t(21) = 2.13, p = .045, d = .45. The NA score decreased significantly from pre-training to post-training, t(21) = 3.61, p = .002, d = .64, and from pre-training to follow-up, t(21) = 4.67, p < .001, d = .62. The RRS score decreased significantly from pre-training to post-training, t(21) = 2.9, p = .008, d = .57, and from pre-training to follow-up, t(21) = 2.64, p = .971, d = .51.
Wait-List
A repeated measure ANOVA was conducted with time as independent variable on BDI-II, PA, NA, and RRS. Mauchly’s assumptions of all variables are met except RRS and BDI-II:χ2 (2) = .12, p = .941; PA: χ2 (2) = 1. 30, p = .538; NA: χ2 (2) = 4.68, p = .096, RRS: χ2(2) = 9.23, p = .010, adjusted by Greenhouse & Geisser, ε = .705. No significant changes was found across the three time points on BDI-II, PA, NA, and RRS, BDI-II in the wait-list, BDI-II: F(2, 36) = .93, p = .403, ηp2 = .049; PA: F(2, 36) = .54, p = .588, ηp2 = .029; PA: F(2, 36) = .51, p = .602, ηp2 = .028; Adjusted by Greenhouse & Geisser, RRS: F(1.409, 25.371) = .15, p = .860, ηp2 = .009.
Clinically Significant Change
At post-training, there are eight participants in the training group with a change score larger than RCI, while only two participants in the wait-list met this criterion, Fisher’s exact test, p = .075. At 4-week follow-up, eleven participants in training group had a change score greater than RCI, compared to only three participants in the wait-list, χ2 = 5.31, p = .021 (see Table 5).
Subgroup Analysis
Means and SDs of study variables for people with BDI-II ≥14 at three time points are presented in Table 6. No group difference was found in the BDI-II, PA, NA, and RRS at baseline, ps > .05. No significant interaction effects on univariate ANOVA of the above variables were found, ps > .05. No significant main effect of group of the above were found, ps > .05. There were significant main effects of time on BDI only, F(2, 46) = 11.81, p < .001, ηp2 = .339.
At post-training, there are eight participants in the training group with a change score larger than RCI, while only two participants in the wait-list met this criterion, Fisher’s exact test, p = .211. At 4-week follow-up, ten participants in training group had a change score greater than RCI, compared to only three participants in the wait-list, Fisher’s exact test, p = .111.
Discussion
The aim of the current study was to obtain estimates to inform sample size primary result of PMIT among Chinese population. It provided rate of screen-positive and attrition rate, effect sizes for sample size calculation for the definitive trial study. Furthermore, it examined the effect of positive mental imagery on depressive symptoms, positive and negative affect, and rumination among Chinese university students. Globally, there is a need to develop, adapt, scale-up and promote low-intensity psychological interventions for populations with mental health concerns but who are unlikely to seek a professional for help. To our knowledge, this was the first evaluation of the PMIT among Chinese adults. Due to the lack of psychological professionals and insufficient psychological services for university students in China (Hu 2010; Liu and Shi 2010), new interventions need to be evaluated that can reach a large group of students. PMIT is a novel and accessible psychological intervention for depression, which can be scaled up to reach people with psychological distress and reduce the treatment gap.
There is a change about the number of target participants in this study. The study originally targeted to have up to 42 eligible participants enrolled to the study, but 66 eligible participants were practically identified during the screening process. A general rule of thumb prefers larger sample size in clinical study, so a larger number of eligible participants seems to be innocuous to the study and participants.
