Abstract
Objectives
To estimate the proportion of neonates getting readmitted to neonatal intensive care unit (NICU), after discharge from the hospital. Secondary objectives were to describe the clinical characteristics, reason for readmission and outcome of neonates getting readmitted.
Methods
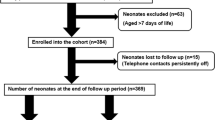
A retrospective descriptive study was conducted to identify neonates getting readmitted to NICU within 28 d of birth and/or before 40 wk post-menstrual age (PMA). Details of neonates who were readmitted to NICU were identified and data extracted in predesigned proforma from digitalized case records (July 2021-June 2023), and outcomes were analyzed.
Results
Out of 26,403 live-births, 5175 neonates required NICU admission (19.6%). Readmissions accounted for 5.9% (95% CI: 5.3–6.6%) of NICU admissions (305/5175) and 1.2% (95% CI: 1.0–1.3%) of live-births. Mean gestational age and birthweight were 36.8 (2.9) wk (range 25–41) and 2584 (713) g (range = 650–4900). Ninety-six (31.5%) were preterm. One hundred and three (33.8%) were high risk neonates. Median age at readmission was 17 d (range: 3–150). Infections (n = 109, 35.7%), infection-related complications (n = 18, 5.9%), feeding problems (n = 63, 20.6%), and jaundice (n = 42, 13.7%) were commonest reasons for readmission. Median duration of hospital stay was 5 d (range: 1–120). Two hundred and ninety four (96.4%) were discharged, and 10 (3.2%) neonates expired.
Conclusions
Readmissions accounted for 5.9% of total NICU admissions. Infections, jaundice and feeding related issues accounted for 76% of all the readmissions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neonates comprise a fragile population who are at risk for a lot of unique problems ranging from hypothermia, hypoglycemia, infection, complications related to prematurity and death. Though 88.6% of the deliveries in India are institutional, follow-up after discharge from hospital is not done routinely [1]. Both high-risk and normal neonates need ongoing follow-up to address concerns and to ensure well-being, failing which they are likely to return to the hospital with complications like jaundice, infection or other morbidities [2, 3]. Studying the clinical characteristics of neonates who are getting readmitted after hospital discharge will help us identify the problems that need to be addressed before discharge. Though there are recent studies emphasizing the need for comprehensive post-discharge care for high-risk preterm infants [4,5,6], there is lack of data on the burden of readmissions in otherwise well, term neonates, in the Indian setting [7], which is why the authors intended to capture the overall profile of readmissions in both these groups, to look for risk factors associated with readmissions.
Material and Methods
The study was conducted as a retrospective descriptive study, in the department of Neonatology, in a tertiary health care centre from Southern India. The study protocol was approved by the Institute Ethics Committee (JIP/IEC-OS/334/2023). Data was collected for a period of 2 y (July 2021-June 2023). The primary objective was to estimate the proportion of neonates requiring readmission to neonatal intensive care unit (NICU), after discharge from hospital. Secondary objectives were to describe the clinical characteristics, reason for readmission and outcome of neonates getting readmitted. Both high-risk (discharged from NICU) and well neonates (discharged from postnatal ward) were included. All neonates who required admission within 28 d of birth (in case of term neonates) and/or before 40 wk of post-menstrual age (PMA) (in preterm neonates) were included, as this was the NICU policy for readmissions. Neonates were discharged from postnatal ward once feeding was established, urine and meconium was voided and there was no excessive weight loss. Point of care capillary bilirubin measurements were done if there was significant jaundice on clinical examination, as the authors did not have a transcutaneous bilirubinometer. Pulse oximetry screening was not being done prior to discharge routinely during the study period. High risk neonates were discharged once the following were achieved: 34 wk post-menstrual age, regained birthweight and/or reached 1500 g, gaining weight for consecutive days, completion of immunization and mother was confident in feeding, thermal regulation, kangaroo mother care (KMC) and administering medications, caffeine stopped and apnea free for at least 5 d off caffeine. If the infant required caffeine in the 5 d period, it was restarted, and based on the infant’s stability and parental preference, the infant was discharged and caffeine was stopped after admission at 40 wk PMA.
