Abstract
The fifth (5th) edition of the World Health Organization (WHO) Classification of Head and Neck Tumors introduces a new chapter dedicated to soft tissue neoplasms commonly affecting the head and neck. While the diversity, rarity, and wide anatomic range of soft tissue tumors precludes a discussion of all entities that may be found in the head and neck, the addition of this new chapter to the head and neck "blue book" aims to provide a more comprehensive and uniform reference text, including updated diagnostic criteria, of mesenchymal tumor types frequently (or exclusively) arising at head and neck sites. Since publication of the previous edition in 2017, there have been numerous advances in our understanding of the pathogenesis of many soft tissue tumors which have facilitated refinements in tumor classification, identification of novel entities, development of diagnostic markers, and improved prognostication. This review will provide a focused discussion of the soft tissue tumors included in the 5th edition WHO Head and Neck classification, with an emphasis on updates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soft tissue neoplasms often pose diagnostic challenges in head and neck pathology, due to their diversity and overlapping histologic spectra. A vast number of soft tissue tumors may arise throughout the upper aerodigestive tract and salivary glands, and some entities arise preferentially or nearly exclusively in specific anatomic sites. The fourth (4th) edition World Health Organization (WHO) Classification of Head and Neck Tumors (2017) [1] included a small number of relevant soft tissue tumors within each site-specific chapter. The fifth (5th) edition of the WHO Classification of Head and Neck Tumors [2] now includes a dedicated chapter for soft tissue tumors, providing a centralized and more practical reference to aid pathologists in the diagnosis of these challenging tumors. This chapter is organized by line of differentiation, mirroring the 5th edition of WHO Classification of Soft Tissue and Bone Tumors (published in 2020) [3]: adipocytic, fibroblastic and myofibroblastic, vascular, pericytic (perivascular), smooth muscle, skeletal muscle, chondro-osseous, peripheral nerve sheath, tumors of uncertain differentiation, and undifferentiated small round cell sarcomas. A small number of anatomic site-specific mesenchymal tumors remain in their respective chapters, including biphenotypic sinonasal sarcoma in "Soft Tissue Tumors of the Nasal Cavity, Paranasal Sinuses, and Skull Base" and ectomesenchymal chondromyxoid tumor in "Oral Cavity and Mobile Tongue." This review is a focused discussion of the soft tissue tumors included in the 5th edition WHO Classification of Head and Neck Tumors, with an emphasis on recent advances in our understanding of tumor pathogenesis, diagnostic and prognostic criteria, and novel immunohistochemical markers. Table 1 summarizes the molecular genetic alterations and surrogate immunohistochemical markers of included entities.
Adipocytic Tumors
This section includes benign ("Lipoma family") and malignant ("Liposarcoma" family) entities. Lipomas are anatomically ubiquitous tumors of mature white fat, characterized by frequent HMGA2 rearrangement [4]. Angiolipomas are driven by PRKD2 mutations [5]. Spindle cell/pleomorphic lipoma commonly arise in the subcutis of the posterior neck, back and shoulder of adult men, and are characterized by frequent 13q14 deletions. This deletion includes the RB1 locus and corresponds with immunohistochemical loss of nuclear RB1 protein expression in neoplastic cells [6].
Atypical lipomatous tumor/well-differentiated liposarcoma (ALT/WDLPS) and dedifferentiated-liposarcoma (DDLPS) are the most likely liposarcoma subtypes to arise in head and neck sites, often in the upper aerodigestive tract [7]. The terms ALT and WDLPS are synonyms, with the former applied to tumors in sites where curative resection is possible (e.g. limbs). In the head and neck, such tumors are almost always classified as WDLPS given that margin-negative resection is often impossible due to anatomic constraints. ALT/WDLPS can progress to DDLPS, which most frequently appears as a non-lipogenic sarcoma and encompasses a broad range of morphologic appearances. High-grade DDLPS (based on the French Fédération Nationale des Centres de Lutte Contre le Cancer grading system) and DDLPS with myogenic differentiation (specifically rhabdomyoblastic) have been associated with worse outcomes [8,9,10,11]. ALT/WDLPS and DDLPS are associated with amplification of 12q13-15 via ring and giant marker chromosomes [12], while other amplified genes may contribute to tumor biology in ways that are not fully characterized. Immunohistochemistry for proteins encoded on this amplified locus, MDM2 and CDK4 (as well as HMGA2) has been established as diagnostic tools for ALT/WDLPS and DDLPS. Most cases show nuclear staining for MDM2 and CDK4, which is highly sensitive although not entirely specific for the diagnoses, as staining (albeit more limited) can be seen in other sarcomas, particularly those with polysomy 12 or low copy number increases in 12q, such as myxofibrosarcoma and malignant peripheral nerve sheath tumor [13]. Staining may also be seen in histiocytes, and fat necrosis may pose a pitfall for misinterpretation as ALT/WDLPS [14]. Fluorescence in situ hybridization (FISH) analysis to detect MDM2 gene amplification is considered the gold standard for ALT/WDLPS and DDLPS, being more sensitive and specific than immunohistochemistry [15], and confirmatory FISH testing is helpful in cases with equivocal or inconsistent MDM2/CDK4 staining and for cases of ALT/WDL and DDLPS arising in unusual sites.
Presentation of myxoid liposarcoma or pleomorphic liposarcoma in this anatomic region should always elicit a strong suspicion for metastasis, as both tumor types typically arise in the extremities and only rarely present primarily in the head and neck. Myxoid liposarcoma is defined by recurrent FUS-DDIT3 fusion (or rarely EWSR1-DDIT3) [16, 17]. DDIT3 immunohistochemistry is highly sensitive and specific for myxoid liposarcoma, including high-grade cases showing predominant round cell morphology [18, 19]. The term “round cell liposarcoma” is no longer endorsed by the WHO Classification of Soft Tissue and Bone Tumors, as the hypercellular areas of high-grade myxoid liposarcoma are not exclusively round cell in appearance. Pleomorphic liposarcoma has no specific immunophenotype or molecular features, and is notably indistinguishable from DDLPS showing "homologous" differentiation, both having characteristic regions of pleomorphic tumor cells resembling myxofibrosarcoma or unclassified pleomorphic sarcoma with variable foci of large atypical lipoblasts [20]; MDM2 and CDK4 are negative in pleomorphic liposarcoma.
Two new adipocytic entities are introduced in this edition: atypical spindle cell lipomatous tumor/atypical pleomorphic lipomatous tumor (ASLT/APLT) and myxoid pleomorphic liposarcoma. While ASLT/APLT is included in the "Liposarcoma family," it should be noted that these tumors have only a low risk of local recurrence (~ 12%) and virtually no risk for metastasis or dedifferentiation [21,22,23,24]. ASLT/APLT are histologically diverse tumors comprised of variable proportions of adipocytes, atypical spindle cells, lipoblasts, and floret-like giant cells, with a frequently myxoid or collagenous stroma (Fig. 1). Although showing some overlapping features with spindle cell/pleomorphic lipoma, ASLT/APLT differs by its wide anatomic distribution and infiltrative growth, and may have increased nuclear pleomorphism, with or without rare atypical mitotic figures which may prompt a misdiagnosis of pleomorphic liposarcoma. RB1 deletions (and immunohistochemical loss of nuclear expression) are characteristic of ASLT/APLT, although deletions of 13q14 are larger than those seen in spindle cell/pleomorphic lipoma, and span flanking genes (including TCBTB2, DLEU1, and ITM2B) [21,22,23]. ASLT/APLT shows variable staining for CD34 (60%), S-100 (40%), and desmin (20%). The so-called “dysplastic lipoma” (or “anisometric cell lipoma”) included in this volume is a controversial entity which likely represents a spindle cell-poor variant of ASLT/APLT, and as such was not included in the more comprehensive 5th edition Classification of Soft Tissue and Bone Tumours.
