Abstract
Malakoplakia is a rare inflammatory condition that typically occurs in the urinary tract. The cutaneous form is less prevalent, and most commonly occurs in the perianal or genital regions. Here we present a 61 year old lady with cutaneous malakoplakia of the neck, which was successfully treated with surgical excision and a prolonged course of ciprofloxacin. We follow our case report with a discussion and literature review of all seventeen previously reported cutaneous head and neck malakoplakia cases from the literature. A diagnosis of cutaneous malakoplakia should be considered in nodular, ulcerated or discharging lesions that are refractory to treatment. Histology is essential, not only to diagnose malakoplakia, but also to exclude other important differential diagnoses, such as malignancy. Combined surgical excision and prolonged antibiotic courses appear to have the highest success rate. Antibiotics should be culture specific, but quinolones appear to be the best empirical choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malakoplakia is a rare inflammatory condition that typically occurs in the urinary tract. Cutaneous malakoplakia is a less common presentation of the disease, which most commonly occurs in the perianal or genital regions.
Here we present a case of cutaneous malakoplakia in the head and neck region followed by a discussion and literature review of all 17 previously reported cutaneous head and neck malakoplakia cases known to the authors. We will discuss pre-disposing factors, differential diagnoses, diagnostic features and treatment.
The Case
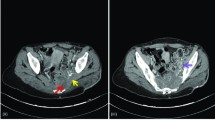
A 61 year old lady, with a background of type 2 diabetes mellitus and chronic obstructive pulmonary disease, was referred to the Otolaryngology department from her General Practitioner (family medicine practitioner) with a 4 week history of a right sided inferior neck mass. She had a mild feeling of general malaise and examination of the mass was consistent with a level 5 neck abscess, with corresponding level 2 and 5 lymphadenopathy. The remainder of head and neck examination, including flexible nasendoscopy, was unremarkable. Aspiration of the lump was attempted on first presentation to ENT, but was unsuccessful in yielding any fluid. Blood tests showed both white cell count and C-reactive protein to be within normal ranges at first presentation. She was treated with Co-amoxiclav, which initially gave a mild improvement in her symptoms, but the lump never completely resolved and her symptoms recurred rapidly after stopping the antibiotics. Several further prolonged courses of antibiotics were used, with similar results. After several months, the wound began to discharge purulent material and some granulation tissue was apparent around the wound site (Fig. 1). Multiple swabs of the wound and discharge were taken for culture, but none grew any organism. Tuberculosis was queried, but Ziehl-Neelsen staining and prolonged culture for Mycobacteria were negative. Initial core biopsy samples were reported as showing chronic inflammatory tissue. A contrast enhanced CT scan of the neck (Fig. 2) showed appearances consistent with an inflammatory mass encircling the right sternocleidomastoid muscle with a central fluid component and overlying skin thickening.
Given a lack of improvement with further courses of antibiotics, a further core biopsy was performed under general anaesthetic. Histology of this sample (Fig. 3) showed Michaelis–Gutmann bodies and malakoplakia was diagnosed. A modified lateral neck dissection as performed in which all sinuses and areas of affected skin were resected, in addition to the majority of the right sternocleidomastoid muscle. The area was then reconstructed with an anterolateral thigh free flap.
The patient responded well to surgery and a further three month course of ciprofloxacin. At her three month post operative follow up appointment she was disease free.
Review of Literature
A Medline (1946-present) search using the mapped term ‘Malacoplakia’ was undertaken, in addition to title and abstract searches for the stems ‘malakoplak*’ and ‘malacoplak*’. Searches were limited to humans. The titles of the 898 results were screened and articles were excluded if pertaining exclusively to malakoplakia in anatomical areas discrete from the head and neck. All 187 remaining titles and available abstracts were then reviewed and all cases of malakoplakia with cutaneous involvement in the head and neck region were included. Results were checked against previous literature reviews (Afonso et al. [18], Kohl and Hans [19] and Remond et al. [20]). This search located a total of 17 reported cases of cutaneous malakoplakia of the head and neck in the literature (Table 1). All ages are affected in the cases noted, ranging from 9 months to 83 years old. 59 % cases were over the age of 50 and 65 % cases were male. 59 % of papers reported factors leading to local or systemic immunosuppression. Where positive culture results were reported, the most common was E.coli (35 %), although the same number of cases had showed no growth or did not report microbiology results. The majority of lesions presented as a variation on a mass-nodule, which could grow rapidly, ulcerate or discharge. As a result, the most common differential diagnoses were malignancy (35 %) and an acute infective process (18 %). Table 2 shows rates of antibiotic and surgical treatments used in reviewed cases. 7 cases reported the duration antibiotics used, with a mean duration of treatment amongst these cases of 105 days (range 10–300 days). 6 cases reported using antibiotics, but did not record the duration of antibiotic treatment. In those 5 cases that prescribed a prolonged course of antibiotics (>30 days) in combination with surgery, resolution was achieved in 100 % cases, with a mean duration of antibiotic treatment in this group of 121 days. This figure was also achieved where surgical excision was used alone, but only in cases where the malakoplakia lesion was small, and in one case only after multiple excisions. This compares with a 50 % resolution rate when antibiotics were used alone.