Data was obtained from NICU excel data sheet and individual digitalized case records were obtained from the medical records section. Consecutive sampling was done. Baseline variables collected were: gestational age (GA), sex, mode of delivery, birthweight, appropriate/small/large for gestational age (AGA/SGA/LGA) status, risk category (high risk/normal), mode of feeding, maternal age, details of previous NICU admission (if any). Data collected on clinical characteristics at readmission included: day of life at readmission, symptoms admitted for, final diagnosis, duration of hospital stay, treatment (need for oxygen/ respiratory support, parenteral nutrition, phototherapy, antibiotics), associated morbidities (shock, culture proven and culture negative sepsis, meningitis) and outcomes (discharge/death). Based on the symptomatology, course during hospital stay and the primary reason requiring admission, final diagnosis was assigned, considering the fact that multiple medical conditions could co-exist in the same infant. Final diagnosis was grouped under one of the 16 broad categories. Antibiotics were initiated in case sepsis was suspected after taking appropriate cultures. Infants who had clinical symptoms of infection with a negative culture and required antibiotics for 5 d or more were classified as culture negative sepsis. Those with positive blood or CSF cultures were labelled as culture proven sepsis. Neonates with excessive weight loss/poor weight gain and/or dehydration in whom other causes were ruled out and there was adequate weight gain after optimization of breastfeeding were labelled as having feeding issues.
For an estimated prevalence of readmissions as 5% (among total NICU admissions; based on unit data) with 1% absolute precision and 95% level of significance, and accounting for missing data (10%), the authors had to screen 2090 admissions. As it was a retrospective study, the authors decided to look at 2 y data, where there were 5175 NICU admissions, which meant the present study was powered to detect the estimated prevalence. Cases with missing/incomplete data were excluded. If the final diagnosis was in doubt, it was cross-checked from the original case-records. Descriptive statistics were depicted as mean (standard deviation/SD) or median (Interquartile range/IQR). Frequencies were represented as percentages. Pre-specified analysis was planned for comparison of readmission diagnosis between term and preterm infants and was done by student t-test/ Mann-Whitney U test, for continuous variables and by Pearson chi-square/ Fisher exact test for categorical variables. To adjust for confounders, the authors intended to use binary multiple logistic regression analysis to identify factors associated with increased rate of NICU admissions in any of the sub-groups (high-risk vs. well baby/ term vs. preterm).
Results
During the study period, there were 26,403 live-births, of which 5175 neonates required NICU admission (19.6%). Readmissions to NICU (n = 305) accounted for 5.9% (95% CI: 5.3–6.6%) of total NICU admissions and 1.2% (95% CI: 1.0-1.3%) of total live-births. The baseline characteristics of admitted neonates are listed in Table 1. Majority of the readmissions were term neonates and two-thirds of the neonates (n = 202) were well neonates, who were earlier discharged from postnatal ward, while the rest comprised of high-risk neonates who were discharged from the NICU. One-third of the population was SGA and exclusive breastfeeding rate in the neonates who got readmitted was 82.3%. Mean gestational age of neonates who got readmitted was 36.8 (2.9) wk, ranging from 25 to 41 wk, with an average birthweight of 2584 (713) g. Out of the readmissions, 31.5% were preterm infants (Table 1).
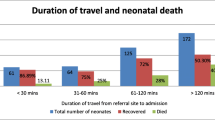
Overall, the commonest reasons for readmissions included: infection and infection associated complications (42.6%), complications due to feeding related issues (19.7%) and jaundice (13.7%), all of which accounted for 76% of all readmissions (Tables 2 and 3). The rest were due to failure to thrive (3.9%), heart disease (3.6%; n = 11: ventricular septal defect – 4, tricuspid atresia – 1, truncus arteriosus – 1, coarctation of aorta – 1, total anomalous pulmonary venous connection – 1, double outlet right ventricle – 1, myocarditis – 2), social reasons (3.3%), hematological (3.3%; n = 10: anemia – 9, Thrombocytopenia – 1), central nervous system/CNS (2%; n = 6: benign sleep myoclonus – 4, neonatal seizures – 2), surgical (1.3%; n = 5: Hirschsprung disease – 1, gastroesophageal reflux disease/GERD – 1, malrotation – 2, tracheoesophageal fistula – 1), Endocrine (1.3%; n = 4: hypothyroidism – 3, metabolic bone disease – 1), medical optimization (1.3%; n = 4: hyperinsulinemic hypoglycemia – 2, caffeine stoppage – 2), metabolic (urea cycle disorder – 1), Retinopathy of prematurity/ROP (0.98%; n = 3), miscellaneous (paracetamol toxicity – 1, swallowed maternal blood – 1, physiological breast enlargement – 1, umbilical granuloma – 1, ranula – 1). Pre-specified subgroup analyses were done for term vs. preterm infants with respect to the etiologies for readmission, which revealed that admissions for feeding problems were significantly higher among term infants (unadjusted odds ratio/OR: 11.63 [3.6-59.36], p < 0.01). After adjusting for SGA status, mode of delivery, low birthweight, early discharge (< 48 h), the association still remained significant (adjusted OR: 7.27 [2.24–23.59], p < 0.01). Among neonates admitted with complications related to feeding problems (n = 60, 19.7%), 85% were admitted for excessive weight loss (n = 38) and hypernatremic dehydration (n = 13).