Myxoid pleomorphic liposarcoma has been reported in the head and neck, although its typical presentation is in the mediastinum of young patients [25, 26]. These tumors are aggressive and show mixed features of myxoid liposarcoma and pleomorphic liposarcoma. Diagnosis requires exclusion of characteristic molecular alterations of other liposarcoma mimics (e.g. MDM2 amplification and FUS-DDIT3). Genomic studies indicate RB1 inactivation secondary to large deletions of the 13q14 region [26, 27]. It should be noted that deletion or inactivation of the RB1 tumor suppressor is a common event in neoplasia and its presence in multiple subsets of lipomas and liposarcomas does not necessarily indicate a pathogenic relationship or tumor evolution between benign and malignant entities.
Fibroblastic and Myofibroblastic Tumors
Tumors of fibroblastic and myofibroblastic differentiation encompass the largest group of soft tissue neoplasms, five of which are included in the 5th edition WHO Head and Neck Classification: nodular fasciitis, desmoid fibromatosis, solitary fibrous tumor, low-grade myofibroblastic sarcoma, and inflammatory myofibroblastic tumor. Among these, only low-grade myofibroblastic sarcoma has no identified recurrent molecular alterations. Approximately 30% of cases show nuclear β-catenin staining (in the absence of CTNNB1 mutation), which may result in a misdiagnosis of desmoid fibromatosis. However, low-grade myofibroblastic sarcoma shows increased cellularity and cytologic atypia relative to desmoid fibromatosis [28]. Desmoid fibromatosis has CTNNB1 exon 3 mutations in the majority of sporadic cases, and a smaller subset are associated with APC mutations in the context of familial adenomatous polyposis [29, 30]. Both mutations result in nuclear β-catenin nuclear expression, although up to 20% of cases are negative by immunohistochemistry. With more sensitive next generation sequencing techniques CTNNB1 mutations can be detected in > 95% of non-APC mutated desmoids.
Nodular fasciitis has the pathognomonic presentation of rapid growth and spontaneous regression. Although once hypothesized to be a reactive process, nodular fasciitis is now understood to be a “transient” neoplasm, based on the presence of the hallmark recurrent MYH9-USP6 fusion [31].
Major insights have been made in the pathogenesis and prognostication of solitary fibrous tumor (SFT). SFT is composed of a haphazard arrangement of spindled and ovoid cells set within a collagenous stroma, with characteristic thin-walled "staghorn" vessels (Fig. 2A). In 2013, two groups reported recurrent NAB2-STAT6 fusion in SFT of all anatomic sites [32, 33]. Notably, the fusion results from a small paracentric inversion of chromosome 12q13 with variable breakpoints, which cannot be detected by karyotype or FISH. STAT6 immunohistochemistry is a useful surrogate marker and has proven to be highly sensitive and specific for SFT [34] (Fig. 2B). Secondary TERT promoter mutations and TP53 mutations have been identified to be associated with more aggressive behavior (including increased metastases) and dedifferentiation [35, 36].
The application of rigorous statistical analysis has resulted in improved prognostic criteria for SFT, with several validated multivariate risk models applicable to SFT of all sites, including SFT of the head and neck (but not meninges) available. These models describe low, intermediate, and high-risk tumor groups and replace the historical terminology of “benign” and “malignant” SFT, the use of which is now discouraged. The most widely adopted risk stratification three-tier model has shown to be reliable for predicting metastasis based on the variables of patient age, tumor size, mitotic count, and necrosis [37] (see Table 2). Separate risk calculators have been proposed by the French Sarcoma group, which predict overall survival, local recurrence, and metastasis based on various combinations of patient age, tumor site, mitotic count, and history of radiotherapy [38]. While site-specific risk models have been proposed to take into account the smaller size of head and neck tumors, there is as yet no biologic evidence to suggest that head and neck SFT behave differently than SFT arising at other extrameningeal sites in terms of metastatic potential, and local recurrence risk remains largely a matter of the completeness of surgical excision together with use of adjuvant radiation therapy.
Inflammatory myofibroblastic tumor (IMT) may arise in the head and neck, the larynx being the most common site. It has been well established that ALK rearrangements occur in up to 60% in IMT, particularly in younger patients [39]. ALK is paired with a broad range of 5’ fusion partners which all result in aberrant ALK homodimerization in the absence of ligand and constitutive activation. In the head and neck a recent series of IMTs in the head and neck, TIMP3 was the most frequent (~ 50%) fusion partner [40]. Most ALK-rearranged IMTs show cytoplasmic positivity for ALK by immunohistochemistry, which can helpful in distinguishing IMT from potential mimics in the head and neck, including sarcomatoid squamous cell carcinoma, embryonal rhabdomyosarcoma, and IgG4-sclerosing disease, although demonstration of rearrangement by FISH or NGS is the gold standard for detection of ALK rearrangements. Among the many ALK antibody clones available, 5A4 AND D5F3 are highly sensitive, particularly in the detection of ALK-rearranged lung adenocarcinomas [41]. A subset of ALK-negative IMT are driven by ROS1 fusions and are positive for ROS by immunohistochemistry [42]. Similarly to lung adenocarcinomas, IMT with ALK rearrangements respond to targeted therapy with Crizotinib [43, 44].
Vascular Tumors
Among the benign vascular tumors, one major advance is the discovery of FOSB or FOS fusions in epithelioid hemangioma [45, 46], which corresponds with nuclear expression for FOSB that is detectable by immunohistochemistry [47, 48]. Notably, epithelioid hemangioma can show morphologic features resembling the reactive process angiolymphoid hyperplasia with eosinophilia. Demonstration of FOS/FOSB rearrangements, when present, can aid in the diagnosis of epithelioid hemangioma in some difficult cases. Although not included in the WHO Classification for Head and Neck, it deserves mention that FOSB fusions (commonly SERPINE-FOSB or ACTB-FOSB) and FOSB nuclear staining are also a feature of pseudomyogenic hemangioendothelioma, a vascular neoplasm of intermediate biologic potential that was fully characterized in 2011 [47, 49,50,51]. These tumors show a characteristic multifocal presentation across multiple tissue planes, histologically resembling epithelioid sarcoma and myoid differentiation, and may rarely arise in the head and neck.
There are no major updates for Kaposi sarcoma, a vascular proliferation induced by HHV8 infection. Most cases in the head and neck present in the oral cavity, frequently the AIDS-related subtype. While some cases act aggressively, with widespread visceral involvement and poor response to treatment, Kaposi sarcoma is only locally aggressive and does not metastasize, and thus does not represent a true sarcoma.
Epithelioid hemangioendothelioma (EHE) is a malignant vascular neoplasm composed of epithelioid cells arranged in cords and strands in a myxohyaline stroma (Fig. 3A). Most cases harbor recurrent WWTR1-CAMA1 gene fusions [52], and CAMTA1 nuclear staining is a reliable marker in distinguishing EHE from other vascular tumors [53] (Fig. 3B). Vascular markers (ERG, CD31, and CD34) are positive. Up to 50% of cases may show keratin expression, which poses a diagnostic pitfall, particularly with myoepithelial neoplasms [54]. EHE harboring variant YAP1-TFE3 account for less than 5% of all EHEs [55], and show a distinctive histological appearance of tumor cells with abundant eosinophilic cytoplasm and more vasoformative and solid architecture. EHE with TFE3-YAP1 shows strong nuclear TFE3 staining, however the specificity of this marker is somewhat limited [55]. Since preparation of the 5th edition WHO, it has been reported that immunohistochemistry using an antibody for the C-terminus of YAP1 shows frequent (77%) nuclear loss in cases of EHE with TFE3-YAP1 and retained expression in nearly all mimics [56], and may serve as a helpful diagnostic adjunct given the limitations of TFE3.