The pilot study obtained estimates to inform sample size of the definitive trial. We obtained a screen-positive rate of 37.5%, using online social networking platform for recruitment. Meanwhile, a portion of registered participants were considered ineligible because they could not made to attend the study process. Overall, there are 71 out of 176 enrolled participants whom were not able to be contacted after effortful contact throughout the screening process or they were not in the city where the study was conducted. It is possible that the current study design limited potential participants from other Chinese areas to take part in the study, but it also showed that online advisement might reach participants without geographical barrier. Considering the strengths and weakness of this recruitment tunnel, online recruitment is considered an acceptable approach. The attrition rate is 20% at post-training, which is relatively high compared with previous studies (i.e., Blackwell et al. 2015; Torkan et al. 2014), but relatively lower than Torkan et al. (2014) in follow-up. A recent pilot study (Bibi et al. 2020) found a high attrition rate amongst university students in positive mental imagery intervention in post-intervention (17.2%) and particularly at follow-up (44.8%), and identified some possible factors hindering their participation, such as negotiating the schedule with other activity commitments and duration of training. Dropout of intervention in the current study was mainly caused by participants becoming busier or not being able to attend sessions due to their coursework. Collecting outcomes remotely was recommended to lower the attrition rate (Bibi et al. 2020). We conducted follow-up assessment online by sending the assessment link via email and obtained a lower attrition rate compared with the previous study at follow-up (44.8%, Bibi et al. 2020; 38.5%, Torkan et al. 2014). Our experience suggest that collecting outcomes remotely can reduce attrition in this population. Future studies are also suggested to deliver the intervention at students’ convenience (e.g., delivery online or allow them to practice at home instead of coming to a computer room) to reduce attrition.
Generally, a decline in depressive symptoms, negative affect, rumination, and an increase in positive affect were observed across time in the training group. Significant changes in depressive symptoms, positive and negative affect at post-training assessment, moderate to large effect size (d = .70–.95). In addition, there was an interaction effect of time and group. However, our result did not demonstrate a significant difference of the target variables between post-training and follow-up assessment.
Rumination involves cognitive processing related to depressive symptoms (Schafer et al. 2017; Watkins 2008). Our result supported that positive mental imagery training can effectively reduce ruminative thinking in training and follow-up, consistent with a previous study (Torkan et al. 2014). A previous internet-based mental imagery training also showed a similar effect on depressive symptoms (Pictet et al. 2016). Healthy individuals (BDI-II < 14) were included in our study, so the overall depressive level in our study was lower than studies used depressive sample, and that probably caused inconsistence in comparison with results of previous studies.
Affect is related to psychological health (Dixon-Gordon et al. 2015) in which cognitive processing is involved (Verstraeten et al. 2011). The improvement of affect can be attribute to the decrease of rumination (Verstraeten et al. 2011). Inconsistent with Murphy et al. (2015), our results not only showed a main effect time in NA, but also found an interaction effect in NA and PA and main effect of time in PA, which suggested that the PMIT can improve positive and negative mood in general. Overall, our result supports that positive mental imagery training can alleviate depressive symptoms, improve emotional well-being, and alter maladaptive thinking style. Individuals with depression were characterized by verbal and ruminative processing and a third-person perspective in mental imagery (Koster et al. 2011; Williams and Moulds 2007). Participants were trained to use concrete information and instruction to generate mental imagery from the first-person perspective during the training, which prevented them from using maladaptive strategies, and thus the symptoms were alleviated.
In terms of clinically significant change, our study found a trend toward significance at post training assessment. After the 4-week training, about 36% of participants in training group had a change score larger than RCI, which still hold a lower proportion comparing with similar studies by Lang et al. (2012) and (Torkan et al. 2014) where they adopted a stricter criterion to decide clinically significant change, 46.2% and 69.2% respectively. At follow-up, half of participants in training group had a change score larger than RCI. The difference of clinically significant change was significant between training group and the waiting-list. The result indicated that no sufficient evidence to support more participants in training group than the wait-list had mitigation of depression at post-training. However, it indicated that more participants in training group than the wait-list had mitigation of depression 4 week after post-training. Overall, comparison in terms of clinically changes with other studies cannot be fairly made because the composition of sample in our study is a mix of minimal to moderate depression.
