Abstract
Küttner tumor/chronic sclerosing sialadenitis is a fibroinflammatory process that characteristically involves the submandibular gland of patients with IgG4-related disease. Histologic examination is often important to make the diagnosis because of its nonspecific clinical and radiologic findings. Microscopically, Küttner tumor should be distinguished from other entities such as extranodal marginal zone lymphoma, Sjögren’s syndrome, and lymphoepithelial sialadenitis. The lesion is histologically well-demarcated with lobular architecture, extensive fibrosis, marked lymphoplasmacytic inflammation, formation of lymphoid follicles, acinar atrophy, and obliterative phlebitis, without the presence of lymphoepithelial lesions. The IgG4-to-IgG positive plasma cell ratio of >40 % is also an important feature to support the diagnosis of Küttner tumor. Moreover, flow cytometry is helpful to exclude a lymphoproliferative process. Clinicians and pathologists should consider the diagnosis of Küttner tumor in patients with elevated serum IgG4 level. Timely and accurate diagnosis is important for appropriate management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
History
A 61-year-old woman with a history of Immunoglobulin G4-(IgG4) related cholangitis and pancreatitis presented with a nontender right submandibular mass, which had been enlarging for 1 month. One year ago, she underwent excision of an enlarging left submandibular gland, which was diagnosed as Sjögren’s syndrome histologically at another hospital. The patient reported that her recent symptoms started when she stopped taking prednisone that had been prescribed for IgG4-related disease. Physical examination revealed indurated, nontender, and mobile right submandibular gland which measured 2.0 cm in diameter. Her serum IgG4 level had been elevated in the past (167.6 mg/dL; reference range: 4.0–86.0 mg/dL) and the level had recently decreased after prednisone therapy (13.7 mg/dL).
Radiology
Computed tomography of the neck with contrast (Fig. 1) showed slight enlargement of the right submandibular gland with subtle adjacent fat stranding without focal mass lesions. The left submandibular gland was absent. The muscles and deep spaces of the neck appeared normal, and no lymphadenopathy was identified. The radiologic findings are suggestive of sialadenitis.
Diagnosis
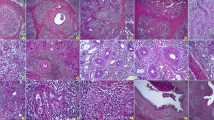
An excisional biopsy was performed to confirm the diagnosis. Gross examination revealed a 3.4 × 2.4 × 1.5 cm right submandibular gland with tan-pink, glistening, and nodular cut surface. The histologic evaluation of the right submandibular gland showed preservation of lobular architecture with prominent interlobular fibrosis (Fig. 2a). Intense lymphoplasmacytic infiltrates were seen in between salivary glands (Fig. 2b). IgG and IgG4 immunostains highlighted the plasma cells and delineated an IgG4/IgG ratio greater than 40 % (Fig. 2c, d). There was no evidence for involvement of the salivary gland by a lymphoproliferative neoplasm, which was confirmed by flow cytometry. The histologic findings and immunohistochemical profile are consistent with the diagnosis of Küttner tumor.
a Low power view of the submandibular gland shows interlobular fibrosis and lymphoplasmacytic infiltrates, Hematoxylin-eosin, original magnification ×4. b Lymphoplasmacytic infiltrates are seen in the lobules, without evidence of lymphoepithelial lesions. Hematoxylin-eosin, original magnification ×10. c–d IgG4-to-IgG positive plasma cell ratio in the lymphoplasmacytic infiltrate is greater than 40 %. c Immunoglobulin G, original magnification ×20. d Immunoglobulin G4, original magnification ×20
Discussion
IgG4-related disease is a fibroinflammatory condition which has been described in many organ systems. The process is characterized by lesions with dense lymphoplasmacytic infiltrates rich in IgG4-positive plasma cells, storiform fibrosis, and elevated serum IgG4 levels [1]. Küttner tumor, also known as chronic sclerosing sialadenitis, was originally described by Küttner [2] who reported a patient with “hard swelling” of submandibular glands. It is a relatively uncommon lesion that is considered to be a part of IgG4-related diseases on the basis of its histologic characteristics and elevated serum IgG4 level [3, 4].
Küttner tumor usually presents in middle-aged patients with a slight male predominance and submandibular gland predilection. Because of the nonspecific clinical findings, serologic testing and histologic examinations are necessary to exclude other diagnoses. Histologic findings of Küttner tumor include a well-defined lesion with lobular architecture preservation, interlobular fibrosis, marked lymphoplasmacytic inflammation, formation of lymphoid follicles, acinar atrophy, obliterative phlebitis, and the absence of lymphoepithelial lesions [4]. The IgG4-to-IgG positive plasma cell ratio of >40 % in lesions with dense lymphoplasmacytic infiltrates is a useful method for establishing the diagnosis of IgG4-related disease [5].