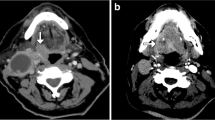
Angiosarcoma is an aggressive malignancy associated with poor outcomes, though histologic grade does not appear to predict prognosis. Most primary angiosarcomas in the head and neck have been reported in the sinonasal tract and oral cavity [57, 58] and show heterogeneous genetic features, including mutations in KDR, PTPRB, and PLCG1 [59,60,61]. Cutaneous angiosarcoma arises in sun-exposed areas of the head and neck and shows a high tumor mutational burden and ultraviolet damage mutational signature [61].
Pericytic (Perivascular) Tumors
Myofibroma and myopericytoma form a morphologic spectrum and are now classified together. Most tumors arise in adults, but some present at birth or during infancy. It has been discovered that PDGFRB mutation is the key pathogenic driver for both familial and sporadic cases of myofibroma and myopericytoma [62,63,64], further supporting their relationship. The rare variant of cellular (atypical) myofibroma has recently been described, which shows fascicular growth and can be infiltrative; these tumors may be confused with leiomyosarcoma as desmin staining is strong and diffuse (whereas desmin is largely negative in conventional myofibroma). Cellular myofibroma harbors recurrent SRF-RELA fusion [65].
Smooth Muscle Tumors
This section includes soft tissue leiomyoma and leiomyosarcoma, and introduces smooth muscle tumor of uncertain malignant potential for cases that fall between the diagnostic criteria of benign and malignant; most have been reported in sinonasal sites [66]. While formal criteria have not been established for smooth muscle tumors of uncertain malignant potential in soft tissue, published examples in the head and neck show increased cellularity, mild cytologic atypia, and mitotic counts of 4 or less per 2 mm2.
The major classification update is that EBV-associated smooth muscle tumor (EBV-SMT) is now listed separately from leiomyosarcoma, as EBV-SMT are indolent tumors that do not metastasize (although they may be multifocal), and are therefore not considered true sarcomas. EBV-SMT arises in the setting of immunosuppression, commonly HIV infection or post-organ transplantation, and prognosis is related to the patient’s degree of immunosuppression. EBV-SMT tend to show only mild-to-moderate cytologic atypia and pleomorphism, low mitotic activity, and infrequent necrosis; some cases may show a uniform ovoid or round cell component. Intratumoral T-lymphocytic infiltrates may be present. Smooth muscle markers SMA and caldesmon are positive but desmin is more variable. Detection of EBV-encoded RNA by in situ hybridization is diagnostic and should be considered for smooth muscle tumors arising in immunocompromised patients or a well-differentiated smooth muscle neoplasm showing unusual cellular uniformity and inflammation.
Skeletal Muscle Tumors
Benign rhabdomyomas and many rhabdomyosarcoma subtypes arise frequently in the head and neck. There are no major updates for fetal-type and adult-type rhabdomyomas. The 5th edition WHO Head and Neck Classification includes all four rhabdomyosarcoma subtypes: embryonal, alveolar, spindle cell/sclerosing, and pleomorphic. While all subtypes are positive for skeletal muscle markers desmin, MYOD1, and myogenin, diffuse myogenin staining is a specific feature of alveolar rhabdomyosarcoma [67]. This pattern is especially helpful in distinguishing alveolar rhabdomyosarcoma from examples of poorly differentiated embryonal rhabdomyosarcoma with predominant round cell morphology. PAX3-FOXO1 (and less commonly PAX7-FOXO1) is the genetic hallmark of alveolar rhabdomyosarcoma [68]. Recently, immunohistochemistry using an antibody for the PAX3/7-FOXO1 fusion protein has been shown to be highly sensitivity and specific for alveolar rhabdomyosarcoma, specifically for cases with PAX3-FOXO1 (but less reliable for cases with PAX7-FOXO1) [69]. It is important to remember that keratin and neuroendocrine markers are positive in a subset of alveolar rhabdomyosarcoma, which can lead to a mistaken diagnosis of neuroendocrine carcinoma [70, 71].
Recent discoveries identifying different recurrent molecular alterations in spindle cell/sclerosing rhabdomyosarcoma support its division into several clinicopathologic subgroups. Three main groups have emerged thus far: (1) congenital/infantile tumors with fusions involving VGLL2 and NCOA2 that are associated with favorable prognosis [72, 73]; (2) tumors with MYOD1 mutations predominantly arising in adolescent and young adults that show aggressive behavior [74,75,76,77]; and (3) tumors lacking known recurrent molecular genetic alterations. Diffuse staining for MYOD1 is a feature of MYOD1-mutant tumors (Fig. 4). There is also a newly recognized variant of spindle cell/sclerosing rhabdomyosarcoma associated with EWSR1/FUS-TFCP2 or MEIS-NCOA2 fusions [78, 79]; this variant arises preferentially in the bone and can show positivity for keratin and ALK, which may pose diagnostic pitfalls (and is listed in the "Odontogenic and maxillofacial bone tumors" chapter).
Chondro-osseous Tumors
The single included entity in this section, soft tissue chondroma, only rarely arises in head and neck sites. Recurrent FN1-FGFR2 and FN1-FGFR1 fusions have been identified in 50% and are associated with grungy calcifications [80]. However, such cases do not show elevated FGF23 mRNA expression and are thus unrelated to phosphaturic mesenchymal tumor, which is also characterized by grungy calcifications and FN1-FGFR1 fusion. Although not included in this edition, synovial chondromatosis may arise in the temporomandibular joint. Tumors are comprised of multiple nodules of hyaline cartilage which may undergo endochondral ossification if longstanding. Similar to soft tissue chondroma, synovial chondromatosis frequently demonstrates FN1 rearrangement, however ACVR2A is the most common 3’ partner, seen in 56% [81].
Peripheral Nerve Sheath Tumors
This section includes the well characterized benign entities neurofibroma (characterized by NF1 inactivation), schwannoma (associated with NF2 inactivation), and neuroma. The neuroma section groups together traumatic neuroma and solitary circumscribed neuroma with syndrome-associated mucosal neuromas (MEN2B-mucosal neuroma, oral pseudoperineurioma, and PIK3CA-related overgrowth spectrum-associated neuroma (PIK3CA-neuroma)).
Granular cell tumor is listed separately in the "Oral Cavity and Mobile Tongue" chapter, but warrants mention as tumors can arise elsewhere such as the larynx. Granular cell tumor is now known to harbor frequent (~ 70%) inactivating mutations of ATP6AP1 and ATP6AP2 [82, 83], which encode endosomal pH regulators. Interestingly, these pathogenic events show a phenotypic association, resulting in abnormal accumulation of intracytoplasmic granules that is a characteristic feature of these tumors.
There have been important insights into the pathogenesis of malignant peripheral nerve sheath tumor (MPNST). MPNST appears as a fascicular spindle cell sarcoma and diagnosis can be challenging as neural markers (S-100, SOX10, and GFAP) are frequently negative. Association with a large nerve, the setting of neurofibromatosis type 1, or history of radiation are helpful features. The majority (80%) of cases show SUZ12 or EED mutations, which encode subunits of the polycomb repressive complex 2 (PRC2) [84, 85]. Resultant dysregulation of PRC2 function leads to loss of the trimethylation mark on histone 3 lysine 27 (H3K27me3), which can be detected by immunohistochemistry (Fig. 5). Immunohistochemistry demonstrating loss of H3K27me3 is overall a useful diagnostic marker for MPNST, specifically for high grade and radiation-associated tumors, although specificity is somewhat limited, as loss of expression can be seen in small subsets of other malignancies, including synovial sarcoma, melanoma, and non-MPNST radiation-associated sarcomas [86,87,88,89,90], as well as some carcinomas.