Among the infections, culture proven sepsis accounted for 41.1% (blood = 38, urine = 8 ). Staph aureus, Escherichia coli, and Elizabethkingia anophelis accounted for 67.4% of all the isolates (Table 3). Seventeen had meningitis and 2 had septic arthritis. Among 66 culture negative infections, culture negative sepsis (n = 24, 36.4%), viral and bacterial pneumonia (n = 13, 19.7%) and viral infections (n = 17, 25.8%) accounted for a little above 80% of all the culture negative infections, followed by scrub typhus (n = 5, 7.6%).
Readmission was also associated with significant morbidities (Table 1). Antibiotics were used in 51.8% neonates, and 9 neonates underwent surgery (3.0%). These included cardiac surgeries, abdominal surgeries, arthrotomy and ventriculoperitoneal shunt surgery. Median duration of hospital stay was 5 d (range 1-120). Two hundred and ninety four (96.4%) were discharged, 1 (0.3%) was discharged against medical advice and 10 (3.2%) neonates expired.
Discussion
In the present study, the authors intended to identify the clinical profile and outcomes of both high-risk (discharged from NICU) and well neonates (discharged from postnatal ward), requiring early readmission, for a period of two years. In a systematic review of 28 studies evaluating risk factors for readmissions in the first month after discharge, the prevalence of readmissions ranged from 0.2 to 19.4% in different studies [8]. In the present study the proportion was 1.2%, though this might be an underrepresentation as it was a single hospital-based retrospective study. Majority (66.2%) neonates had an initial uneventful postnatal course. Most common causes of readmission were infections and associated complications (42.6%), followed by feeding related problems (20.6%) and jaundice (13.7%). The results are similar to other Indian studies [4,5,6]. Kumar et al. reported that at least 66% required readmissions for infections, whereas 47% required readmissions for infections in another centre in Northern India [4]. Mortality rates in rehospitalization was 3.2% in the present study, which was similar to the results of other Indian studies [4,5,6]. While these studies were focused on high-risk preterm infants, another study from Northern India evaluating rehospitalization rates in low-risk infants found that 8.3% of neonates discharged within 48 h of life required readmission, most of them (50%) for jaundice [7].
Studies conducted on safe early discharge of mother and neonates within 48 h after delivery have reported that readmission rates are higher with predominant causes being hyperbilirubinemia, feeding problems, hypernatremic dehydration and infection [8,9,10,11,12], underscoring the need for early follow-up even in term neonates, who are discharged from postnatal wards [9]. On the other hand, in high-risk preterm infants discharged from NICU, infections were found to be the leading cause of rehospitalization [4, 5, 13]. In the present study, the authors found that infections were the commonest cause of readmissions in both term and preterm neonates. Feeding problems requiring rehospitalization were more common in term neonates compared to preterm neonates. The probable explanation could be that term neonates stay for shorter duration in the hospital and end-up getting discharged before feeding is well established. A similar trend has been observed in other studies, where a shorter duration of stay in term neonates (< 72 h), is associated with more readmissions for feeding problems, probably because of discharge prior to establishment of regular breastfeeding [14,15,16,17,18].
Paul et al. concluded that male sex, vacuum-assisted delivery, gestational age < 37 wk, and length of stay < 72 h were predictors of readmission in the first 10 d of life [19]. A systematic review including 28 studies found that primiparity, Asian race, maternal comorbidities, vaginal delivery, male sex and neonatal comorbidities were the factors associated with readmission in the first month of life [8]. In the present study too, majority (58.4%) neonates readmitted were males. A shorter length of initial hospital stay has been associated with greater readmissions, in various settings [15,16,17,18]. A study amongst breastfeeding infants said that prematurity and short hospital stays were risk factors for readmission with hyperbilirubinemia, excessive weight loss and hypernatremia, whereas an initial hospital stay of ≥ 3 d was associated with a reduced risk for readmission of these infants, possibly related to establishment of breastfeeding [11]. Similarly, Jarrett and colleagues from Australia found that discharge prior to establishment of regular breastfeeding was associated with an increased incidence of readmissions among a cohort of relatively stable term infants [20]. On the contrary, Harron and colleagues didn’t find any difference in readmission rates with respect to shorter vs. longer initial hospital stays [15]. In the present study, though feeding related problems were more common among term infants, a binary multiple logistic regression analysis including initial hospital stay < 48 h, SGA status, and mode of delivery as co-variates did not show any of these factors to be associated with readmission. Readmission amongst previous NICU graduates, especially for preterm infants has been found to be common in some studies [16], with predominant risk factors being gestational age < 28 wk, birth weight < 1500 g, multiple pregnancy and mechanical ventilation [21]. It is evident that both high-risk and normal neonates need ongoing follow-up to address concerns and to ensure well-being, failing which they are likely to return to the hospital with complications like jaundice, infection or other morbidities.