The most important entities in the differential diagnosis of Küttner tumor are extranodal marginal zone lymphoma (MALT) and other inflammatory processes such as Sjögren’s syndrome and lymphoepithelial sialadenitis. Major salivary gland neoplasms predominantly arise in the parotid glands (80 %), while submandibular gland involvement is only seen in 10–15 % of the cases. The most frequent benign and malignant tumors of the submandibular gland are pleomorphic adenoma and adenoid cystic carcinoma, respectively [6]. The diagnosis of these tumors are rarely problematic because of their distinctive morphologic findings.
The clinical manifestations of Sjögren’s syndrome include persistent dry eyes and/or mouth and parotid gland enlargement. Isolated involvement of submandibular glands would be unusual for Sjögren’s syndrome. Positive serologic testing for anti-Ro/SSA (anti-Sjögren’s-syndrome-related antigen A) and/or anti-La/SSB (anti-Sjögren’s-syndrome-related antigen B) antibodies, the combination of high anti-nuclear antibody (ANA) titer with positive rheumatoid factor, or the presence of a centromere staining of ANA on immunofluorescence also support the diagnosis. Minor salivary gland biopsies demonstrate periductal lymphoplasmacytic inflammation without interlobular fibrosis, or lymphoid follicular hyperplasia.
Lymphoepithelial sialadenitis, occasionally associated with Sjögren’s syndrome, is histologically characterized by numerous lymphoepithelial lesions which consist of ductal epithelial cell proliferation with the formation of lymphoepithelial islands and cystic dilatation of peripheral ducts. Interlobular fibrosis and elevated number of IgG4 positive plasma cells are usually absent.
Most salivary gland MALT lymphomas develop on the basis of chronic antigen stimulation associated with Sjögren’s syndrome and lymphoepithelial sialadenitis. Rarely, they have been reported to arise from Küttner tumor [7]. MALT lymphoma is marked by a proliferation of neoplastic marginal zone B cells, with scattered large, transformed lymphoid cells, reactive germinal centers, and lymphoepithelial lesions. Increased plasma cells may also be seen in MALT lymphoma with plasmacytic differentiation. The demonstration of monoclonality either by immunohistochemistry or flow cytometry and recurrent chromosomal abnormalities (t(11;18) (API2-MALT1), t(14;18) (IGH-MALT1), t(1;14) (IGH-BCL10)) are helpful to make the diagnosis [8].
Corticosteroids are the first line treatment for patients with IgG4-related disease, with most patients responding promptly to an initial high dose of prednisone (30–40 mg daily) which is tapered over 3–6 months. Patients with refractory or recurrent disease may benefit from second line immunosuppressive agents, which include azathioprine, mycophenolate, and rituximab [9]. In conclusion, Küttner tumor should be considered in patients with a history of IgG4-related disease. Histologic diagnosis is important to exclude other inflammatory processes and malignancies. Early diagnosis is beneficial to detect other disease manifestations and to prevent irreversible organ dysfunction.
References
Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539–51.
Kuttner H. Uber entzundiche tumoren der submaaxillar-.speichel-druse. Bruns Beitr Klin Chir. 1986;15:815–34.
Kitagawa S, Zen Y, Harada K, et al. Abundant IgG4-positive plasma cell infiltration characterizes chronic sclerosing sialadenitis (Küttner tumor). Am J Surg Pathol. 2005;29:783–91.
Geyer JT, Ferry JA, Harris NL, et al. Chronic sclerosing sialadenitis (Küttner tumor) is an IgG4-associated disease. Am J Surg Pathol. 2010;34:202–10.
Deshpande V, Zen Y, Chan JKC, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25:1181–92.
Rapidis AD, Stavrianos S, Lagogiannis G, Faratzis G. Tumor of the submandibular gland: clinicopathologic analysis of 23 patients. J Oral Maxillofac Surg. 2004;62:1203–8.
Ochoa ER, Harris NL, Pilch BZ. Marginal zone B-cell lymphoma of the salivary gland arising in chronic sclerosing sialadenitis (Küttner tumor). Am J Surg Pathol. 2001;25:1546–50.
Ihrler S, Baretton GB, Menauer F, et al. Sjogren’s syndrome and MALT lymphomas of salivary glands: a DNA-cytometric and interphase-cytogenetic study. Mod Pathol. 2000;13:4–12.
Culver EL, Hunt A, Crewe E, et al. Immunoglobulin G4 related chronic sclerosing sialadenitis. J Laryngol Otol. 2015;129:226–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Putra, J., Ornstein, D.L. Küttner Tumor: IgG4-Related Disease of the Submandibular Gland. Head and Neck Pathol 10, 530–532 (2016). https://doi.org/10.1007/s12105-016-0729-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-016-0729-2