Tumors of Uncertain Differentiation
This category comprises a diverse group of soft tissue neoplasms for which there is no identifiable line of differentiation. There remains a section for "undifferentiated sarcoma" which is a heterogeneous group and strictly a diagnosis of exclusion, after thorough histologic evaluation, application of relevant ancillary studies, and clinical correlation. These undifferentiated sarcomas are typically reported descriptively based on predominant morphologic pattern (round cell, spindle cell, epithelioid, and pleomorphic). Many tumors in this group are high-grade pleomorphic sarcomas and associated with poor prognosis. Genetic subsets and putative novel entities are increasingly being identified among these undifferentiated tumors, particularly within the round cell group.
Phosphaturic mesenchymal tumor is included in the head and neck classification for the first time. These tumors may arise in the soft tissue or bone of adults with a wide anatomic distribution, including head and neck. As mentioned earlier, these tumors harbor FN1-FGFR1 fusion, and are associated with tumor-induced osteomalacia secondary to secretion of FGF23 which leads to renal wasting of phosphate [91,92,93]. Tumors are comprised of sheets of bland, spindle and stellate cells associated with hemangiopericytoma-like vessels and frequently admixed with osteoclast-like giant cells. The tumor cells produce distinctive "grungy" appearing stromal calcifications (Fig. 6). Most tumors are benign and osteomalacia typically resolves after resection.
The section for myxoma refers to the benign myxoid neoplasms that can be associated with Carney complex (distinct from the entities odontogenic myxoma and intramuscular myxoma). These myxomas are histologically indistinguishable from superficial angiomyxoma. Presentation in the upper aerodigestive tract is rare, but has been reported in the sinonasal tract and larynx. Carney complex should be considered in the following settings: myxomas in the external auditory ear, multiple cutaneous myxomas, and/or presence of other clinical stigmata (such as spotty pigmentation and malignant melanotic nerve sheath tumor). Germline inactivating PRKAR1A mutations occur in Carney complex [94], and immunohistochemical loss of PRKAR1A is seen in Carney complex-associated tumors, including cardiac myxoma, malignant melanotic nerve sheath tumor, and superficial angiomyxoma [95, 96]. PRKAR1A mutation also appears to be a feature of sporadic counterparts, as sporadic superficial angiomyxoma may show immunohistochemical loss of expression of PRKAR1A [97].
Extraskeletal myxoid chondrosarcoma is only rarely encountered in the head and neck, but shows histologic overlap with soft tissue and salivary myoepithelial neoplasms. It should be noted that despite the terminology, tumors show no evidence of cartilaginous differentiation. Microscopically, tumors demonstrate lobulated growth with intervening fibrous septa, with uniform ovoid cells arranged in interconnected corded, reticular, and trabecular growth patterns embedded in an abundant chondromyxoid stroma. EWSR1-NR4A3 fusion is the molecular hallmark [98]. Molecular testing may be necessary as tumors have a non-specific immunophenotype, with only variable staining for S-100 (20%). While INSM1 is frequently positive (80%), specificity is somewhat limited [99].
It has been well established that synovial sarcoma harbors recurrent SS18-SSX fusions, involving one of three highly homologous SSX genes (SSX1, SSX2, or SS4) [100]. Most synovial sarcomas appear as uniform spindle cell sarcomas that enter the differential diagnosis of entities such as MPNST and biphenotypic sinonasal sarcoma. While most are monophasic with purely spindled morphology, approximately one third are biphasic showing an epithelial component (often glandular) admixed with spindle cells. Poorly differentiated variants show predominant round cell morphology and are associated with more aggressive behavior. Focal-to-multifocal EMA (and infrequent keratin) staining may be seen across all subtypes. The conventional immunohistochemical marker TLE1 is frequently used, and while sensitivity for synovial sarcoma is high, specificity is only moderate [101,102,103]. Recently, the SS18-SSX fusion-specific antibody and an SSX C-terminus-specific antibody have both been shown to have high sensitivity and specificity for synovial sarcoma, including poorly differentiated tumors, and can serve as reliable immunohistochemical surrogates for molecular testing [104, 105] (Fig. 7).
Lastly, there is a section for the emerging group of GLI1-altered mesenchymal tumors, including tumors having GLI1 rearrangement (~ 2/3 of cases; most commonly ACTB-GLI1) and GLI1 amplification (~ 1/3) [106]. Among the fewer than 40 cases reported in the literature, approximately 40% arise in the head and neck, most commonly on the tongue [107]. ACTB-GLI1 was first reported in 2004 in five tumors termed "pericytoma with t(7;12)" on the basis of SMA expression and indolent behavior [108]. Subsequent descriptions of similar tumors having GLI1 fused to ACTB, PTCH1, or MALAT1 demonstrated a significant risk of metastasis (~ 20%) [107, 109, 110]. The morphologic spectrum of these tumors is broad, but commonly shows nested and sheetlike growth of epithelioid, ovoid, or spindled tumor cells, with ovoid to round nuclei and eosinophilic or cleared cytoplasm. Intervening thin-walled vessels between tumor nests is a common feature, frequently with tumor cells protruding into vascular spaces. The immunophenotype is inconsistent and non-specific; S-100 is most likely to be positive (60%) and there is variable staining for SMA, CD99, EMA, and keratin. GLI1 amplifications often include flanking genes CDK4, MDM2, and STAT6¸which corresponds with MDM2, CDK4, and STAT6 staining [106]. It remains to be determined whether this provisional group represents a uniform clinicopathologic entity.
Undifferentiated Small Round Cell Sarcomas of Bone and Soft Tissue
This section of the WHO Head and Neck classification is devoted to Ewing sarcoma, as 10% of cases (both extra- and intraosseous) may arise in this anatomic region. Ewing sarcoma, the first sarcoma type recognized to have a recurrent cytogenetic abnormality, harbors EWSR1-FLI1 fusion [111], with rare variant fusions involving other members of the ETS (erythroblast transformation specific) family (e.g. EWSR1-ERG) and FUS in lieu or EWSR1. Integration of clinical, morphologic, and immunohistochemical features should guide confirmatory molecular testing. While not specific, Ewing sarcoma characteristically shows diffuse membranous CD99 staining. NKX2.2 has been shown to have high sensitivity (93%), although specificity is moderate as staining can be seen in several mimics including small cell carcinoma, olfactory neuroblastoma, and mesenchymal chondrosarcoma [112, 113]. There are now recognized genetic subsets among undifferentiated round cell sarcomas that were often classified as "atypical Ewing sarcoma", including CIC-rearrangement, BCOR alterations, and EWSR1 fusions to non-ETS partner genes, which are detailed in the 5th edition WHO Soft Tissue and Bone Classification [3].
Adamantinoma-like Ewing sarcoma is introduced in this section. Deeper characterization over the recent years has shown that tumors frequently arise in the head and neck, particularly salivary gland [114, 115]. Adamantinoma-like Ewing sarcoma also harbors EWSR1-FLI1 fusion, and some authors regard this as a variant of Ewing sarcoma that demonstrates epithelial differentiation. Tumors show lobules, nests, and sheets of uniform basaloid cells, often with peripheral nuclear palisading, and a frequently hyalinized or myxoid stroma (Fig. 8A). Tumors show diffuse positivity for keratin and p40 (Fig. 8B, C); rarely keratin pearl formation is seen. Basaloid carcinomas among other round cell sarcomas enter the differential diagnosis. CD99 and NKX2.2 are positive, similar to conventional Ewing sarcoma (Fig. 8D). It remains to be determined whether this distinctive entity is truly related to Ewing sarcoma or is a carcinoma that shares an identical fusion, and further investigation is needed to determine optimal management as a sarcoma or carcinoma.
Summary
The 5th edition WHO Classification of Head and Neck Tumors introduces a new chapter dedicated to soft tissue tumors and provides an updated text of the clinicopathologic and molecular features of both common and rare neoplasms encountered in the head and neck. This updated classification will ideally facilitate more accurate diagnosis and increased understanding of these challenging tumor types, leading to improved patient care.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ. WHO Classification of tumours: pathology and genetics of head and neck tumours. Lyon: IARC Press; 2017.