Limitations
This study is a pilot study without randomization. Allocation was decided by participants’ application to PMIT in semester 1(training group) or a second semester (waitlist control group), which was helpful to increase their motivation to enroll in the study. However, participants were not randomly assigned, so other unmeasured factors might partially account for treatment outcome (Leon 2011), such as readiness of participation, and factors influencing motivation. According to report standards Quantitative Research in Psychology (Appelbaum et al. 2018), registration is not compulsory for studies using non-randomized assignment. However, studies without registration may lead to biases. Future studies should be registered and utilize randomized controlled trial design to minimize risk for bias and. In addition, using a wait list as a control comparison is not as strong as an active control (e.g., identical intervention but removing mental imagery procedure), which is recommended for future larger randomized controlled trial. Both participants and researchers were not blind to their condition in the current study, and future studies should avoid it and using a double-blind approach for eliminate bias. Although the actual training was different from the ideal experimental manipulation, it was more in line with real life conditions and has higher ecological validity, but a full trial is needed to evaluate treatment effectiveness.
This study included participants with minimal depression, who could possibly have little decrease in BDI-II across the study, which influenced the overall outcomes on depressive symptoms. Murphy et al. (2015) discovered that positive mental imagery training did not have interaction effect but a main effect of time on healthy population (mean BDI-II scores <5), which was partially consistent with our study. The inclusion of participants with minimal depression made it difficult to explore a rigorous clinically significant change and to interpret the effect of training on depressive symptoms in terms of BDI-II scores. In addition, the current study excluded serious psychotic problems, protentional cognitive dysfunction and suicidal risk to eliminate possible confounding and potential risk of severe mental illness and cognitive damage. These may lead a bias that people with severe depressive symptoms or non-severe depression serious psychopathological comorbidity were not included. Future study should decide a more rigorous criteria and evaluation for depression.
The measurements used in the study merely relied on self-report, which was consistent with previous studies on the topics of depressive symptoms, affectivity, and rumination (Blackwell et al. 2015; Murphy et al. 2015; Torkan et al. 2014). Structured clinical interview was not used as an assessment throughout the study. Future study is suggested to use clinical interview to evaluate depression at each assessment time-point to follow the status of depression and use more objective indicators such as bio-marker and implicit measurement. Moreover, the current study only included participants who responded to assessments at all three time points. Intention-to-treat analysis is recommended for future studies to eliminate bias caused by removing non-compliance, withdrawal, and missing data (Gupta 2011).
Conclusion
Our study obtained estimates for sample size calculation and acquire preliminary evidence of PMIT for a future definitive trial study. Future study is suggested to recruit participant via online and decide an adequate sample size by consulting the finding of the current study. Successful rumination reduction with the aid of PMIT might reduce students’ suicidal ideation (Miranda and Nolen-Hoeksema 2007). In addition, PMIT can work as a stand-alone intervention, which would be helpful to prepare clients for cognitive behavioral therapy (CBT) (Williams et al. 2015). A larger, more rigorous study is needed to examine the efficacy and effectiveness of PMIT among Chinese populations which is helpful to inform or aid in developing university psychological services, and are likely to reduce the treatment gap in university settings.
References
Andrade, L. H., Alonso, J., Mneimneh, Z., Wells, J. E., Al-Hamzawi, A., Borges, G., et al. (2014). Barriers to mental health treatment: Results from the WHO world mental health surveys. Psychological Medicine, 44, 1303–1317. https://doi.org/10.1017/s0033291713001943.
Appelbaum, M., Cooper, H., Kline, R. B., Mayo-Wilson, E., Nezu, A. M., & Rao, S. M. (2018). Journal article reporting standards for quantitative research in psychology: The APA publications and communications board task force report. The American Psychologist, 73, 3–25. https://doi.org/10.1037/amp0000191.
Bar-Haim, Y., Lamy, D., Pergamin, L., Bakermans-Kranenburg, M. J., & van IJzendoorn, M. H. (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133, 1–24. https://doi.org/10.1037/0033-2909.133.1.1.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for the Beck depression inventory-II. San Antonio, TX: Psychological Corporation.
Bibi, A., Margraf, J., & Blackwell, S. E. (2020). Positive imagery cognitive bias modification for symptoms of depression among university students in Pakistan: A pilot study. Journal of Experimental Psychopathology, 11, 2043808720918030. https://doi.org/10.1177/2043808720918030.