Many cases used combinations of antibiotics, of which quinolones (N = 5), cephalosporins (N = 4), co-trimoxazole (N = 3) and penicillins (N = 3) were the most common. Cases in which a quinolones or penicillin was used as part of the antibiotic regime, in combination with surgical treatment, resolution was achieved in 100 % of cases. The last case successfully using a penicillin was in 1998, compared with 2006 for a quinolone. Debridement and antibiotics achieved resolution in 75 % cases, whereas excision and antibiotics achieved resolution in 86 % cases; In the 2 cases where total resolution was not achieved, the duration of antibiotic treatment was not recorded.
Discussion
Malakoplakia is a rare non-malignant inflammatory condition which most commonly presents in the urinary tract. It is much more common in adults than children [21]. Cutaneous malakoplakia is most commonly seen in older males, and is most commonly found in the perineal area [2]. Its rarity and non-specific appearance make it a challenging diagnosis which can only be made histologically by identifiying its characteristic Michaelis–Gutmann (MG) bodies, first described in 1902 as foamy macorphages containing targetoid intracytoplasmic inclusion bodies [22]. These Michaelis–Gutmann bodies stain positively with periodic acid Schiff, Perl’s (iron) and Von Kossa (calcium) stains.
Clinically the appearance of malakoplakia can be varied, and differential diagnoses commonly include tuberculosis, non-tuberculous bacterial infection, parasites such as Taenia spp. and malignancy. It is not known why malakoplakia occurs, but many factors have been implicated, including opportunistic bacterial infection by gram negative bacilli, such as E. coli, in the immunocompromised host [23]. It has been postulated that the lesion occurs as a result of macrophages being unable to completely destroy bacteria that they have phagocytosed [24]. The result of this is the pathognomonic Michaelis–Gutmann bodies. Further, it is thought that the particular bacterial species implicated may act on cyclic GMP production in the macrophages in order to impair their action [25]. Immunosuppression, whether generalised or localised, is commonly implicated [3]. Cases of malakoplakia, including many in this literature review, have been reported in sites of surgical wounds and irradiated cancerous tissue, as well as development in patients with HIV, diabetes mellitus, underlying malignancy, sarcoidosis and those on long term immunomodulating medication, including steroids. The likely immunosuppressive factor in our patient is her underlying type II diabetes mellitus, although her long smoking history may also be contributory.
A number of treatments have been used successfully in case reports from the literature, including surgical excision, antibiotic therapy and bethanechol chloride [8] which theoretically acts to increase cGMP levels. Combinations of antibiotics involving co-trimoxazole or ciprofloxacin are commonly used, due to their good intracellular penetration within macrophages [26]. However, in our literature review, only one case successfully used antibiotics alone to bring about resolution.
The most common and successful approach from appears to be the use of prolonged courses of antibiotics combined with surgical excision. This combined approach was required to bring about a successful outcome in our case. Excision was more effective than debridement, and was successfully used alone in many small lesions. Although quinolones and ampicillin were used with equal success rates, ampicillin had not been used in any cases within the last 15 years, which may reflect the development of widespread resistance of E.coli to this antibiotic.
Conclusion
Cutaneous malakoplakia is a rare diagnosis in the head and neck, but should be considered in cases of nodular, ulcerated or discharging lesions that are refractory to treatment. Histology is essential, not only to diagnose malakoplakia, but also to exclude other important differential diagnoses, such as malignancy. Combined surgical excision and prolonged antibiotic courses appear to have the highest success rate. Antibiotics should be culture specific, but combinations involving a quinolone are good empirical choices before culture results become available.
References
Rubinson R, Mendes VS, Sanchez G, Costantini S. Malakoplakia. Pediatr Dermatol. 2012;29(4):541–3.
Garg M, Eley KA, Bond SE, Shah KA, Browning L, Watt-Smith SR. Malakoplakia presenting as an enlarging neck mass: case presentation and review of the literature. Head Neck. 2010;32(9):1269–72.
Coombes DM, Norris PM, Barrett AW, Brown AE. Malakoplakia of the face: a rare but important diagnosis. Br J Oral Maxillofac Surg. 2010;48(1):55–7.