WHO Classification of Tumours Editorial Board. Head and neck tumours. 5th ed. Lyon: International Agency for Research on Cancer; 2022.
WHO Classification of Tumours Editorial Board. Soft tissue and bone tumours. 5th ed. Lyon: International Agency for Research on Cancer; 2020.
Bianchini L, Birtwisle L, Saâda E, Bazin A, Long E, Roussel JF, et al. Identification of PPAP2B as a novel recurrent translocation partner gene of HMGA2 in lipomas. Genes Chromosomes Cancer. 2013;52(6):580–90.
Hofvander J, Arbajian E, Stenkula KG, Lindkvist-Petersson K, Larsson M, Nilsson J, et al. Frequent low-level mutations of protein kinase D2 in angiolipoma. J Pathol. 2017;241(5):578–82.
Chen BJ, Marino-Enriquez A, Fletcher CD, Hornick JL. Loss of retinoblastoma protein expression in spindle cell/pleomorphic lipomas and cytogenetically related tumors: an immunohistochemical study with diagnostic implications. Am J Surg Pathol. 2012;36(8):1119–28.
Fritchie K, Ghosh T, Graham RP, Roden AC, Schembri-Wismayer D, Folpe A, et al. Well-differentiated/dedifferentiated liposarcoma arising in the upper aerodigestive tract: 8 cases mimicking non-adipocytic lesions. Head Neck Pathol. 2020;14(4):974–81.
Keung EZ, Hornick JL, Bertagnolli MM, Baldini EH, Raut CP. Predictors of outcomes in patients with primary retroperitoneal dedifferentiated liposarcoma undergoing surgery. J Am Coll Surg. 2014;218(2):206–17.
Jour G, Gullet A, Liu M, Hoch BL. Prognostic relevance of Fédération Nationale des Centres de Lutte Contre le Cancer grade and MDM2 amplification levels in dedifferentiated liposarcoma: a study of 50 cases. Mod Pathol. 2015;28(1):37–47.
Gronchi A, Collini P, Miceli R, Valeri B, Renne SL, Dagrada G, et al. Myogenic differentiation and histologic grading are major prognostic determinants in retroperitoneal liposarcoma. Am J Surg Pathol. 2015;39(3):383–93.
Kurzawa P, Mullen JT, Chen YL, Johnstone SE, Deshpande V, Chebib I, et al. Prognostic value of myogenic differentiation in dedifferentiated liposarcoma. Am J Surg Pathol. 2020;44(6):799–804.
Hostein I, Pelmus M, Aurias A, Pedeutour F, Mathoulin-Pelissier S, Coindre JM. Evaluation of MDM2 and CDK4 amplification by real-time PCR on paraffin wax-embedded material: a potential tool for the diagnosis of atypical lipomatous tumours/well-differentiated liposarcomas. J Pathol. 2004;202(1):95–102.
Binh MB, Sastre-Garau X, Guillou L, de Pinieux G, Terrier P, Lagace R, et al. MDM2 and CDK4 immunostainings are useful adjuncts in diagnosing well-differentiated and dedifferentiated liposarcoma subtypes: a comparative analysis of 559 soft tissue neoplasms with genetic data. Am J Surg Pathol. 2005;29(10):1340–7.
Stojanov IJ, Mariño-Enriquez A, Bahri N, Jo VY, Woo SB. Lipomas of the oral cavity: utility of MDM2 and CDK4 in avoiding overdiagnosis as atypical lipomatous tumor. Head Neck Pathol. 2019;13(2):169–76.
Weaver J, Downs-Kelly E, Goldblum JR, Turner S, Kulkarni S, Tubbs RR, et al. Fluorescence in situ hybridization for MDM2 gene amplification as a diagnostic tool in lipomatous neoplasms. Mod Pathol. 2008;21(8):943–9.
Panagopoulos I, Hoglund M, Mertens F, Mandahl N, Mitelman F, Aman P. Fusion of the EWS and CHOP genes in myxoid liposarcoma. Oncogene. 1996;12(3):489–94.
Dal Cin P, Sciot R, Panagopoulos I, Aman P, Samson I, Mandahl N, et al. Additional evidence of a variant translocation t(12;22) with EWS/CHOP fusion in myxoid liposarcoma: clinicopathological features. J Pathol. 1997;182(4):437–41.
Scapa JV, Cloutier JM, Raghavan SS, Peters-Schulze G, Varma S, Charville GW. DDIT3 immunohistochemistry is a useful tool for the diagnosis of myxoid liposarcoma. Am J Surg Pathol. 2021;45(2):230–9.
Baranov E, Black MA, Fletcher CDM, Charville GW, Hornick JL. Nuclear expression of DDIT3 distinguishes high-grade myxoid liposarcoma from other round cell sarcomas. Mod Pathol. 2021;34(7):1367–72.
Marino-Enriquez A, Fletcher CD, Dal Cin P, Hornick JL. Dedifferentiated liposarcoma with “homologous” lipoblastic (pleomorphic liposarcoma-like) differentiation: clinicopathologic and molecular analysis of a series suggesting revised diagnostic criteria. Am J Surg Pathol. 2010;34(8):1122–31.
Creytens D, van Gorp J, Savola S, Ferdinande L, Mentzel T, Libbrecht L. Atypical spindle cell lipoma: a clinicopathologic, immunohistochemical, and molecular study emphasizing its relationship to classical spindle cell lipoma. Virch Archiv. 2014;465(1):97–108.
Creytens D, Mentzel T, Ferdinande L, Lecoutere E, van Gorp J, Atanesyan L, et al. “Atypical” pleomorphic lipomatous tumor: a clinicopathologic, immunohistochemical and molecular study of 21 cases, emphasizing its relationship to atypical spindle cell lipomatous tumor and suggesting a morphologic spectrum (atypical spindle cell/pleomorphic lipomatous tumor). Am J Surg Pathol. 2017;41(11):1443–55.
Marino-Enriquez A, Nascimento AF, Ligon AH, Liang C, Fletcher CD. Atypical spindle cell lipomatous tumor: clinicopathologic characterization of 232 cases demonstrating a morphologic spectrum. Am J Surg Pathol. 2017;41(2):234–44.
Anderson WJ, Fletcher CDM, Jo VY. Atypical pleomorphic lipomatous tumor: expanding our current understanding in a clinicopathologic analysis of 64 cases. Am J Surg Pathol. 2021;45(9):1282–92.
Alaggio R, Coffin CM, Weiss SW, Bridge JA, Issakov J, Oliveira AM, et al. Liposarcomas in young patients: a study of 82 cases occurring in patients younger than 22 years of age. Am J Surg Pathol. 2009;33(5):645–58.
Creytens D, Folpe AL, Koelsche C, Mentzel T, Ferdinande L, van Gorp JM, et al. Myxoid pleomorphic liposarcoma-a clinicopathologic, immunohistochemical, molecular genetic and epigenetic study of 12 cases, suggesting a possible relationship with conventional pleomorphic liposarcoma. Mod Pathol. 2021;34(11):2043–9.
Hofvander J, Jo VY, Ghanei I, Gisselsson D, Mårtensson E, Mertens F. Comprehensive genetic analysis of a paediatric pleomorphic myxoid liposarcoma reveals near-haploidization and loss of the RB1 gene. Histopathology. 2016;69(1):141–7.
Carlson JW, Fletcher CD. Immunohistochemistry for beta-catenin in the differential diagnosis of spindle cell lesions: analysis of a series and review of the literature. Histopathology. 2007;51(4):509–14.
Miyaki M, Konishi M, Kikuchi-Yanoshita R, Enomoto M, Tanaka K, Takahashi H, et al. Coexistence of somatic and germ-line mutations of APC gene in desmoid tumors from patients with familial adenomatous polyposis. Cancer Res. 1993;53(21):5079–82.