Blackwell, S. E., & Holmes, E. A. (2010). Modifying interpretation and imagination in clinical depression: A single case series using cognitive Bias modification. Applied Cognitive Psychology, 24, 338–350. https://doi.org/10.1002/acp.1680.
Blackwell, S. E., Browning, M., Mathews, A., Pictet, A., Welch, J., Davies, J., Watson, P., Geddes, J. R., & Holmes, E. A. (2015). Positive imagery-based cognitive Bias modification as a web-based treatment tool for depressed adults: A randomized controlled trial. Clinical Psychological Science: A Journal of the Association for Psychological Science, 3, 91–111. https://doi.org/10.1177/2167702614560746.
Bowler, J. O., Mackintosh, B., Dunn, B. D., Mathews, A., Dalgleish, T., & Hoppitt, L. (2012). A comparison of cognitive bias modification for interpretation and computerized cognitive behavior therapy: Effects on anxiety, depression, attentional control, and interpretive bias. Journal of Consulting and Clinical Psychology, 80, 1021–1033. https://doi.org/10.1037/a0029932.
Brans, K., Koval, P., Verduyn, P., Lim, Y. L., & Kuppens, P. (2013). The regulation of negative and positive affect in daily life. Emotion, 13, 926–939. https://doi.org/10.1037/a0032400.
Burnett Heyes, S., Pictet, A., Mitchell, H., Raeder, S. M., Lau, J. Y. F., Holmes, E. A., & Blackwell, S. E. (2017). Mental imagery-based training to modify mood and cognitive Bias in adolescents: Effects of valence and perspective. Cognitive Therapy and Research, 41, 73–88. https://doi.org/10.1007/s10608-016-9795-8.
Chen, L., Wang, L., Qiu, X. H., Yang, X. X., Qiao, Z. X., Yang, Y. J., & Liang, Y. (2013). Depression among Chinese university students: Prevalence and socio-demographic correlates. PLoS One, 8, e58379. https://doi.org/10.1371/journal.pone.0058379.
Davies, E. B., Morriss, R., & Glazebrook, C. (2014). Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: A systematic review and meta-analysis. Journal of Medical Internet Research, 16, e130. https://doi.org/10.2196/jmir.3142.
Dixon-Gordon, K. L., Aldao, A., & De Los Reyes, A. (2015). Repertoires of emotion regulation: A person-centered approach to assessing emotion regulation strategies and links to psychopathology. Cognition and Emotion, 29, 1314–1325. https://doi.org/10.1080/02699931.2014.983046.
Fredrickson, B. L. (2001). The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. The American Psychologist, 56, 218–226. https://doi.org/10.1037//0003-066x.56.3.218.
Grol, M., Vanlessen, N., & De Raedt, R. (2017). Feeling happy when feeling down: The effectiveness of positive mental imagery in dysphoria. Journal of Behavior Therapy and Experimental Psychiatry, 57, 156–162. https://doi.org/10.1016/j.jbtep.2017.05.008.
Gupta, S. K. (2011). Intention-to-treat concept: A review. Perspectives in Clinical Research, 2, 109–112. https://doi.org/10.4103/2229-3485.83221.
Hall, B. J., Xiong, P., Guo, X., Sou, E. K. L., Chou, U. I., & Shen, Z. (2018). An evaluation of a low intensity mHealth enhanced mindfulness intervention for Chinese university students: A randomized controlled trial. Psychiatry Research, 270, 394–403. https://doi.org/10.1016/j.psychres.2018.09.060.
Han, X., & Yang, H.-F. (2009). Chinese version of Nolen-Hoeksema ruminative responses scale (RRS) used in 912 college students: Reliability and validity. Chinese Journal of Clinical Psychology, 17, 550–551.
Holmes, E. A., & Mathews, A. (2005). Mental imagery and emotion: A special relationship? Emotion, 5, 489–497. https://doi.org/10.1037/1528-3542.5.4.489.