Akkuzu G, Aydin E, Bilezikçi B, Akkuzu B, Ozluoglu LN. Malakoplakia in nasal vestibule. Otolaryngol Head Neck Surg. 2006;135(4):636–7.
Toubes-Klingler E, Prabhu VC, Bernal K, Poage D, Swindells S. Malacoplakia of the cranium and cerebrum in a human immunodeficiency virus-infected man: case report. J Neurosurg. 2006;104(3):432–5.
Kumar Vinod, Coady MSE. Malakoplakia of the neck in an immunosuppressed patient. Plast Reconstr Surg. 2005;116(6):125e–7e.
Pang LC. Malacoplakia manifesting as a chronic inflammatorymass at the site of a nonhealing surgical wound. Ear Nose Throat J. 2003;82:876–80.
Schmerber S, Lantuejoul S, Lavieille JP, Reyt E. Malakoplakia of the neck. Arch Otolaryngol Head Neck Surgery. 2003;129(11):1240–2.
Enjolras O, Guillemette J, Carlotti A, Plantier F, Jubert C, Escande JP. Cutaneous malacoplakia: a pediatric case. Annales de dermatologie et de venereologie. 1998;125(8):522–4.
Feldmann R, Breier F, Duschet P, Löw-Weiser H, Gschnait F. Cutaneous malakoplakia on the forehead. Dermatology. 1997;194(4):358–60.
Douglas-Jones AG, Rodd C, James EMV, Mills RGS. Prediagnostic malakoplakia presenting as a chronic inflammatory mass in the soft tissues of the neck. J Laryngol Otol. 1992;106(02):173–7.
Nayar RC, Garg I, Alapatt JJ. Malakoplakia of the temporal bone in a nine-month-old infant. J Laryngol Otol. 1991;105(07):568–70.
Lowitt MH, et al. Cutaneous malacoplakia: a report of two cases and review of the literature. J Am Acad Dermatol. 1996;34(2):325–32.
Kumar PV, Tabei SZ. Cutaneous malakoplakia diagnosed by scraping cytology. Acta Cytol. 1988;32:125–7.
Font Ramon L, Bersani Thomas A, Eagle Ralph C. Malakoplakia of the eyelid: clinical, histopathologic, and ultrastructural characteristics. Ophthalmology. 1988;95(1):61–8.
Addison DJ. Malakoplakia of the eyelid. Ophthalmology. 1986;93(8):1064–7.
Chaudhry AP, Satchidanand SK, Anthone R, Baumler RA, Gaeta JF. An unusual case of supraclavicular and colonic malakoplakia—a light and ultrastructural study. J Pathol. 1980;131(3):193–208.
Afonso JPJM, Ando PN, Padilha MHVDQ, Michalany NS, Porro AM. Cutaneous malakoplakia: case report and review. Anais brasileiros de dermatologia. 2013;88(3):432–7.
Kohl Shane K, Hans Christine P. Cutaneous malakoplakia. Arch Pathol Lab Med. 2008;132(1):113.
Remond B, Dompmartin A, Moreau A, Esnault P, Thomas A, Mandard JC, Leroy D. Cutaneous malacoplakia. Int J Dermatol. 1994;33(8):538–42.
McClure John. Malakoplakia. J Pathol. 1983;140(4):275–330.
Michaelis L, Gutmann C. ÜberEinschlüsse in blasentumoren. Z Klin Med. 1902;47:208–15.
Stanton MJ, Maxted W. Malacoplakia: a study of the literature and current concepts of pathogenesis, diagnosis and treatment. J urolo. 1981;125(2):139.
Lou TY, Teplitz C. Malakoplakia: pathogenesis and ultrastructural morphogenesis: a problem of altered macrophage (phagolysosomal) response. Hum Pathol. 1974;5:191–207.
Abdou NI, NaPombejara C, Sagawa A, Ragland C, Stechschulte DJ, Nilsson U, Sooley B. Malakoplakia: evidence for monocyte lysosomal abnormality correctable by cholinergic agonist in vitro and in vivo. N Engl J Med. 1977;297(26):1413–9.
van der Voort PH, ten Velden JJ, Wassenaar RP, Silberbusch J. Malacoplakia: two case reports and a comparison of treatment modalities based on a literature review. Arch Intern Med. 1996;156(5):577–83.
Acknowledgments
Mr. Martin Heaton, Consultant Plastic Surgeon at the Norfolk and Norwich University Hospital UK, for all his help with this patient’s surgical reconstructive work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Rights and permissions
About this article
Cite this article
Coates, M., Del Pero, M.M. & Nassif, R. A Case of Cutaneous Malakoplakia in the Head and Neck Region and Review of the Literature. Head and Neck Pathol 10, 444–450 (2016). https://doi.org/10.1007/s12105-016-0721-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-016-0721-x