Amary MF, Pauwels P, Meulemans E, Roemen GM, Islam L, Idowu B, et al. Detection of beta-catenin mutations in paraffin-embedded sporadic desmoid-type fibromatosis by mutation-specific restriction enzyme digestion (MSRED): an ancillary diagnostic tool. Am J Surg Pathol. 2007;31(9):1299–309.
Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91(10):1427–33.
Robinson DR, Wu YM, Kalyana-Sundaram S, Cao X, Lonigro RJ, Sung YS, et al. Identification of recurrent NAB2-STAT6 gene fusions in solitary fibrous tumor by integrative sequencing. Nat Genet. 2013;45(2):180–5.
Mohajeri A, Tayebwa J, Collin A, Nilsson J, Magnusson L, von Steyern FV, et al. Comprehensive genetic analysis identifies a pathognomonic NAB2/STAT6 fusion gene, nonrandom secondary genomic imbalances, and a characteristic gene expression profile in solitary fibrous tumor. Genes Chromosomes Cancer. 2013;52(10):873–86.
Doyle LA, Vivero M, Fletcher CD, Mertens F, Hornick JL. Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histologic mimics. Mod Pathol. 2014;27(3):390–5.
Bahrami A, Lee S, Schaefer IM, Boland JM, Patton KT, Pounds S, et al. TERT promoter mutations and prognosis in solitary fibrous tumor. Mod Pathol. 2016;29(12):1511–22.
Demicco EG, Wani K, Ingram D, Wagner M, Maki RG, Rizzo A, et al. TERT promoter mutations in solitary fibrous tumour. Histopathology. 2018;73(5):843–51.
Demicco EG, Wagner MJ, Maki RG, Gupta V, Iofin I, Lazar AJ, et al. Risk assessment in solitary fibrous tumors: validation and refinement of a risk stratification model. Mod Pathol. 2017;30(10):1433–42.
Salas S, Resseguier N, Blay JY, Le Cesne A, Italiano A, Chevreau C, et al. Prediction of local and metastatic recurrence in solitary fibrous tumor: construction of a risk calculator in a multicenter cohort from the French Sarcoma Group (FSG) database. Ann Oncol. 2017;28(8):1979–87.
Griffin CA, Hawkins AL, Dvorak C, Henkle C, Ellingham T, Perlman EJ. Recurrent involvement of 2p23 in inflammatory myofibroblastic tumors. Cancer Res. 1999;59(12):2776–80.
Kerr DA, Thompson LDR, Tafe LJ, Jo VY, Neyaz A, Divakar P, et al. Clinicopathologic and genomic characterization of inflammatory myofibroblastic tumors of the head and neck: highlighting a novel fusion and potential diagnostic pitfall. Am J Surg Pathol. 2021;45(12):1707–19.
Hutarew G, Hauser-Kronberger C, Strasser F, Llenos IC, Dietze O. Immunohistochemistry as a screening tool for ALK rearrangement in NSCLC: evaluation of five different ALK antibody clones and ALK FISH. Histopathology. 2014;65(3):398–407.
Hornick JL, Sholl LM, Dal Cin P, Childress MA, Lovly CM. Expression of ROS1 predicts ROS1 gene rearrangement in inflammatory myofibroblastic tumors. Mod Pathol. 2015;28(5):732–9.
Butrynski JE, D’Adamo DR, Hornick JL, Dal Cin P, Antonescu CR, Jhanwar SC, et al. Crizotinib in ALK-rearranged inflammatory myofibroblastic tumor. N Engl J Med. 2010;363(18):1727–33.
Schöffski P, Sufliarsky J, Gelderblom H, Blay JY, Strauss SJ, Stacchiotti S, et al. Crizotinib in patients with advanced, inoperable inflammatory myofibroblastic tumours with and without anaplastic lymphoma kinase gene alterations (European Organisation for Research and Treatment of Cancer 90101 CREATE): a multicentre, single-drug, prospective, non-randomised phase 2 trial. Lancet Respir Med. 2018;6(6):431–41.
Antonescu CR, Chen HW, Zhang L, Sung YS, Panicek D, Agaram NP, et al. ZFP36-FOSB fusion defines a subset of epithelioid hemangioma with atypical features. Genes Chromosomes Cancer. 2014;53(11):951–9.
Huang SC, Zhang L, Sung YS, Chen CL, Krausz T, Dickson BC, et al. Frequent FOS gene rearrangements in epithelioid hemangioma: a molecular study of 58 cases with morphologic reappraisal. Am J Surg Pathol. 2015;39(10):1313–21.
Hung YP, Fletcher CD, Hornick JL. FOSB is a useful diagnostic marker for pseudomyogenic hemangioendothelioma. Am J Surg Pathol. 2017;41(5):596–606.
Ortins-Pina A, Llamas-Velasco M, Turpin S, Soares-de-Almeida L, Filipe P, Kutzner H. FOSB immunoreactivity in endothelia of epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia). J Cutan Pathol. 2018;45(6):395–402.
Walther C, Tayebwa J, Lilljebjorn H, Magnusson L, Nilsson J, von Steyern FV, et al. A novel SERPINE1-FOSB fusion gene results in transcriptional up-regulation of FOSB in pseudomyogenic haemangioendothelioma. J Pathol. 2014;232(5):534–40.
Agaram NP, Zhang L, Cotzia P, Antonescu CR. Expanding the spectrum of genetic alterations in pseudomyogenic hemangioendothelioma with recurrent novel ACTB-FOSB gene fusions. Am J Surg Pathol. 2018;42(12):1653–61.
Hornick JL, Fletcher CD. Pseudomyogenic hemangioendothelioma: a distinctive, often multicentric tumor with indolent behavior. Am J Surg Pathol. 2011;35(2):190–201.
Errani C, Zhang L, Sung YS, Hajdu M, Singer S, Maki RG, et al. A novel WWTR1-CAMTA1 gene fusion is a consistent abnormality in epithelioid hemangioendothelioma of different anatomic sites. Genes Chromosomes Cancer. 2011;50(8):644–53.
Doyle LA, Fletcher CD, Hornick JL. Nuclear expression of CAMTA1 distinguishes epithelioid hemangioendothelioma from histologic mimics. Am J Surg Pathol. 2016;40(1):94–102.
Flucke U, Vogels RJ, de Saint Aubain Somerhausen N, Creytens DH, Riedl RG, van Gorp JM, et al. Epithelioid Hemangioendothelioma: clinicopathologic, immunhistochemical, and molecular genetic analysis of 39 cases. Diagn Pathol. 2014;9:131.
Antonescu CR, Le Loarer F, Mosquera JM, Sboner A, Zhang L, Chen CL, et al. Novel YAP1-TFE3 fusion defines a distinct subset of epithelioid hemangioendothelioma. Genes Chromosomes Cancer. 2013;52(8):775–84.
Anderson WJ, Fletcher CDM, Hornick JL. Loss of expression of YAP1 C-terminus as an ancillary marker for epithelioid hemangioendothelioma variant with YAP1-TFE3 fusion and other YAP1-related vascular neoplasms. Mod Pathol. 2021;34(11):2036–42.
Fanburg-Smith JC, Furlong MA, Childers EL. Oral and salivary gland angiosarcoma: a clinicopathologic study of 29 cases. Mod Pathol. 2003;16(3):263–71.
Nelson BL, Thompson LD. Sinonasal tract angiosarcoma: a clinicopathologic and immunophenotypic study of 10 cases with a review of the literature. Head Neck Pathol. 2007;1(1):1–12.
Antonescu CR, Yoshida A, Guo T, Chang NE, Zhang L, Agaram NP, et al. KDR activating mutations in human angiosarcomas are sensitive to specific kinase inhibitors. Cancer Res. 2009;69(18):7175–9.
Behjati S, Tarpey PS, Sheldon H, Martincorena I, Van Loo P, Gundem G, et al. Recurrent PTPRB and PLCG1 mutations in angiosarcoma. Nat Genet. 2014;46(4):376–9.