Hu, W. (2010). Problems and countermeasures in the psychological Counselling of local universities. China Higher Education Research, 75-77.
Huang, J., & Wang, Y. (2015). Cognitive Bias modification: Paradigm and effectiveness. Chinese. Journal of Clinical Psychology, 23, 443–447. https://doi.org/10.16128/j.cnki.1005-3611.2015.03.014.
Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. https://doi.org/10.1037//0022-006x.59.1.12.
Jiang, C. X., Li, Z. Z., Chen, P., & Chen, L. Z. (2015). Prevalence of depression among college-goers in mainland China: A methodical evaluation and meta-analysis. Medicine (Baltimore), 94, e2071. https://doi.org/10.1097/md.0000000000002071.
Koster, E. H., De Lissnyder, E., Derakshan, N., & De Raedt, R. (2011). Understanding depressive rumination from a cognitive science perspective: The impaired disengagement hypothesis. Clinical Psychology Review, 31, 138–145. https://doi.org/10.1016/j.cpr.2010.08.005.
Lang, T. J., Blackwell, S. E., Harmer, C. J., Davison, P., & Holmes, E. A. (2012). Cognitive Bias modification using mental imagery for depression: Developing a novel computerized intervention to change negative thinking styles. European Journal of Personality, 26, 145–157. https://doi.org/10.1002/per.855.
Lei, X. Y., Xiao, L. M., Liu, Y. N., & Li, Y. M. (2016). Prevalence of depression among Chinese University students: A meta-analysis. PLoS One, 11, e0153454. https://doi.org/10.1371/journal.pone.0153454.
Leon, A. C. (2011). Evaluation of psychiatric interventions in an observational study: Issues in design and analysis. Dialogues in Clinical Neuroscience, 13, 191–198.
Levens, S. M., & Gotlib, I. H. (2009). Impaired selection of relevant positive information in depression. Depression and Anxiety, 26, 403–410. https://doi.org/10.1002/da.20565.
Liu, R., & Shi, L. (2010). Investigation of college psychological Counselling. Social Science of Beijing, 3, 88–91.
MacLeod, C., & Mathews, A. (2012). Cognitive bias modification approaches to anxiety. Annual Review of Clinical Psychology, 8, 189–217. https://doi.org/10.1146/annurev-clinpsy-032511-143052.
Miranda, R., & Nolen-Hoeksema, S. (2007). Brooding and reflection: Rumination predicts suicidal ideation at 1-year follow-up in a community sample. Behaviour Research and Therapy, 45, 3088–3095. https://doi.org/10.1016/j.brat.2007.07.015.
Murphy, S. E., Clare O'Donoghue, M., Drazich, E. H., Blackwell, S. E., Christina Nobre, A., & Holmes, E. A. (2015). Imagining a brighter future: The effect of positive imagery training on mood, prospective mental imagery and emotional bias in older adults. Psychiatry Research, 230, 36–43. https://doi.org/10.1016/j.psychres.2015.07.059.
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology, 61, 115–121. https://doi.org/10.1037//0022-3514.61.1.115.
Nolen-Hoeksema, S., McBride, A., & Larson, J. (1997). Rumination and psychological distress among bereaved partners. Journal of Personality and Social Psychology, 72, 855–862. https://doi.org/10.1037//0022-3514.72.4.855.
Pictet, A., Jermann, F., & Ceschi, G. (2016). When less could be more: Investigating the effects of a brief internet-based imagery cognitive bias modification intervention in depression. Behaviour Research and Therapy, 84, 45–51. https://doi.org/10.1016/j.brat.2016.07.008.
Qiu, L., Zheng, X., & Wang, Y. (2008). Revision of the positive affect and negative affect Scal. Chinese Journal of Applied Psychology, 17, 550–551.
Renner, F., Ji, J. L., Pictet, A., Holmes, E. A., & Blackwell, S. E. (2017). Effects of engaging in repeated mental imagery of future positive events on Behavioural activation in individuals with major depressive disorder. Cognitive Therapy and Research, 41, 369–380. https://doi.org/10.1007/s10608-016-9776-y.