Multiple interventions have been proposed to reduce readmissions in neonates. Hyperbilirubinemia guidelines and universal screening for bilirubin in term and near-term newborns has decreased the readmission rates significantly [22] and such means could be useful for our population too, as about 13.7% (n = 42) neonates were admitted with jaundice. Another study proposed that risk factors such as substantial weight loss (> 5% difference between birth and discharge) and elevated hematocrit to be taken into account in the decision to discharge neonate, owing to the risk of significant jaundice in these neonates [17]. Datar et al. noted that postpartum length of stay legislation was found to reduce the incidence of readmissions [23]. Another study from Lebanon concluded that postponing discharge until 24 h and ensuring adequate breastfeeding reduced the number of readmissions for jaundice in term and late preterm neonates [24]. Nilsson et al. observed that focused breastfeeding counseling was associated with lesser need for readmissions in early-discharge setting [25]. Many of these interventions can be easily implemented in low-middle income countries (LMICs) also, using point of care quality improvement (POCQI) initiatives. Inclusion of a comprehensive strategy comprising essential newborn care, objective breastfeeding assessment and appropriate lactation support, weight-check at discharge, recall of selected neonates based on Bhutani’s nomograms for bilirubin measurements are all some of the interventions that can be deployed. Integration of these initiatives with the existing packages like home-based neonatal (HBNC) and young child care (HBYC) will ensure participation of stakeholders from the community also.
One of the strengths of present study is inclusion of both high-risk as well as normal neonates, and large sample size. Catering to a large population, the authors believe the common reasons for readmission found in the present study will be applicable to centres elsewhere in the country as well. Being a retrospective study, there were a few limitations as well: there may be a slight over-representation of infection associated morbidities, as the present is a tertiary referral centre; readmissions occurring in hospitals other than present one weren’t accounted for; shorter visits to the emergency department not requiring hospitalization were not captured; lack of electronic database for all livebirths, precluded use of a control group, which would have ideally helped authors’ analyze other co-variates affecting readmission rates.
Conclusions
Readmissions accounted for 1.2% of all live-births and 5.9% of total NICU admissions, majority of which were neonates who had an initial uneventful postnatal course (66.2%). Infections, jaundice and feeding related issues accounted for 76% of all the re-admissions. It is important to devise follow-up plans incorporating essential newborn care, lactation support, weight-check and jaundice monitoring for low-risk term neonates to reduce repeat hospitalizations.
References
International Institute for Population Sciences (IIPS) and Ministry of Health and Family Welfare. National Family Health Survey-4 (NFHS-5), India-Factsheet. Available at: http://rchiips.org/nfhs/factsheet_NFHS-5.shtml. Accessed on 21 Mar 2024.
Jones E, Stewart F, Taylor B, Davis PG, Brown SJ. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst Rev. 2021;6:CD002958.
Bernardo J, Keiser A, Aucott S, Yanek LR, Johnson CT, Donohue P. Early readmission following NICU discharges among a national sample: associated factors and spending. Am J Perinatol. 2023;40:1437–45.
Kumar V, Anand P, Verma A, Thukral A, Sankar MJ, Agarwal R. Need for repeat-hospitalization in very low birth weight or very preterm infants: a prospective cohort study. Indian J Pediatr. 2024. https://doi.org/10.1007/s12098-023-04999-7.
Saini D, Kaur H, Prajapati M, et al. Survival rate, postdischarge readmission rate, its causes and outcomes among the preterm neonates admitted in a tertiary care centre, northern India. J Neonatol. 2022;36:6–12.
Mukhopadhyay K, Louis D, Mahajan G, Mahajan R. Longitudinal growth and post-discharge mortality and morbidity among extremely low birth weight neonates. Indian Pediatr. 2014;51:723–6.