Painter CA, Jain E, Tomson BN, Dunphy M, Stoddard RE, Thomas BS, et al. The Angiosarcoma Project: enabling genomic and clinical discoveries in a rare cancer through patient-partnered research. Nat Med. 2020;26(2):181–7.
Agaimy A, Bieg M, Michal M, Geddert H, Märkl B, Seitz J, et al. Recurrent Somatic PDGFRB Mutations in Sporadic Infantile/Solitary Adult Myofibromas But Not in Angioleiomyomas and Myopericytomas. Am J Surg Pathol. 2017;41(2):195–203.
Hung YP, Fletcher CDM. Myopericytomatosis: clinicopathologic analysis of 11 cases with molecular identification of recurrent PDGFRB alterations in myopericytomatosis and myopericytoma. Am J Surg Pathol. 2017;41(8):1034–44.
Martignetti JA, Tian L, Li D, Ramirez MC, Camacho-Vanegas O, Camacho SC, et al. Mutations in PDGFRB cause autosomal-dominant infantile myofibromatosis. Am J Hum Genet. 2013;92(6):1001–7.
Antonescu CR, Sung YS, Zhang L, Agaram NP, Fletcher CD. Recurrent SRF-RELA fusions define a novel subset of cellular myofibroma/myopericytoma: a potential diagnostic pitfall with sarcomas with myogenic differentiation. Am J Surg Pathol. 2017;41(5):677–84.
Huang HY, Antonescu CR. Sinonasal smooth muscle cell tumors: a clinicopathologic and immunohistochemical analysis of 12 cases with emphasis on the low-grade end of the spectrum. Arch Pathol Lab Med. 2003;127(3):297–304.
Dias P, Chen B, Dilday B, Palmer H, Hosoi H, Singh S, et al. Strong immunostaining for myogenin in rhabdomyosarcoma is significantly associated with tumors of the alveolar subclass. Am J Pathol. 2000;156(2):399–408.
Sorensen PH, Lynch JC, Qualman SJ, Tirabosco R, Lim JF, Maurer HM, et al. PAX3-FKHR and PAX7-FKHR gene fusions are prognostic indicators in alveolar rhabdomyosarcoma: a report from the children’s oncology group. J Clin Oncol. 2002;20(11):2672–9.
Azorsa DO, Bode PK, Wachtel M, Cheuk ATC, Meltzer PS, Vokuhl C, et al. Immunohistochemical detection of PAX-FOXO1 fusion proteins in alveolar rhabdomyosarcoma using breakpoint specific monoclonal antibodies. Mod Pathol. 2021;34(4):748–57.
Bahrami A, Gown AM, Baird GS, Hicks MJ, Folpe AL. Aberrant expression of epithelial and neuroendocrine markers in alveolar rhabdomyosarcoma: a potentially serious diagnostic pitfall. Mod Pathol. 2008;21(7):795–806.
Thompson LDR, Jo VY, Agaimy A, Llombart-Bosch A, Morales GN, Machado I, et al. Sinonasal tract alveolar rhabdomyosarcoma in adults: a clinicopathologic and immunophenotypic study of fifty-two cases with emphasis on epithelial immunoreactivity. Head Neck Pathol. 2018;12(2):181–92.
Mosquera JM, Sboner A, Zhang L, Kitabayashi N, Chen CL, Sung YS, et al. Recurrent NCOA2 gene rearrangements in congenital/infantile spindle cell rhabdomyosarcoma. Genes Chromosomes Cancer. 2013;52(6):538–50.
Alaggio R, Zhang L, Sung YS, Huang SC, Chen CL, Bisogno G, et al. A molecular study of pediatric spindle and sclerosing rhabdomyosarcoma: identification of novel and recurrent VGLL2-related fusions in infantile cases. Am J Surg Pathol. 2016;40(2):224–35.
Agaram NP, Chen CL, Zhang L, LaQuaglia MP, Wexler L, Antonescu CR. Recurrent MYOD1 mutations in pediatric and adult sclerosing and spindle cell rhabdomyosarcomas: evidence for a common pathogenesis. Genes Chromosomes Cancer. 2014;53(9):779–87.
Szuhai K, de Jong D, Leung WY, Fletcher CD, Hogendoorn PC. Transactivating mutation of the MYOD1 gene is a frequent event in adult spindle cell rhabdomyosarcoma. J Pathol. 2014;232(3):300–7.
Rekhi B, Upadhyay P, Ramteke MP, Dutt A. MYOD1 (L122R) mutations are associated with spindle cell and sclerosing rhabdomyosarcomas with aggressive clinical outcomes. Mod Pathol. 2016;29(12):1532–40.
Tsai JW, ChangChien YC, Lee JC, Kao YC, Li WS, Liang CW, et al. The expanding morphological and genetic spectrum of MYOD1-mutant spindle cell/sclerosing rhabdomyosarcomas: a clinicopathological and molecular comparison of mutated and non-mutated cases. Histopathology. 2019;74(6):933–43.
Dashti NK, Wehrs RN, Thomas BC, Nair A, Davila J, Buckner JC, et al. Spindle cell rhabdomyosarcoma of bone with FUS-TFCP2 fusion: confirmation of a very recently described rhabdomyosarcoma subtype. Histopathology. 2018;73(3):514–20.
Agaram NP, Zhang L, Sung YS, Cavalcanti MS, Torrence D, Wexler L, et al. Expanding the spectrum of intraosseous rhabdomyosarcoma: correlation between 2 distinct gene fusions and phenotype. Am J Surg Pathol. 2019;43(5):695–702.
Amary F, Perez-Casanova L, Ye H, Cottone L, Strobl AC, Cool P, et al. Synovial chondromatosis and soft tissue chondroma: extraosseous cartilaginous tumor defined by FN1 gene rearrangement. Mod Pathol. 2019;32(12):1762–71.
Agaram NP, Zhang L, Dickson BC, Swanson D, Sung YS, Panicek DM, et al. A molecular study of synovial chondromatosis. Genes Chromosomes Cancer. 2020;59(3):144–51.
Pareja F, Brandes AH, Basili T, Selenica P, Geyer FC, Fan D, et al. Loss-of-function mutations in ATP6AP1 and ATP6AP2 in granular cell tumors. Nat Commun. 2018;9(1):3533.
França JA, Gayden T, Bareke E, Santos JN, de Sousa SF, Bastos-Rodrigues L, et al. Whole-exome sequencing reveals novel vacuolar ATPase genes’ variants and variants in genes involved in lysosomal biology and autophagosomal formation in oral granular cell tumors. J Oral Pathol Med. 2021;50(4):410–7.
Lee W, Teckie S, Wiesner T, Ran L, Prieto Granada CN, Lin M, et al. PRC2 is recurrently inactivated through EED or SUZ12 loss in malignant peripheral nerve sheath tumors. Nat Genet. 2014;46(11):1227–32.
Zhang M, Wang Y, Jones S, Sausen M, McMahon K, Sharma R, et al. Somatic mutations of SUZ12 in malignant peripheral nerve sheath tumors. Nat Genet. 2014;46(11):1170–2.
Prieto-Granada CN, Wiesner T, Messina JL, Jungbluth AA, Chi P, Antonescu CR. Loss of H3K27me3 expression is a highly sensitive marker for sporadic and radiation-induced MPNST. Am J Surg Pathol. 2016;40(4):479–89.
Schaefer IM, Fletcher CD, Hornick JL. Loss of H3K27 trimethylation distinguishes malignant peripheral nerve sheath tumors from histologic mimics. Mod Pathol. 2016;29(1):4–13.
Cleven AH, Sannaa GA, Briaire-de Bruijn I, Ingram DR, van de Rijn M, Rubin BP, et al. Loss of H3K27 tri-methylation is a diagnostic marker for malignant peripheral nerve sheath tumors and an indicator for an inferior survival. Mod Pathol. 2016;29(6):582–90.