Saleh, D., Camart, N., Sbeira, F., & Romo, L. (2018). Can we learn to manage stress? A randomized controlled trial carried out on university students. PLoS One, 13, e0200997. https://doi.org/10.1371/journal.pone.0200997.
Schafer, J. O., Naumann, E., Holmes, E. A., Tuschen-Caffier, B., & Samson, A. C. (2017). Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta-analytic review. Journal of Youth and Adolescence, 46, 261–276. https://doi.org/10.1007/s10964-016-0585-0.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The Mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(Suppl 20), 22–33 quiz 34-57.
Shi, M., Liu, L., Wang, Z. Y., & Wang, L. (2016). Prevalence of depressive symptoms and its correlations with positive psychological variables among Chinese medical students: An exploratory cross-sectional study. BMC Psychiatry, 16, 3. https://doi.org/10.1186/s12888-016-0710-3.
Tang, F., Byrne, M., & Qin, P. (2018). Psychological distress and risk for suicidal behavior among university students in contemporary China. Journal of Affective Disorders, 228, 101–108. https://doi.org/10.1016/j.jad.2017.12.005.
Torkan, H., Blackwell, S. E., Holmes, E. A., Kalantari, M., Neshat-Doost, H. T., Maroufi, M., & Talebi, H. (2014). Positive imagery cognitive Bias modification in treatment-seeking patients with major depression in Iran: A pilot study. Cognitive Therapy and Research, 38, 132–145. https://doi.org/10.1007/s10608-014-9598-8.
Verstraeten, K., Bijttebier, P., Vasey, M. W., & Raes, F. (2011). Specificity of worry and rumination in the development of anxiety and depressive symptoms in children. The British Journal of Clinical Psychology, 50, 364–378. https://doi.org/10.1348/014466510x532715.
Wang, Z., Yuan, C., Huang, J., Li, Z., Chen, J., Zhang, H., et al. (2011). Reliability and validity of the Chinese version of Beck depression inventory-II among depression patients. Chinese Mental Health Journal, 25, 476–480. https://doi.org/10.3969/j.issn.1000-6729.2011.06.014.
Watkins, E. R. (2008). Constructive and unconstructive repetitive thought. Psychological Bulletin, 134, 163–206. https://doi.org/10.1037/0033-2909.134.2.163.
Watson, D., Clark, L. A., & Carey, G. (1988). Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology, 97, 346–353. https://doi.org/10.1037//0021-843x.97.3.346.
Williams, A. D., & Moulds, M. L. (2007). Cognitive avoidance of intrusive memories: Recall vantage perspective and associations with depression. Behaviour Research and Therapy, 45, 1141–1153. https://doi.org/10.1016/j.brat.2006.09.005.
Williams, A. D., O'Moore, K., Blackwell, S. E., Smith, J., Holmes, E. A., & Andrews, G. (2015). Positive imagery cognitive bias modification (CBM) and internet-based cognitive behavioral therapy (iCBT): A randomized controlled trial. Journal of Affective Disorders, 178, 131–141. https://doi.org/10.1016/j.jad.2015.02.026.
Yang, W., Wu, D., & Peng, F. (2012). Application of Chinese version of Beck depression inventory-if to Chinese first-year college students. Chinese Journal of Clinical Psychology, 6, 762–764.
Yang, W., Lin, L., Zhu, W., & Liang, S. (2015). An introduction to mental health services at universities in China. Mental Health & Prevention, 3, 11–16. https://doi.org/10.1016/j.mhp.2015.04.001.
Funding
This work was supported by the Beijing Shangshan Foundation and the National Natural Science Foundation of China under grant number 31271094.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study procedures were approved by the Correspondence Author’s Institutional Review Board.
Informed Consent
Participants provided written informed consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sit, H.F., Hall, B.J., Wang, Y. et al. The effect of positive mental imagery training on Chinese University students with depression: A pilot study. Curr Psychol 41, 3716–3729 (2022). https://doi.org/10.1007/s12144-020-00867-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12144-020-00867-1