Gupta P, Malhotra S, Singh DK, Dua T. Length of postnatal stay in healthy newborns and re-hospitalization following their early discharge. Indian J Pediatr. 2006;73:897–900.
Della PR, Huang H, Roberts PA, Porter P, Adams E, Zhou H. Risk factors associated with 31-day unplanned hospital readmission in newborns: a systematic review. Eur J Pediatr. 2023;182:1469–82.
Seki K, Iwasaki S, An H, et al. Early discharge from a neonatal intensive care unit and rates of readmission. Pediatr Int. 2011;53:7–12.
Young PC, Korgenski K, Buchi KF. Early readmission of newborns in a large health care system. Pediatrics. 2013;131:e1538–44.
Hall RT, Simon S, Smith MT. Readmission of breastfed infants in the first 2 weeks of life. J Perinatol. 2000;20:432–7.
Arora I, Juneja H, Bhandekar H, Chandankhede M. Neonatal hypernatremic dehydration in breastfed neonates: a prospective study unmasking the influences of breastfeeding practices and early weight monitoring. J Matern Fetal Neonatal Med. 2024;37:2299568.
Kuint J, Lerner-Geva L, Chodick G, Boyko V, Shalev V, Reichman B; Israel Neonatal Network. Type of re-hospitalization and association with neonatal morbidities in infants of very low birth weight. Neonatology. 2019;115:292–300.
Hannan KE, Hwang SS, Bourque SL. Readmissions among NICU graduates: who, when and why? Semin Perinatol. 2020;44:151245.
Harron K, Gilbert R, Cromwell D, Oddie S, van der Meulen J. Newborn length of stay and risk of readmission. Paediatr Perinat Epidemiol. 2017;31:221–32.
Farhat R, Rajab M. Length of postnatal hospital stay in healthy newborns and re-hospitalization following early discharge. N Am J Med Sci. 2011;3:146–51.
Blumovich A, Mangel L, Yochpaz S, Mandel D, Marom R. Risk factors for readmission for phototherapy due to jaundice in healthy newborns: a retrospective, observational study. BMC Pediatr. 2020;20:248.
Lee KS, Perlman M, Ballantyne M, Elliott I, To T. Association between duration of neonatal hospital stay and readmission rate. J Pediatr. 1995;127:758–66.
Paul IM, Lehman EB, Hollenbeak CS, Maisels MJ. Preventable newborn readmissions since passage of the newborns’ and mothers’ Health Protection Act. Pediatrics. 2006;118:2349–58.
Jarrett O, Gim D, Puusepp-Benazzouz H, Liu A, Bhurawala H. Factors contributing to neonatal readmissions to a level 4 hospital within 28 days after birth. J Paediatr Child Health. 2022;58:1251–5.
Zheng QM, Hua WZ, Zhou JX, Jiang LP. Current status of unplanned readmission of neonates within 31 days after discharge from the neonatal intensive care unit and risk factors for readmission [Article in English, Chinese]. Zhongguo Dang Dai Er Ke Za Zhi. 2022;24:314–8.
Alkalay AL, Bresee CJ, Simmons CF. Decreased neonatal jaundice readmission rate after implementing hyperbilirubinemia guidelines and universal screening for bilirubin. Clin Pediatr (Phila). 2010;49:830–3.
Datar A, Sood N. Impact of postpartum hospital-stay legislation on newborn length of stay, readmission, and mortality in California. Pediatrics. 2006;118:63–72.
Hanin EA, Rayan H, Hani T, Taleb J, Dany AH, Lama C. Breastfeeding and readmission for hyperbilirubinemia in late preterm and term infants in Beirut, Lebanon. Indian Pediatr. 2022;59:218–21.
Nilsson IMS, Strandberg-Larsen K, Knight CH, Hansen AV, Kronborg H. Focused breastfeeding counselling improves short- and long-term success in an early-discharge setting: a cluster-randomized study. Matern Child Nutr. 2017;13:e12432.
Author information
Authors and Affiliations
Contributions
DM collected and analysed the data, and wrote the initial manuscript; AM conceptualized and designed the study, supervised data collection, analysed data, and revised the manuscript. Both authors have approved the final version of the manuscript. AM shall act as the guarantor of the paper.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mandal, D., Murugesan, A. Clinical Profile of Neonates Getting Readmitted to Neonatal Intensive Care Unit (NICU) after Discharge from Hospital. Indian J Pediatr (2024). https://doi.org/10.1007/s12098-024-05236-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12098-024-05236-5