Le Guellec S, Macagno N, Velasco V, Lamant L, Lae M, Filleron T, et al. Loss of H3K27 trimethylation is not suitable for distinguishing malignant peripheral nerve sheath tumor from melanoma: a study of 387 cases including mimicking lesions. Mod Pathol. 2017;30(12):1677–87.
Panse G, Mito JK, Ingram DR, Wani K, Khan S, Lazar AJ, et al. Radiation-associated sarcomas other than malignant peripheral nerve sheath tumours demonstrate loss of histone H3K27 trimethylation(†). Histopathology. 2021;78(2):321–6.
Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, et al. Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci U S A. 2001;98(11):6500–5.
Folpe AL, Fanburg-Smith JC, Billings SD, Bisceglia M, Bertoni F, Cho JY, et al. Most osteomalacia-associated mesenchymal tumors are a single histopathologic entity: an analysis of 32 cases and a comprehensive review of the literature. Am J Surg Pathol. 2004;28(1):1–30.
Bahrami A, Weiss SW, Montgomery E, Horvai AE, Jin L, Inwards CY, et al. RT-PCR analysis for FGF23 using paraffin sections in the diagnosis of phosphaturic mesenchymal tumors with and without known tumor induced osteomalacia. Am J Surg Pathol. 2009;33(9):1348–54.
Stratakis CA. Mutations of the gene encoding the protein kinase A type I-alpha regulatory subunit (PRKAR1A) in patients with the “complex of spotty skin pigmentation, myxomas, endocrine overactivity, and schwannomas” (Carney complex). Ann N Y Acad Sci. 2002;968:3–21.
Torres-Mora J, Dry S, Li X, Binder S, Amin M, Folpe AL. Malignant melanotic schwannian tumor: a clinicopathologic, immunohistochemical, and gene expression profiling study of 40 cases, with a proposal for the reclassification of “melanotic schwannoma.” Am J Surg Pathol. 2014;38(1):94–105.
Maleszewski JJ, Larsen BT, Kip NS, Castonguay MC, Edwards WD, Carney JA, et al. PRKAR1A in the development of cardiac myxoma: a study of 110 cases including isolated and syndromic tumors. Am J Surg Pathol. 2014;38(8):1079–87.
Hafeez F, Krakowski AC, Lian CG, Nazarian RM, Maleszewski JJ. Sporadic superficial angiomyxomas demonstrate loss of PRKAR1A expression. Histopathology. 2021. https://doi.org/10.1111/his.14568.
Panagopoulos I, Mertens F, Isaksson M, Domanski HA, Brosjo O, Heim S, et al. Molecular genetic characterization of the EWS/CHN and RBP56/CHN fusion genes in extraskeletal myxoid chondrosarcoma. Genes Chromosomes Cancer. 2002;35(4):340–52.
Yoshida A, Makise N, Wakai S, Kawai A, Hiraoka N. INSM1 expression and its diagnostic significance in extraskeletal myxoid chondrosarcoma. Mod Pathol. 2018;31(5):744–52.
Crew AJ, Clark J, Fisher C, Gill S, Grimer R, Chand A, et al. Fusion of SYT to two genes, SSX1 and SSX2, encoding proteins with homology to the Kruppel-associated box in human synovial sarcoma. EMBO J. 1995;14(10):2333–40.
Kosemehmetoglu K, Vrana JA, Folpe AL. TLE1 expression is not specific for synovial sarcoma: a whole section study of 163 soft tissue and bone neoplasms. Mod Pathol. 2009;22(7):872–8.
Terry J, Saito T, Subramanian S, Ruttan C, Antonescu CR, Goldblum JR, et al. TLE1 as a diagnostic immunohistochemical marker for synovial sarcoma emerging from gene expression profiling studies. Am J Surg Pathol. 2007;31(2):240–6.
Foo WC, Cruise MW, Wick MR, Hornick JL. Immunohistochemical staining for TLE1 distinguishes synovial sarcoma from histologic mimics. Am J Clin Pathol. 2011;135(6):839–44.
Zaborowski M, Vargas AC, Pulvers J, Clarkson A, de Guzman D, Sioson L, et al. When used together SS18-SSX fusion-specific and SSX C-terminus immunohistochemistry are highly specific and sensitive for the diagnosis of synovial sarcoma and can replace FISH or molecular testing in most cases. Histopathology. 2020;77(4):588–600.
Baranov E, McBride MJ, Bellizzi AM, Ligon AH, Fletcher CDM, Kadoch C, et al. A novel SS18-SSX fusion-specific antibody for the diagnosis of synovial sarcoma. Am J Surg Pathol. 2020;44(7):922–33.
Agaram NP, Zhang L, Sung YS, Singer S, Stevens T, Prieto-Granada CN, et al. GLI1-amplifications expand the spectrum of soft tissue neoplasms defined by GLI1 gene fusions. Mod Pathol. 2019;32(11):1617–26.
Xu B, Chang K, Folpe AL, Kao YC, Wey SL, Huang HY, et al. Head and neck mesenchymal neoplasms with GLI1 gene alterations: a pathologic entity with distinct histologic features and potential for distant metastasis. Am J Surg Pathol. 2020;44(6):729–37.
Dahlen A, Mertens F, Mandahl N, Panagopoulos I. Molecular genetic characterization of the genomic ACTB-GLI fusion in pericytoma with t(7;12). Biochem Biophys Res Commun. 2004;325(4):1318–23.
Antonescu CR, Agaram NP, Sung YS, Zhang L, Swanson D, Dickson BC. A distinct malignant epithelioid neoplasm with gli1 gene rearrangements, frequent S100 protein expression, and metastatic potential: expanding the spectrum of pathologic entities with ACTB/MALAT1/PTCH1-GLI1 fusions. Am J Surg Pathol. 2018;42(4):553–60.
Kerr DA, Pinto A, Subhawong TK, Wilky BA, Schlumbrecht MP, Antonescu CR, et al. Pericytoma with t(7;12) and ACTB-GLI1 fusion: reevaluation of an unusual entity and its relationship to the spectrum of GLI1 fusion-related neoplasms. Am J Surg Pathol. 2019;43(12):1682–92.
Delattre O, Zucman J, Melot T, Garau XS, Zucker JM, Lenoir GM, et al. The Ewing family of tumors–a subgroup of small-round-cell tumors defined by specific chimeric transcripts. N Engl J Med. 1994;331(5):294–9.
Yoshida A, Sekine S, Tsuta K, Fukayama M, Furuta K, Tsuda H. NKX2.2 is a useful immunohistochemical marker for Ewing sarcoma. Am J Surg Pathol. 2012;36(7):993–9.
Hung YP, Fletcher CD, Hornick JL. Evaluation of NKX2-2 expression in round cell sarcomas and other tumors with EWSR1 rearrangement: imperfect specificity for Ewing sarcoma. Mod Pathol. 2016;29(4):370–80.
Bishop JA, Alaggio R, Zhang L, Seethala RR, Antonescu CR. Adamantinoma-like Ewing family tumors of the head and neck: a pitfall in the differential diagnosis of basaloid and myoepithelial carcinomas. Am J Surg Pathol. 2015;39(9):1267–74.
Rooper LM, Jo VY, Antonescu CR, Nose V, Westra WH, Seethala RR, et al. Adamantinoma-like ewing sarcoma of the salivary glands: a newly recognized mimicker of basaloid salivary carcinomas. Am J Surg Pathol. 2019;43(2):187–94.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no relevant conflicts of interest.
Ethics Approval
Not applicable; the contents of this review do not involve patient data or private health information.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jo, V.Y., Demicco, E.G. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Soft Tissue Tumors. Head and Neck Pathol 16, 87–100 (2022). https://doi.org/10.1007/s12105-022-01425-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-022-01425-w